Chapter 4. Conservative dentistry, its divisions, purposes and tasks
Conservative Dentistry – part of dentistry, which studies etiology, pathogenesis, clinical manifestations, treatment and prevention of diseases of hard tooth tissues (caries and its complications, non-caries lesions), parodontium and oral mucosa, that is stomatological diseases, which are needed, in the first place, conservative, therapeutic treatment.
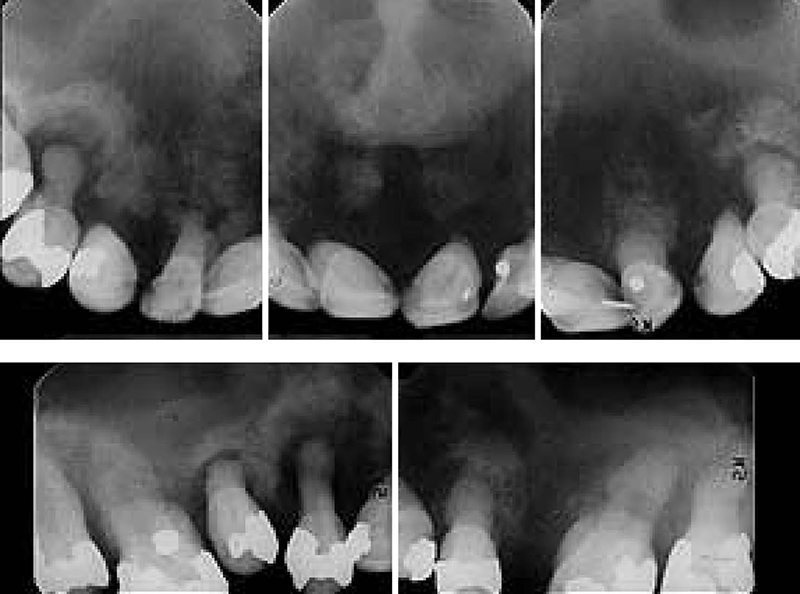
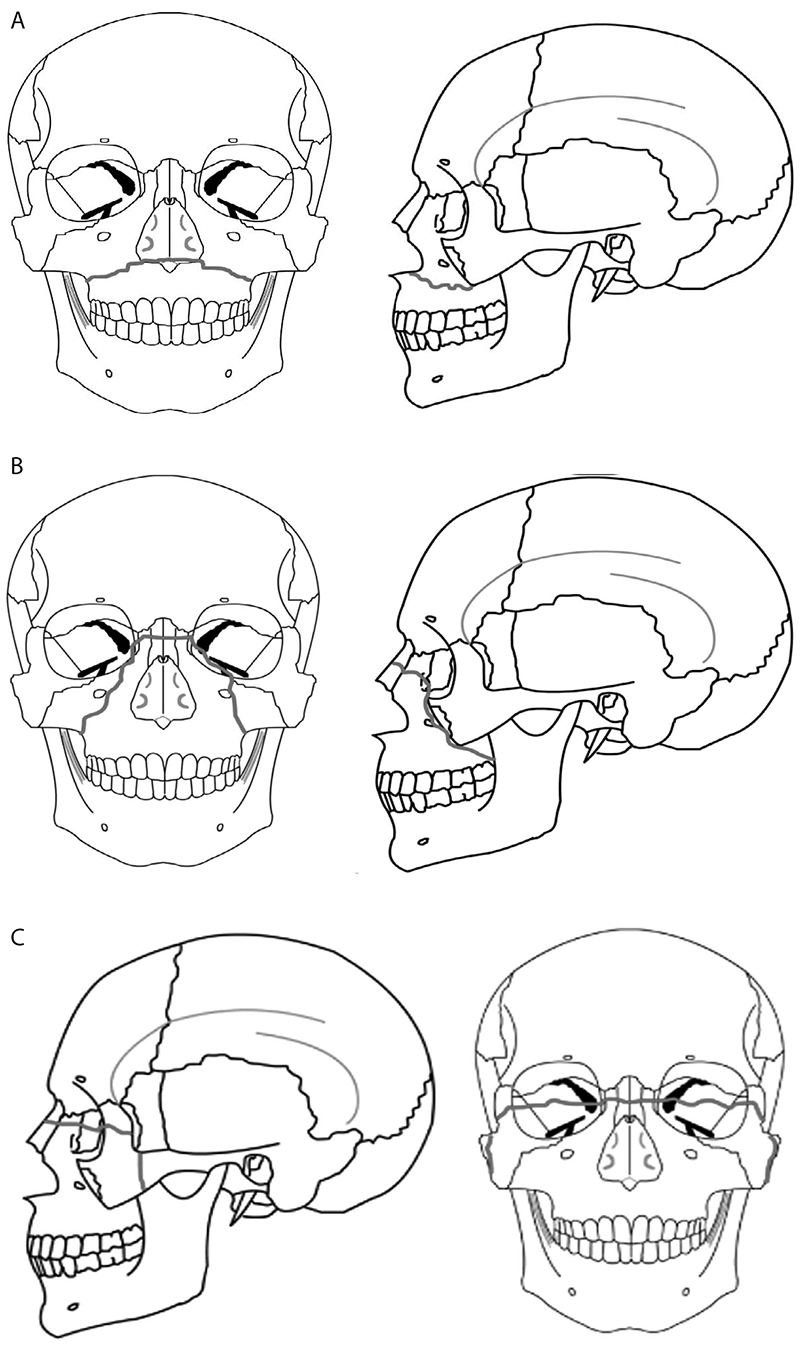
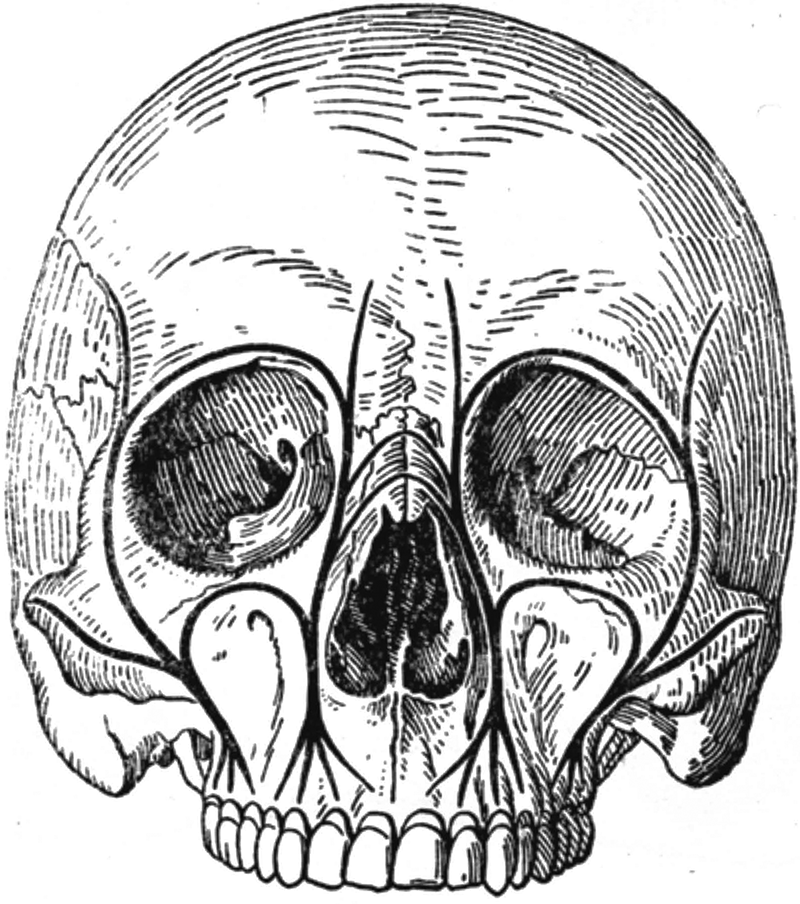
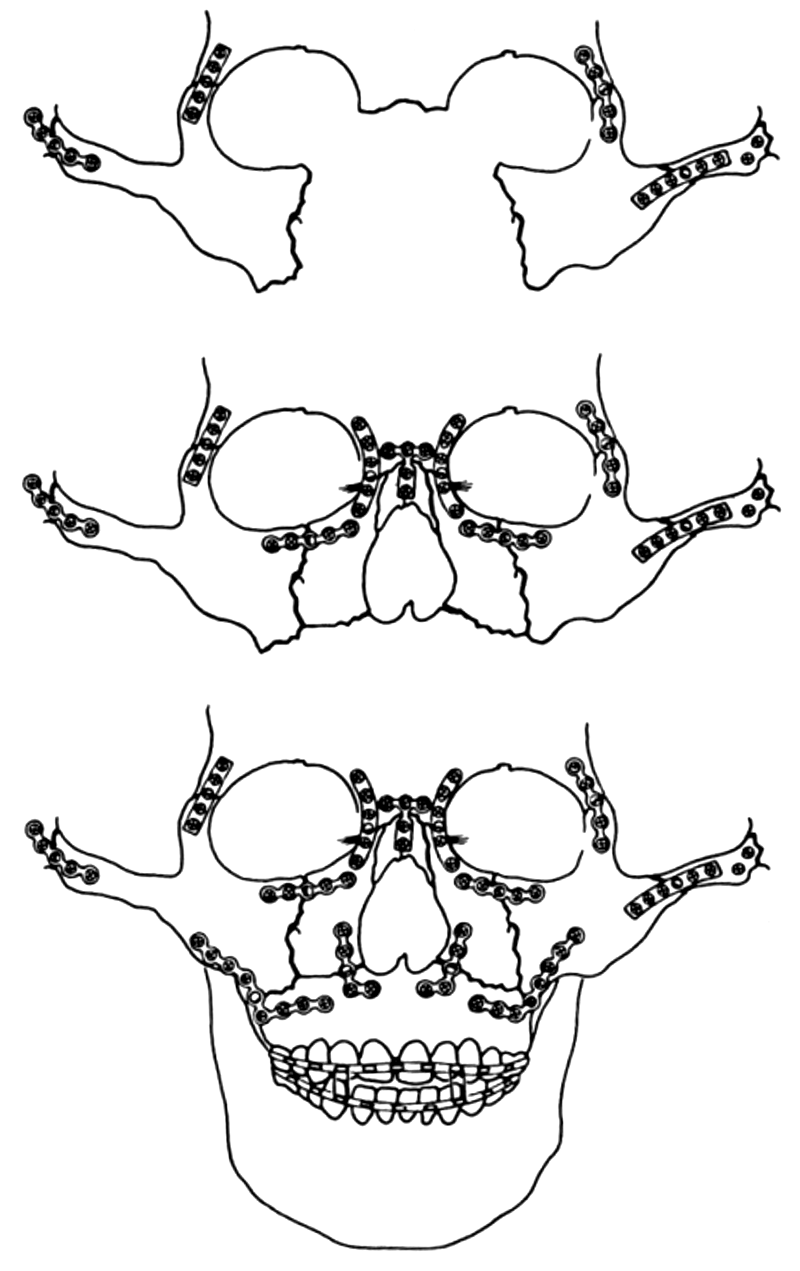
Schema 1

Schema 2

Schema 3

Schema 4

Chapter 5. Noncarious lesions, which appear after the eruption of teeth
Abrasion of the hard teeth tissues
Teeth are obliterated not only by the contact of occlusal surfaces of teeth-antagonists, but also in the section of interdental contact points. As a result of elasticity of the collagenic fibers of periodontium teeth insignificantly move along each other, which is called the physiological mobility (amplitude of 0,1–0,2 mm). In this regard, with age as a result of abrasion the planar contact appears between teeth instead of the point one.
Physiological abrasion is observed both in temporary and in permanent occlusion, for example: temporary and permanent incisors erupt with serrations, which obliterate quite rapidly. In temporary teeth the process of abrasion is more expressed and it barely depends on character of food. When biting and chewing food the abrasion and grinding of the occlusal surfaces of dental crowns occur. The smooth polished areas (facets), whose arrangement depends on the form of occlusion, are forming in superficial layer of enamel.
The degree of physiological abrasion of teeth has risen with the age.
Pathologic abrasion of teeth is the state of their increased abrasion, when the atypical contact areas, surrounded by the sharp edges of the preserved enamel, are formed in the tooth or teeth in a short time. In this case the teeth lose their anatomical form, interrelation in dentitions changes, occlusion reduces and dentitions cannot carry the functional load without subsequent damage of hard tissues.
Clinical picture of pathologic abrasion
Complaints:
- To the increased sensitivity to the temperature stimuli.
- With the deepening of process pain from chemical stimuli can be joined, and then – from mechanical stimuli.
- Subsequently, as a result of intensive postponement of replacing dentine, the increased sensitivity can decrease or disappear.
- In spite of the significant abrasion, in most people the sensitivity of pulp remains or decreases insignificantly.
Objectively:
- Abrasion manifests as disappearance of the cusps of occlusal surface, cutting edges of frontal teeth visually.
- Specific grinding in occlusal surfaces and cutting edges of teeth-antagonists occur.
- Characteristic, smoothly polished, bright surfaces of abrasion (facets), surrounded by protruding sharp edges of enamel are formed. The surfaces of abrasion are different and they depend on the form of occlusion, influence of exogenous and endogenous factors, influence of local mechanical factors.
- Once the enamel is lost completely, considerably process of abrasion of dentine accelerates, which leads to the formation of sharp edges and changes of the anatomical form of teeth. The hard tissues of dental crowns can obliterate almost to the level of gums in the neglected cases of pathologic abrasion.
- With generalized abrasion the lower part of face decreases and occlusion reduces sharply, that causes the disease of temporal-mandibular joint, periodontium and reduction of effectiveness of the chewing of food.
- Surfaces are damaged with caries very rarely, which is explained with the loss of retentional points for the delay of food and microorganisms.
Treatment of pathologic abrasion consists in:
- Elimination of etiological factors.
- Elimination of hyperesthesia.
- Polishing sharp edges of teeth and filling defects.
- Prosthetic treatment to eliminate separate defects and to increase the height of occlusion with fixed or removable denture.
Wedge-shaped defect
It is localized in precervical section. It has the form of the wedge, whose edge is directed toward the cavity of dental crown.
Clinical picture of wedge-shaped defect
Complaints:
- Complaints cannot appear at the initial stages of development of the wedge-shaped defect.
- The sensation of pain or the increased sensitivity from acid, sweet, cold and hot appear with the recession, at the last stages – aesthetical defect.
- Complaints have not been ever, because the slow development of process conduce to deposition of tertiary dentine, but pulp gradually atrophies.
- As a rule, complaints disappear with an even bigger recession of defect, in this case the cavity of tooth is obliterated and it looks as dark point.
- The subsequent progress of defect can lead to the fracture of crown. Rarely defect is complicated with caries.
Objectively: at the early stages of its development wedge-shaped defect does not have a form of wedge, but superficial scratches or thin fissures, or slots are revealed. Then these recesses begin to widen and, reaching certain depth, more and more they acquire the form of a wedge.
Both walls are smooth, shining, polished, unconverted in colour.
Defects are localized on the vestibular surfaces predominantly and very rare – on lingual (palatine). They can be single, but more often – multiple and they are placed on the symmetrical teeth, they develop very slowly.
Treatment of wedge-shaped defect
The general treatment provides for prescription the microelements and vitamins for the purpose of strengthening of structure of teeth internally and the removal of hyperesthesia.
The wedge-shaped defects, whose depth exceeds 2 mm, must be filled (before this course of remineralized therapy is prescribed).
In certain cases, in danger of destruction of the tooth crown the tooth is covered with an artificial crown.
Erosion of hard teeth tissues
This is the progressive loss of hard teeth tissues (enamel or dentine) with unexplained etiology. In contrast to the carious lesions, the appearance of erosion is not related to the influence of microorganisms.
Clinical picture. Erosions are localized on the symmetrical surfaces of central and lateral incisors of upper jaw, and also on canines and premolars of both jaws, they does not occur on incisors and molar of the lower jaw. As a rule, there are no single lesions, usually two and more symmetrically placed teeth are involved.
Since the beginning of development erosion looks as defect of oval form, which is placed in the transverse direction on the most convex part of vestibular surface of crown. The bottom of erosion is smooth, shining, solid. A constant recession and the expansion of the limits of erosion lead to the loss of entire enamel on the vestibular surface of tooth and part of the dentine.
Subjectively. Pains appear rarely or expressed weakly. This is connected with the slow development of process, as a result of which occurs the postponement of replacing dentine. The pains can appear from all forms of stimuli – temperature, chemical and mechanical with increasing depth of lesion. The periods of appearance of pain (active phase) alternate with their absence (stopped erosion).
Treatment of the erosions of hard tissues. It is necessary to take into account the activity of process and character of the associated somatic disease (which is treated by a specialist).
Necrosis of hard teeth tissues
This is unique noncarious lesion, which is developed under the influence of some unmicrobal external factors (acids, ionizing emission), it is characterized with the progressive and irreversible destruction of hard teeth tissues and can to lead to total loss of teeth.
Necrosis is caused by both exogenous and endogenous (disturbance of the activity of endocrine glands, diseases of central nervous system, chronic intoxication of organism) factors. Types of necrosis are: precervical and chemical necrosis.
Acidic (chemical) necrosis appears in people, who work in the manufacturing mostly of inorganic acids, which evaporate and fall into the saliva. In this case the saliva acquires acid reaction and decalcifies the hard teeth tissues. This lesion is possible, but in the mild form, when using 10 % of hydrochloric acid with achylic gastritis. Oral respiration favours to the appearance of acidic necrosis.
At acidic necrosis, at first, frontal teeth are affected, enamel begins to disappear from the cutting edge, and then process passes to the vestibular surface. At first, teeth become matted, then – dull gray, sometimes yellow or brown. The dental crowns become shorter, the cutting edge acquires oval form. Gradually the crowns of front teeth become destroyed to gingival edge, and premolars and molars erase badly.
Typical complaints in patients appear already at the initial stages: the sensations of numbness and soreness in the teeth, the sensation of adhesion of teeth with occlusal contact appear. The phenomena of hyperesthesia can appear. If replacing dentine manages to form, then painful sensation subside.
Treatment consists in:
- elimination of the reason for the acidic necrosis (with hydrochloric acid must drink through the straw);
- remineralizing therapy with the preparations of calcium and fluorine;
- alkaline gargles.
Hyperesthesia of hard teeth tissues
Hyperestesia is the increased painful sensitivity of the hard teeth tissues in response to the action even of insignificant temperature, chemical and mechanical stimuli, which rapidly disappears. Usually these phenomena are constant, but sometimes temporary calming or curtailment of pain (remission) can observe. Sometimes pain can radiate to the adjacent teeth. More often this phenomenon is observed with the pathology of the hard tooth tissues of noncarious origin, and also with the caries and the diseases of periodontium.
Hyperesthesia can be:
- local (it appears from the action of local stimuli);
- systemic or generalized, which appears with neural and mental diseases (psychoneuroses), endocrinopathies, metabolic disturbances, diseases of digestive canal, climax, infectious diseases.
The most important is local treatment of hyperesthesia. These groups of medicines can be used for treatment:
- Cauter medicines.
- Medicines with dehydrating action.
- Medicines with biological action.
- Anesthetics and analgesics.
- Adhesive systems of light-cured composite materials.
Clinical efficiency and complications for home methods of tooth bleaching, dental treatments and preventive measures:

Methods of elimination of external colouring of teeth:
- Microabrasion:
- Removal of a superficial layer of enamel.
- Smoothing of enamel.
- Light reflexion.
- Bleaching.
- Clarification of enamel – (without destroying enamel structure):
- Professional cleaning.
- Sanitation.
- Individual hygiene of oral cavity.
- Bleaching:
- The bleaching agent penetrates into enamel.
- Discharge of О2.
- Oxidation of organic substances, which colouring teeth.
- Denaturation of proteins entering into a pigment.
- Tooth clarification.
Classification of dental bleaching:
- Professional office (surgery) bleaching systems.
- Professional home bleaching systems.
- Home means:
- Teeth bleaching pastes.
- Rinses.
- Chewing gums.
- Bleaching sticks, pencils, varnishes, gels.
Types of bleaching substances
The 1st group – Contains acids.
The 2nd group – Substances discharging oxygen.
The 3rd group – Physical factors intensifying action of the bleaching substances: laser, ultraviolet rays, heat, halogen light.
The 4th group – Combined.
Chapter 6. Dental caries
Dental caries (tooth decay) and periodontal disease are probably the most common chronic diseases in the world. Although caries has been affected humans since prehistoric times, the prevalence of this disease has greatly increased in modern times on a worldwide basis, an increase strongly associated with dietary change. However, evidence now indicates that this trend peaked and began to decline in many countries in the late 1970s and early 1980s, and the decline was most notable in certain segments of the population of the United States and Western Europe. The decline in caries in developed countries such as the United States has been most prominent in the upper and middle classes, while the lower socioeconomic classes and rural residents have retained a higher prevalence of tooth decay.
A dental caries (caries dentis, from Latin – caries – decay) is a pathological process which manifests as demineralization and destruction of hard tooth tissues forming carious cavity. Dental caries is an infectious microbiologic disease of the teeth that results in localized dissolution and destruction of the hard tooth calcified tissues.
As a human disease caries is known from deep antiquity, possible information about this illness appeared in hand-written manuscripts already near a 3000 year B. C. An examination of prehistoric crania found in various museums indicated that the percentage of carious teeth ranged from 2 to 7 %. At that time caries yet was not enough widespread illness, but in more late epoch (Middle Ages) its prevalence began to increase. It links with the nutritional changes of people, environmental conditions and mode of life. By the year 1850 there was a rapid dietary change in the direction of increasing consumption of sugar and milled wheat products by all segments of the population. In the XIX century, caries experience in England increased rapidly after 1850. Since the XVII century, caries prevalence increase sharply and in XX century its prevalence in some regions of world is nearly 100 %. Now there are different levels of caries prevalence from 1–3 % in the countries of Western Europe to 80–97 % in the countries of Africa, Asia and former Soviet Union. It is explained by alongside factors: the character of nutrition (above all things excess of carbohydrates in food (sugar and milled wheat products) and relative lack of proteins in the nutritional ration), low concentration of fluoride and other macro-, microelements in drinking-water, social and climate conditions.
In epidemiology studies of estimation of the state of teeth some indexes were used: caries prevalence, intensity, morbidity (increase of intensity for a period of time). The number of individuals in a population having a disease at a particular point in time is known as the prevalence of disease.
Caries prevalence (latitude) is calculated by dividing the number of persons who have caries lesion, filled and extracted teeth (regardless of the number of carious teeth in each of them) by the total number of inspected persons and is expressed in percentages:

The number of persons with new cases of a disease in a population over a given period of time, usually 1 year, is the incidence of the disease.
The most common epidemiologic measure of caries is evaluation of the number of permanent teeth that are diseased, missing, or filled (DMF). Measures of primary teeth are also reported as DMF. DMF may be reported as the number of teeth (DMFT) or surfaces affected (DMFS). This measure is cumulative because it totals the number of restorations and extractions in addition to the number of teeth having active caries.
The index of DMF of teeth is the number of caries – diseased tooth (D), filling (F) and missing because of complications of caries (M) in one inspected person. In determination of this and other mean values of indexes of intensity in a significant number of people their sum divides by the number of inspected people. During determining the index of DMF a tooth which has one or a few carious cavities is considered as decayed or diseased (D), filling – one or a few filling cavities, regardless of their size and condition. If in a tooth there is simultaneously filling and carious cavity, it is considered as caries. In children this index is calculated depending on occlusion: in permanent occlusion there are permanent teeth measured by caries (index of DMF); in primary (milk) teeth – index of df (decay and filling) and in adolescence measured both permanent and primary teeth – DMF + df.
The general condition of human organism, in particular, past and concomitant systemic diseases have a definite influence on intensity of caries. There is higher prevalence of caries in children carrying infectious and systemic diseases. The general changes in immunological reactivity of organism made a considerable influence on caries development.
The status of oral hygiene and quality of teeth brushing is one of important factors in caries development. The regular care of teeth with the use of modern prophylactic and hygienic measures is a very effective method of caries prophylaxis. Up to a point, uneven cleaning of different teeth is expressed in frequency of caries development in separate teeth. Very often caries develops in teeth with very complicated anatomical form of crowns with plenty of pits and fissures.
On the basis of overall caries patterns permanent teeth can be grouped according to their susceptibility to caries, from the most to the least susceptible, as follows:
- Lower first and second molars, upper first molars
- Upper second molars.
- Upper premolars.
- Upper incisors.
- Upper canines.
- Lower premolars.
- Lower incisors.
- Lower canines.
Theories of the dental caries
Dental caries is the best known and most widespread human diseases. In spite of successes attained lately in caries prophylaxis and medical treatment in the countries of Western Europe and North America caries remains the most widespread disease.
The problem of caries development interested many researchers since ancient times. Depending on the degree of development of science and medicine different theories of caries development were presented. Therefore no wonder that to the present time a lot of different conceptions of caries were proposed.
Modern conceptions of caries development
The interaction of three main factors is essential for the initiation and progression of caries: a susceptible host tissue, the tooth; microflora with a cariogenic potential; and a suitable local substrate to meet the requirements of the pathodontic flora. The tooth is the target tissue destroyed in the dental caries process. The cariogenic oral flora, localized on specific sites of teeth, is the agent that produces and secretes the chemical substances (organic acids, chelating agents and proteolytic enzymes) that cause the destruction of the inorganic components and the subsequent breakdown of the organic moieties of enamel and dentin. The local substrate provides the nutritional and energy requirement for the oral microflora, thereby permitting them to colonize, grow, and metabolize on selective surfaces of teeth. The third factor – resistance of the tooth – is obviously important since it determines the overall effect of the attack.
According to the modern conceptions of caries development (E. V. Borovsky et al., 1979, 1982) there are few groups of cariogenic factors. There are factors of systemic character, local and related to resistance of hard tooth tissues. To systemic factors belong non sufficient diet and drinking-water (the especially low contents of fluoride in water), systemic diseases and disorders, extreme unfavorable influences. Local factors are the dental plaques, microflora, disturbance of saliva composition and properties, carbohydrate food debris. Disturbances of resistance of dental hard tooth tissues are related to their inferior structure, defects of chemical composition, unfavorable genetic code (by the hereditary propensity of hard tooth tissues to the caries). It is needed to mean that the separately taken cariogenic factor or their group, affecting a tooth, made it susceptible to influence of direct cariogenic factors (acids), creating, thus, a cariogenic situation. However, only cooperation of different groups of cariogenic factors creates favourable conditions for caries development.
Groups of cariogenic factors
| Systemic cariogenic factors |
Local cariogenic factors: |
Disturbance of tooth tissues resistance: |
| Non sufficient diet and drinking water |
Dental plaques |
Defects of structure |
| Systemic diseases and systemic disorders |
Microflora |
Defects of chemical composition |
| Extreme unfavorable influences |
Disturbances of properties and composition of saliva |
Unfavorable genetic code |
| – |
Carbohydrate food rests |
– |
The systemic cariogenic factors
Non sufficient diet and drinking water. Development, forming and subsequent existence of teeth to a great extent rely on the nutrition of man, disturbance of which results in development of diseases, including dental caries. The most credible cariogenic action is made because of excess of carbohydrates in food, deficiency of mineral salts and microelements in it, soft consistency of food. By numerous clinical investigations in people which ingested many of carbohydrates in diet the considerable prevalence of caries was revealed. Especially it was expressed in the use of sucrose and glucose. They render the most unfavorable action in children, when hard tooth tissues are yet not completely mineralized.
Cariogenic action of excess of di- and monosaccharides in the diet was confirmed as a whole alongside with experiments of caries modeling in animals. It was revealed, that the greatest carogenic effect was rendered by sucrose, to a lesser extent – glucose and then other carbohydrates. Cariogenic action of carbohydrates is more evident at their direct contact with hard tooth tissues in the oral cavity.
Systemic diseases, disorders and concomitant diseases creating a favorable background for caries development. Numerous investigations showed that people with most systemic diseases are accompanied by considerable prevalence and intensity of caries. Different degrees of caries prevalence relies on influence of systemic diseases on the common state of organism and their duration. It is impossible to consider that common diseases directly affect hard tooth tissues, they rather affect them indirectly by means of changes of composition of saliva, rate of saliva flow or through pulp. In some measure this influence is possible by means of change in composition of microflora and hygienic status of the oral cavity. The most unfavorable influence of common diseases on teeth is indicated during their development, mineralization and eruption. In children of different ages with concomitant diseases of internal organs, dental caries develops especially often and is characterized by the acute coarse and numerous lesions of teeth. Thus, these diseases create a background on which unfavorable local cariogenic factors will be easily realized.
Among unfavorable extreme influences on human organism the most damaging action on teeth is rendered by ionizing radiation. It violates activity of salivary glands of oral cavity, diminishes the rate of saliva flow, large amount of dental debris – substantia alba – accumulates on teeth (G. M. Barer, 1972). In future spots of enamel demineralization and destruction develop on these places. Direct damaging action of ionizing radiation, directly on hard tooth tissues, is also revealed.
Local cariogenic factors made direct damaging action on hard tooth tissues. Most cariogenic action both independently and in combination with other factors had dental deposits: dental debris and dental plaques. Dental deposit is rather yellow or grayish-white soft and sticky deposition on the surface of teeth, which is a conglomerate of microorganisms, cells of desquamate epithelium, leucocytes, mixture of proteins and lipids of saliva with the particles of food. Soft dental debris has no permanent inner structure, it is not tightly attached to the enamel surface, thus it can be easily washed off by stream of water or taken off by a cotton pellet. A gelatinous mass of bacteria adhering to the tooth surface is termed dental plaque. Dental plaque is a soft amorphous granular deposit, which is enough tightly attached to the tooth surface, from which it can be removed only by mechanical cleaning with a special instrument or tooth brush. When plaque is small in size it cannot be revealed (if not colored by means of food dyes and coloring agents), in large amounts the mass on the tooth surface becomes grayish or yellow-grey.
Formation of acids in dental debris (dental plaque) and decline of pH takes occur only when carbohydrates enter oral cavity. The microorganisms of plaque fermente sucrose, glucose and fructose easier. The cellular elements of plaque together with protein agglutinative elements provide its porous structure which can pass through itself oral fluid (saliva, food liquids). The microorganisms form extracellular polysaccharides which clog intercellular spaces with plaque and thus promote the accumulation of organic acids in it. Most easily carbohydrates (sucrose, glucose) penetrate in dental plaque, which are revealed in it in the amount directly proportional to their concentration in saliva and duration of application. Simultaneously the plaque prevents the penetration of alkaline components of saliva buffer system, which can neutralize acids. In the abcence of carbohydrates the level of plaque pH usually ranges close to neutral – 7.0. Entering oral cavity carbohydrates cause sharp increase in acidity of plaque, which lasts about 30 minutes reaching the maximum of pH to 5.8–4.5.
After this the saliva buffer systems neutralize the acidic environment in plaque and its pH subsides to the neutral level again. During repeated entering of sucrose enough persistent decline in pH under the dental plaque occurs, this leads to damage of dental enamel.
Dissolution of dental enamel begins when pH = 5.5 therefore this pH level is called critical. Under the plaque the increase in acidity might be more significant. In addition plaque prevents the penetration into the enamel of alkaline components of saliva buffer system, which can neutralize acids and inorganic matters, that constantly enter the enamel with saliva, restoring its mineral structure.
Role of microorganisms in caries development. The considerable role of microorganisms in caries development was confirmed by works of W. Miller.
The highest cariogenic activity was revealed among streptococci, especially Str. mutans. This species of streptococci causes in animals the most rapid caries development with a plenty (to 75 %) of affected teeth. Today the properties of this species of streptococci are studied in great detail and its exceptional role in caries development is shown.
The ability of this species of streptococci to adhesion on the dental surface due to the synthesis extra cell polymers, such as, for example, dextrans. It is necessary to emphasize that other types of cariogenic microorganisms are able to synthesize such polymers of sugars (especially sucrose which enters oral cavity). Such polymers give a possibility to other cariogenic bacteria to be glued to hard tooth tissues (enamel), thus forming a dental plaque matrix.
In carious cavities and saliva in patients with dental caries lots of lactobacilli were revealed. These bacteria have very high acidophilic properties and power to cause caries development in experimental animals. In people with active caries higher contents of lactobacilli in saliva, in comparison with healthy persons, are revealed. On the basis of determining the amount of acidophilic bacteria in saliva a test was developed, the so-called streptococcus or lactobacilli test, which is an indicator of caries activity or susceptibility to caries development.
Acidophilic actinomyces species have a definite role in caries development. They are also selected from carious cavities. The highest cariogenic activity was shown in two kinds of actinomyces species – Actinomyces viscosus and Actinomyces muslundii – in experimental study of actinomyces species in gnotobiotic animal. Actinomyces species take a significant part in dental plaque matrix formation.
In case of appropriate conditions the microorganisms of dental plaque actively ferment carbohydrates, producing acids. Under the influence of cariogenic factors on tooth enamel the processes of demineralization and depolymerization of organic matters occur, as a result appears a caries lesion. A number of anticariogenic factors prevents the action of cariogenic factors: antimicrobial systems of saliva, presence of microelements (especially fluoride) in diet, high buffer capacity of saliva, presence of inhibitors of proteolytic enzymes, intensity of processes of enamel remineralization and its high caries resistance, strengthening of trophic function of pulp and rise of organism resistance.
In studying disease, primary factors (prerequisites), without which the disease process cannot develop, are often not clearly distinguished from secondary or predisposing factors which control the rate of disease progression. Many secondary factors, such as salivary composition and its flow rate, oral hygiene and diet influence the caries process. Secondary factors affect one or several of the following: increase or reduce the tooth (host) resistance to dental caries; increase or decrease the quantitative and qualitative nature of the oral microflora involved in dental caries; increase or reduce the cariogenicity of the local substrate.
Disturbances of properties and composition of saliva. Saliva plays an important role in providing the physiological balance of processes of mineralization and demineralization in dental enamel. With this function the tooth mineralization, “maturation” of enamel after tooth eruption is carried out, optimum composition of enamel and its remineralization after the damage or disease are supported. Saliva has the protective function of organs of oral cavity from damaging action of factors of external environment and cleansing function, which consists of permanent mechanical and chemical cleansing the oral cavity from food debris, microorganisms, etc.
The saliva reaction (pH) influences on the degree of saliva hydroxyapatite supersaturating: with reduction of pH it sharply goes down. Supersaturating of oral liquid remains only to pH 6.0–6.2 (critical level of pH), and with further acidification it slumps and saliva becomes unsaturated with hydroxyapatite. Usually the reaction of oral fluid lies within the limits of pH 6.5–7.5 and on average it is 7.2, therefore it is neutral or low alkali. Saliva contains a very power buffer system with big capacity. It allows to support the neutral reaction of environment of oral cavity constantly. Therefore the decline in saliva pH, lower than the critical value 6.2–6.0, is marked only locally: in dental debris and under dental plaque. The decline of saliva pH is marked after entering oral cavity by carbohydrates. Reduction of secretion of saliva (hyposalivation) or almost complete cessation of its flow (xerostomia) is accompanied by decline of pH and sharp increase of caries development.
The use of carbohydrates with food causes hyperglycemia, hyposalivation, increase of saliva oxygen absorption and saliva P/Ca coefficient. In people which use a plenty of carbohydrates such changes in saliva occur during practically all day long. Carbohydrates stimulate acidogenic activity of microorganisms in oral cavity (“metabolic explosion”) because of what the quantity of organic acids in saliva significantly increase – in 4-5 times – in comparison with normal condition. All these changes promote in such persons susceptibility to caries which is often numerous and active.
Food debris, accumulated on teeth and in interdental spaces, have pronounced cariogenic effect. Staying saved in retention areas for a long time, they become a breeding ground and material of which microorganisms can produce acids. The most essential value had carbohydrates, especially sucrose and glucose. Carbohydrate food debris can easy transform not only in acids, but also in dextrans, levans, which play a considerable role in forming dental plaque and its attachment to the teeth surface. The sufficient thickness of food debris also prevents the penetration of components of saliva buffer system through them, that additionally creates conditions for accumulation of acids under them.
Defective structure and resistance of hard tooth tissues
Defective structure of hard tooth tissues. An independent factor, which influences on teeth susceptibility or resistance to caries, differs in disturbance of hard tooth tissues structure. This can be the definite peculiarities of chemical composition of enamel apatites, presence of different substitutions in the crystals of apatites, correlations of different inorganic ingredients in its molecule, violations of the P/Ca coefficient. Rightness, regularity of enamel structure of protein matrix and its properties, ability for polymerization and connections of calcium and phosphorus, its co-operation with inorganic phase of enamel have great value. Presence or absence of defects in enamel structure, its density, regularity of structure, size and number of structural violations, density of crystals and rods packing, presence of tufts and lamella and their location, degree of enamel structure maturity and their saturation with calcium, phosphate and fluoride influence on caries resistance at tissular level.
Tooth chemical composition connects with its structure very tightly and has almost the same value in caries development. For example, high mineral concentration determines high density of enamel structure which determines its resistance to caries development. Caries resistance areas have higher contents of fluoride, molybdenum, strontium, selenium, phosphorus and vice versa caries-susceptible areas have lesser. Disturbance of biochemical composition of hard tooth tissues and metabolic processes, that determine caries-susceptibility, can be realized in a caries lesion only in cooperation with other cariogenic factors.
A certain place among cariogenic factors is occupied by unfavorable genetic code that is heredity. It is known, that there is a definite hereditary susceptibility to caries development, although other authors explain it by similarity of food characters. However application of modern methods of genetic analysis allows to reveal a lot (to 16) of genes which are responsible for caries development (C. Chain, 1968). It was supposed that genetic susceptibility to caries development will be realized, mostly, through proper structural features of hard tooth tissues, chemical composition of saliva, some features of metabolic processes in organism.
The above-mentioned cariogenic factors (both general and local) can be expressed in other degree. Caries development is possible at enough different variants of their co-operation, for example, at strong disturbance of tooth structure, small diet violations and a little amount of acidophilic microorganisms in oral cavity are enough to cause dental caries. Thus, under appropriate conditions the cooperation of cariogenic factors becomes possible and as a result caries develops.
Classification of caries
Clinical features of caries are enough various: from a chalky white spot on the surface of enamel to an expressed destruction of hard tooth tissues. These numerous forms of caries, per se, are stages of tooth destruction changing each other consistently (if untreated). The progress of caries process leads to destruction of entire thickness of hard tooth tissues, perforation of pulp chamber and development of inflammation of pulp (pulpitis) or periodontal ligament (apical periodontitis). Therefore pulpitis and apical periodontitis, another tissues of maxillo-facial region, which arise because of caries process, are called caries complications.
Depending on the depth of caries lesion of enamel and dentine, caries is divided into superficial, middle and deep. Depending on the caries course, acute (rampant) and chronic caries are distinguished.
Incipient caries (caries incipience). A characteristic feature is development of demineralization on the enamel surface. As a result incipient white spot lesions and stained, roughened, partially remineralized incipient lesions of enamel develop. A carious cavity in enamel is forming.
Superficial caries (caries superficialis) – there is a carious defect in enamel, dentino-enamel junction is not destroyed by caries process.
Middle caries (caries media) – carious cavity in dentin is formed: in mantle dentin. This layer of dentin is juxtaposed with enamel and converted into the initial layer of dentin from the basement membrane.
Deep caries (caries profunda) – carious cavity in mantle dentin is formed: in circumpulpal dentin. This layer of dentin is localized very close to pulp. The carious cavity can divide from the pulp chamber only very thin partition or only the layer of secondary dentin.
Clinical feature of caries
Incipient caries. Patients complain of spots (white, chalky white, opaque or pigmented), rarely of feeling insignificant sensitiveness, sorenesses of the mouth from different irritants, mainly chemical (sour, sweet).
In the acute (rampant) course on the limited areas of dental enamel the opaque, deprived of natural transparency, chalky white spots appear. At first, spots are small, but, gradually increase in size. They are often located on occlusal surfaces in retentive points: pits and fissures of occlusal surfaces of teeth, cervical areas. In children they are often localized on a vestibular surface and cervical areas. For the best revealing of caries spots it is recommended to remove debris from the spot surface and dry up the tooth crown: intact enamel saves its natural transparency and brilliance, while the surface of caries spot loses transparency and becomes opaque. When probing a roughness, insignificant pliability and painfulness of their surface can be revealed.
The histological features at an initial caries are characterized by development of different degrees of enamel demineralization. In enamel section the body of caries lesion has the form of of a triangle with the basis directed to enamel surface. In the study in the polarized light depending on the structure changes in enamel lesion a few areas are distinguished. The most demineralized is subsuperficial lesion layer, which is covered with mineralized superficial enamel layer. This interesting phenomenon is explained by remineralization processes of carious lesion by the mineral components of saliva. If oral fluid is unable to provide remineralization of the demineralized enamel area, rapid development of caries lesion occurs.
Superficial caries. In some period of time in the center of carious spot the superficial layer of enamel loses the integrity and defect appears in enamel. At acute superficial caries patients complains of insignificant pain, more frequent of feeling soreness of the mouth and affected tooth, caused by chemical irritants, which at once disappear after cessation of irritant actions. Sometimes shot-term pain from thermal and mechanical irritants occur, more often in place of localization of carious lesion.
At the examination of tooth in the area of chalky white color a lesion of a shallow enamel defect (cavity) is determined, placed within the enamel borders. The enamel wall with lesion is softened, yellow-grey and a little sensible when probing. Sometimes it can be only rough surface, but after removing the softened enamel surface the lesion (cavity) is found.
The chronic superficial caries course is mainly painless. Insignificant pain from chemical irritants rarely occurs. But it disappears immediately after cessation of irritant action. A small enamel lesion (cavity) with enough dense yellow-brown or brown enamel walls is revealed on the enamel surface. The cavity has a wide, exposed inlet without overhanging margins. Probing of carious defect is practically painless. When superficial caries is localized in fissures the margins of lesions remain undamaged.
Superficial caries is diagnosed on such grounds: a) patient’ complaints about short-term painful feeling mainly from chemical irritants; pain disappears after cessation of irritant action; b) revealing of shallow carious cavity, located within enamel borders, or of fissures pigmentation on occlusal surface, in which the softened demineralized enamel is revealed when probing; c) painful preparation of hard tooth tissues especially at the dentinoenamel junction.
Middle caries (caries media). After destruction during the pathological process of dentinoenamel junction caries quickly begins to spread to the dentine. Middle caries (caries media) is pathological condition, when a carious cavity is located in mantle dentin. Patients with acute middle caries often complain about painful feeling. More often the pain has weak intensity and appears only under the action of irritants: chemical, thermal, mechanical. On the tooth surface there is a chalky white carious spot with the enamel defect in a center. Examination of the cavity is difficult because of its narrow inlet. The cavity usually has a depth of 1,5–2 mm, it is filled with food debris and softened dentin. Complete examination of carious cavity is possible only after removing of overhanging chalky white enamel margins with special instruments (burs, excavators). The cavity is wider near the dentinoenamel junction and it is narrowing towards the pulp gradually. The softened dentine which covers the cavity, is grey-white or yellow, rarely – pigmented. The degree of dentine softening depends on the activity of caries process: at acute (rampant) caries the hard tooth tissues are more softened like a cartilage, at chronic course it can be harder and pigmented. Probing of carious cavity is practically painless except the dentinoenamel junction.
Chronic middle caries has practically little clinical symptoms. In some cases weak pain can occur because of action of chemical, rarely thermal and mechanical irritants and it disappears at once after their cessation. When examining the carious cavity a rather wide inlet is revealed, it is located in mantle dentin, the depth of cavity is 1,5–2 mm depending on the surface of the tooth. The carious cavity is covered with rather dense pigmented dentin, floor and walls of the cavity are painless when probing. During electric pulp testing (electroodontodiagnostic method) the pulp reacts on the current strength of 6–12 mcA.
Deep caries (caries profunda). It is characterized by formation of carious cavity which affected almost all layers of dentine practically to pulp and it is located in circumpulpal dentin. Patients with acute deep caries complain about causal pain which appears because of action of thermal, mechanical, chemical irritants and disappears after their cessation. Inserting into the carious cavity of cotton tampon with hot (no more than 50 ºC) or cold water, and also ether is usually accompanied by sharp pain reaction, however, pain disappears after the removal of irritants from the cavity. Carious cavity is located within the limits of circumpulpal dentin with the overhanging margins of enamel. Enamel around the inlet has softened chalky white color. The carious cavity is filled with grey-whitish or yellow softened dentin. When probing a painful area on the cavity floor and dentinoenamel junction is revealed. Often it is the places of projection of pulp horns, which directly react on irritants; however, perforation of carious cavity is not observed. At acute deep caries, probing of caries cavity floor must be made very carefully. At the points of pulp horns projection the dentinal wall is very thin, the dentine is softened and can be easily pierced with a probe and injure pulp. It is accompanied by sharp pain and a blood drop appears in the carious cavity.
At the chronic deep caries there can be no complaints of pain, while insignificant, brief pain after thermal, chemical and mechanical irritants can be revealed. Defect of hard tooth tissues is located in limits of circumpulpal dentin, rather large in size, occupies considerable part of tooth crown. Cavity is wide opened (the overhanging edges of enamel are broken off because of their fragility). As a result, the transversal sizes of cavity exceed its depth. Walls and floor of carious cavity are filled with rather dense, pigmented dentin, but without sclerotic brilliance. Pigmentation of its walls and floor has enough wide spectrum – from yellow-brown to brown and even almost black color. Probing of walls and floor of the cavity is painless, because of development of well expressed areas of transparent and secondary dentin under them. Surface of the carious dentin is rough when probing. The development of such cavity continues for years.
Medical treatment of dental caries
Medical treatment of caries consists of a number of measures of general and local character depending on the stage of development of pathological process and character of its course. On early stages (caries incipience) this complex of measures is directed on the removal or reduction of effect of demineralized factors action, and also on renewal (remineralization) of partly demineralized hard tooth tissues. When the pathological process spreads to enamelodentinal junction, a dentine strikes and a carious cavity appears, conservative (remineralization) therapy can not result in success. It is connected with the fact that hard tooth tissues do not possess property to regenerate the primary form in the area of carious lesion. Therefore for local medical treatment of carious cavities their preparation is used, with the subsequent filling of cavity and renewal of anatomic form of tooth by filling material.
None of varieties of restoration treatment of dental caries can be complete “curing”. Destroyed with caries the hard tooth tissues (and adjoining areas of healthy enamel) are not substituted for newly formed enamel and dentin. Besides, there is no restoration material capable to protect hard tooth tissues from further destructive caries processes during all life. Tooth filling is only symptomatic treatment which does not eliminate the etiologic factors of dental caries.
Therefore the prevention of carious lesions development (prophylactic measures) is the basic principle of caries treatment, than – necessary medical treatment (remineralization therapy) and, in the last turn, forced measure – filling the carious cavity with filling materials, conducted along with the measures of the secondary caries prophylaxis.
Thus, now there are two main methods of local caries treatment:
- caries treatment without preparation and filling – remineralization therapy;
- operative caries treatment by the operative preparation of demineralized hard tooth tissues with the subsequent filling of carious cavity.
The choice of treatment method depends on the stage of caries development, activity of caries (acute or chronic), localization of carious cavity, age and general condition of patient.
Conservative medical treatment (remineralization therapy) of dental caries can be conducted only on the stage of absence of a cavity in hard tooth tissues, that is at caries incipience, when anatomic integrity of enamel is not broken.
In general for local remineralization therapy of incipient caries such groups of medications can be used:
1. Means, which influence on mineralization of enamel (they restore and complement ions which are absent in the crystals of enamel at caries; influence on kinetics of mineralization, ect).
2. Means, which prevent adsorption of organic matters (acids, toxins and other products of vital functions of microorganisms) on the surface of hard tooth tissues (desorbents, hydrofobic pellicle coverages, sealants).
Various preparations of fluoride, calcium, phosphor-calcium combination, complexes of mineral components (remodent), etc, are referred to the first group. Their introduction into the demineralized enamel areas renders assistance in remineralization, renewal of mineralization degree, increases stability of enamel to action of acids and other cariogenic factors. Preparations of fluoride, pectins, natural and synthetic varnishes, and various fissure sealants prevent adsorption of organic matters.
Preparations of calcium and fluoride are often applied for remineralization. The usage of different calcium salts is pathogenetic reasonable with its predominance among other mineral elements in the structure of hard tooth tissues apatites (hydroxyapatite, etc.). Efficiency of fluoride preparations application is conditioned with its influence on some mechanisms of pathological process.
There was proposed application and electrophoresis of 1 % solution of sodium fluoride for medical treatment of initial caries. The surface of teeth is carefully cleaned from dental plaques with the help of excavators or special brushes and pastes. Teeth are isolated from saliva and a cotton tampon or a small gauze serviette moistened with 1 % solution of sodium fluoride is put on the carious lesion. Duration of application is 15–20 minutes, during this time the cotton tampon with sodium fluoride solution is been changing 3–4 times. The course of medical treatment consists of 15–20 everyday application. More effective is introduction into enamel of fluoride with electrophoresis with 1 % solution of sodium fluoride that provides more deep penetration of fluoride ions in hard tooth tissues. Duration of procedure is 10–20 minutes, the course of medical electrophoresis treatment is 10 attendances.
Medical forms, which provide adhesion of fluoride preparation to the enamel, in particular, fluoride varnishes and gels, are developed for prolongation of fluoride action on hard, tooth tissues. Fluoride varnish is a composition of natural yellow resins of viscid consistency which contain 1–5 % fluoride (as often as sodium fluoride). For example, widely applied in practice fluoride varnish contains 5 % sodium fluoride, 40 % silver fir balsam, 10 % shellac, 12 % chloroform, 24 % ethyl alcohol, etc. A number of various fluoride varnishes is proposed, for example, “Fluor Protector”, “Duraphat”, “Bifluorid 12” (VOCO), “Belagel F”, “Belak F” (“VladMiVa”, Russia), etc. Teeth are isolated from saliva, dried out and on the area of demineralized enamel the fluoride varnish is applied, which dries up on the enamel surface during 4–5 minutes. Than the patient is recommended not to eat for 2–3 hours, to save this varnish film. It remains on the tooth surface for a few hours, that provides the long contact of fluoride with tooth enamel. Fluoride gels are also applied. In general the course of remineralization therapy consists of 15–20 attendances which are carried out every day or on alternate days.
For local medical treatment of initial caries the preparations of calcium are widely used: 10 % solution of calcium gluconate or calcium chloride, 5–10 % acidified solution of calcium phosphate, 2,5 % solution of calcium glycerophosphate. They are applied for applications and electrophoresis (the ions of calcium enter from a positive electrode – anode). The course of medical treatment depends on caries activity, number of carious lesions, etc., and it can achieve 15–20 applications or 10–15 procedures of electrophoresis. Efficiency of remineralization action of calcium preparations is multiplied at their combination with phosphorus preparations. As a remineralization preparation the solution, which contains 11 % calcium and 22 % phosphorus is also used (A. Iraig, I. Iraham, 1975). Calcium-phosphate gels, which provide long remineralization action, were also developed. As a remineralization mean fluid containing synthetic hydroxyapatite can be used.
As a result of the effectively carried out medical treatment (remineralization therapy) the demineralized areas of enamel diminish in sizes or disappear. It is possible transition of caries in its stationary form: in such cases a carious spot changes the color from chalky white to yellow or brown and some diminishes in sizes. To determine the effectiveness of the treatment the remineralization teeth are painted with dyes, for example, with 2 % water solution of methylene blue. If renewal of the degree of mineralization of enamel mineral structures is happened, the area of caries spot is not painted with methylene blue or the degree of staining is insignificant.
It has long been recognized that pits and fissures, especially on occlusal surfaces of teeth, are the most susceptible to caries. At localization of carious spots in fissures of molars and premolars one of the effective methods of medical treatment of such caries is sealing pits and fissures with sealants. Pit-and-fissure sealants provide safe and effective method of prevention of caries. Sealants are the most effective in children when they are applied to the pits and fissures of permanent posterior teeth immediately after eruption of the clinical crowns.
For fissure sealing a number of the most various preparations is used. For filling microspaces which appear in enamel at incipient caries the simple chemical matters can be used: silver nitrate, zinc chloride. Sealing cements (polycarboxylate, silicate, polyacrilic, glass-ionomer cements), composites (chemical and light cured) are actually used for fissures. For greater remineralization action the fluoride preparations are introduced into sealant composition.
At chronic course of incipient caries (yellow and brown carious spots) remineralization therapy is not obligatory. Except for preparation, at chronic caries the pigmented spots can be deleted with the method of enamel microabrasion. Enamel microabrasion is the controlled deleting of enamel, which changed its color, with the mixture of pumice powder and acid, usually hydrochloric acids. For this purpose special device is used – “HANDIBLASTER” (“Bisco”). This method is effective for medical treatment of superficial enamel discolorations (white or brown spots) caused by orthodontic treatment. The device sprays abrasive powder (usually aluminum oxide) on the surface of the tooth for preparation or treatment of the tooth surface before filling.
Operative caries treatment (filling)
During operative caries treatment and filling carious cavity such requirements are recommended to fulfill:
- Completely remove the hard tooth tissues, destroyed by caries, under sufficient anesthesia.
- Create the most convenient conditions for firm and reliable fixations of restorations in prepared carious cavity.
- Unite antiseptic processing with careful drying of prepared hard tooth tissues.
- Rationally select filling material according to classes of carious cavity and properties of restorative materials, following the rules of its manipulation and inserting into carious cavity.
- Grinding, finishing and polishing of the restoration.
In caries treatment such steps are distinguished:
- preparation of oral cavity;
- anesthesia;
- preparation of carious cavity (tooth preparation);
- application of isolating or curative liner;
- filling;
- modeling,
- final grinding, shaping and polishing of the restoration.
In general, the objectives of tooth preparation are to: (1) remove all defects and provide necessary protection to the pulp; (2) extend the restoration (carious cavity); mastication the tooth or the restoration or both will not break and the restoration will not be displaced; and (4) allow for esthetic and functional placement of restorative material.
General rules of tooth preparation:
- Pain control: local anesthesia, analgesia (inhalation sedation), hypnosis.
- Opening and widening the carious cavity.
- Necrectomy.
- Forming and shaping the cavity.
- Beveling enamel margins.
The conventional preparation design is typical for amalgam restoration and includes the following characteristics: (1) uniform pulpal and/or axial wall depths; (2) cavosurface margin design that results in a 90-degree restoration margin; and (3) primary retention form derived from occlusally converging vertical walls.
Clinical techniques of filling carious cavity:
- Antiseptical rinsing of oral cavity.
- Isolation of operating site (rubber dam, cotton rolls).
- Drying the carious cavity.
- Using traditional liners or bases to protect the pulp (up to DEJ).
- Placement and condensing the filling material.
- Contouring of restoration and correction of occlusion.
- Shaping and polishing of restoration (when using amalgam – after 24 hours on next visit).
Isolation of the operative field can be accomplished with a rubber dam or cotton rolls, with or without a retraction cord. Regardless of the method, isolation of the area is imperative if the desired result of restoration is to be obtained. Contamination of cavity enamel or dentin by saliva results in significantly decreased bond of filling material (composite), likewise, contamination of the composite material during insertion results in degradation of physical properties.
When zinc phosphate, glass-ionomer, or polycarboxylate cement bases are used, tooth depth and properties of prior liners determine the technique of placement. When there is known or suspected exposure to the pulp, it must be protected against forcing material into the pulp chamber. Therefore it is essential to either first use calcium hydroxide cement in adequate thickness or nonpressure technique for placing an overlay base.
The filling of carious cavity (e.g. glass-ionomer cements and compomers). Dry the prepared carious cavity of tooth but do not desiccate. The powder/liquid ratio is 2 scoops to 2 drops. Tumble the powder before dispensing. Mix the powder and liquid rapidly for 30 seconds. Place the mixed cement in the carious cavity. A gel state is reached after 1 minute, after which the excess cement can be removed.
The filling of caries cavity (e.g. composites). Once the tooth preparation was completed, the prepared tooth structure is prepared for composite insertion and shaping. Treating the prepared tooth for bonding requires etching and then application of an adhesive if only enamel is prepared, or primer and adhesive if the composite will be bonded to the dentin as well as enamel.
If liquid etchants are used, they are applied with small cotton pellets, foam sponges, or special applicator tips or microbrushes. The acid (liquid or gel) is gently applied to the appropriate surfaces to be bonded, keeping the excess to maximum of 0.5 mm more than expected extent of the restoration. An etching time 15 seconds – for both dentin and enamel is considered sufficient. For enamel-only preparations, 30 seconds is considered optimal. The area is then rinsed with water.
Once enamel (and dentin) is etched, rinsed, and left appropriately moist, the primer is applied to both surfaces. Most contemporary bonding systems combine the primer and adhesive into a single bottle, allowing only a one-time application. If this is the case, it is applied to the moist etched surfaces.
Inserting the Composite. The composite restoration is usually placed in two stages. First, bonding adhesives are applied (if not already placed during the procedures of etching and priming enamel and dentin). Second, the composite restorative material is inserted. With newer bonding systems the adhesive may be combined with another component of the system, mostly the primer. Therefore, as usual, etching and priming the prepared tooth structure and placing the bonding adhesive should be done according to the manufacturer’s directions.
Starting in the most remote area of anterior tooth preparation, the composite is steadily injecting, ensuring that the tip remains in the material while slowly withdrawing the syringe. If the area is large, the light-cured composite is placed in 1 to 2-mm thicknesses, with each increment being cured per manufacturer’s instructions. Usually a hand instrument is used to adapt the composite to the preparation after each syringe injection of material. When curing, the light should be kept as close to the material as possible. If using a hand instrument insertion, a small amount of the composite is carried to the remote area of the preparation and condensed and cured; then more composite is placed and cured with care to adapt it well to the internal preparation walls. The preparation is filled to slight excess so that positive pressure can be applied by the matrix strip.
Following insertion and polymerization of the composite material, the matrix and wedges are removed. If correction is needed, it should be accomplished at this time, because any additions will bond satisfactorily to the uncontaminated, oxygen-inhibited surface layer of the composite material.
Contouring can be initiated immediately after the light-cured composite material has been polymerized or 3 minutes after the initial hardening of self-cured material.
Polishing the contoured composite restoration is done with very fine polishing discs, fine rubber points or cups, and/or composite polishing pastes. Although conventional finishing techniques produce a smooth surface texture with microfill composites, a higher luster can be obtained by using discs, rubber points, or cups, all of which are specifically made for polishing these materials.
Systemic caries treatment. Dental caries is a disease which attacks the dental hard tissues by demineralising enamel. If oral conditions are favourable then this demineralisation can progress from the outer enamel layer of the tooth into the softer underlying dentine, resulting in decay. Dental decay is more common in individuals who often dietary intake of sugars (fermentable carbohydrates). Frequency of intake of carbohydrate is more predictive in the decay process than the absolute amount.
A number of nutritional factors, which may be factors in growth and development such as Vitamins A and D, water hardness and proteins, are hypothesised as potentially linked to dental caries. However, there is little evidence to demonstrate that systemic effects of poor nutrition increase the risk of dental decay, and it is generally accepted that while diet can have a profound local effect on erupted teeth, it has much less effect while the teeth are forming. The diet-caries relationship therefore needs to be evaluated not only against the quantity and type of fermentable carbohydrate consumed, but also against several background factors including intake pattern, total food intake, salivary secretion rate, plaque composition and use of fluoride.
Although the type of sugar consumed is an important factor in development of caries, the frequency of sugar consumption is of greater significance. It has been accepted that the frequency of ingestion of sugar-containing foods is directly proportional to caries experience: that was found that children with caries have snacks between meals approximately four times each day. Children with caries have a high frequency of sugar consumption, not only in fluids given in the nursing bottle, but also in sweetened solid foods. Increased frequency of eating sucrose increases the acidity of plaque and enhances the establishment and dominance of aciduric Mutans Streptococci. It is logical to suppose that partial substitution of sugar in the diet can lead to reduction in the total sugar consumption. The low caries rate in children was associated with total intake of sugars of 10 kg per person per year (about 30 g/day), but caries development increases steeply with intakes of 15 kg upwards (WHO, 1990).
Numerous studies show the prevalence of the disease as to affect up to 70 % of the childhood population, especially in socio-economically deprived population. Inadequacy of the host’s immune-defences may play a role in the acquisition of carious lesions.
Foods and food components that have anticariogenic properties are sometimes referred to as “cariostatic factors”. Despite being one of the main sources of sugars in the diet, milk is anticariogenic. The sugar in milk is lactose, which is the least cariogenic sugar, and milk is also known to contain protective factors. The cariostatic nature of milk can be attributed to the presence of calcium, phosphate, casein and lipids. Calcium and phosphate are present in cow’s milk in high concentrations (125 mg and 96 mg/100 g respectively) and are able to prevent enamel demineralization. Consumption of cheese increases oral pH by stimulating salivary flow and raises plaque calcium concentrations, both of which protect against demineralization.
Tea also contains polyphenols, in addition to fluoride and flavanoids. Tea extracts have also been shown to inhibit salivary amylase activity. The protective effect of tea may be associated with fluoride or antibacterial action of polyphenols, or both.
Dietary control is an important part of caries prevention. Successful dietary advice at the level of an individual (advice that leads to caries reduction) requires effective advice, adequate provision and resources to provide advice, and patient compliance. However, efforts at this level need to be reinforced with population-based strategies for caries prevention.
The arrows in the preventive non-operative quiver are:
- plaque control;
- use of fluoride;
- dietary modification.
The way in which each of these modalities is used will depend on the circumstances of the individual patient.
Since carious lesions form as a result of the metabolic processes in the dental plaque, good plaque control must be the cornerstone of preventive non-operative treatment. Teeth should be brushed regularly, at least once every day with a fluoride-containing toothpaste. The brushing interferes with the growth of the biofilm and the fluoride application retards lesion progression. The quality of cleaning, rather than the frequency, seems to be of prime importance.
No change in diet should be suggested for a caries-inactive patient, but the dentist should still make the patient aware of how changes in diet (e.g. frequent sugar attacks) may pose a problem if the oral hygiene is poor.
Complication of the caries: pulpitis and periodontitis
Pulpitis
Progressive caries destruction of hard tooth tissues without treatment leads to penetration of microorganisms and toxins into pulp. As a result – developed pulp inflammation (pulpitis) and apical periodontitis. So these diseases are called caries consequences.
The inflammation of pulp – pulpitis, occurred in 14–25 % of cases among other dental diseases. Character of pulp inflammation, its course, dynamics of development are usually connected with different levels of organism resistance. Processes of exudation, alteration (destruction) and proliferation prevail in clinical features.
The causes of pulp inflammation are microorganisms and different traumatic, chemical and iatric (cavity preparation, restoration, orthodontic movement, periodontal curettage) irritants.
Bacterial causes. Caries is, by far, the most common way of penetration into the dental pulp of infecting bacteria and/or their toxins. Long before the bacteria reach the pulp to actually infect it, the pulp becomes inflamed from irritation by preceding bacterial toxins. Pathosis increase, however, when the lesion reaches the depth of 0,5 mm of the pulp, and abscess formation develop when the irritation dentin barrier is breached. The acuteness or chronicity of caries as a disease serves to stimulate the production of effective irritation dentin barrier. The highly acute lesion evidently over-whelms the pulp’s calcific defense capability, while chronic lesion provides time for the development of irritation and sclerotic dentin defense. Decalcified leathery dentin might provide bacterial pathway for pulp invasion and infection. Accidental coronal fracture in the pulp seldom devitalizes the pulp at that instant. Incomplete fracture of the crown (infraction), usually from unknown causes, often allows bacteria enter the pulp. Most of the bacteria of the endodontic infection are strict anaerobes.
Iatric causes. The heat generated by grinding procedures of tooth structure is often cited as the greatest single cause of pulp damaging during cavity preparation.
Another traumatic factors: the increased incidence of pulp death following pulp exposure after wrong preparation. The advent of pin placement into the dentin to support amalgam restorations, or as a framework for building up badly broken down teeth for full-crown construction, an increase in pulp inflammation and death have been noted.
Chemical causes. To the severe insult of dental caries bacteria to the pulp, plus the iatric trauma from cavity preparations, the chemical insult from the various filling materials must be added. Silicate cements have long been condemned both clinically and histologically as a pulp irritant. The composites contain acrylic monomers in their catalyst system, and it can be assumed that the monomer would cause damage, as in the case of cold-curing resins. One could say that pulp injury from chemical irritants can best be prevented by not applying chemicals to the dentin.
Pulpal pathosis is basically a reaction to bacteria and bacterial products. This can be a direct response to caries, microleakage of bacteria around fillings and crowns, or bacterial contamination after trauma, either physical or iatrogenic. The pulp responds to these challenges by the inflammatory process.
Since the pulp histological diagnosis is impossible to determine without removing it and submitting it for histological examination, a clinical classification system was developed. This system is based on patient’s symptoms and results of clinical tests. There are next pulpitis forms to be distinguished:
I. Acute pulpitis:
- Pulp hyperemia.
- Acute circumscription pulpitis.
- Acute diffusion pulpitis.
- Acute purulent pulpitis.
- Acute traumatic pulpitis.
II. Chronic pulpitis:
- Chronic fibrous pulpitis.
- Chronic hypertrophic pulpitis.
- Chronic gangrenous pulpitis.
- Chronic concremental pulpitis.
III. Exacerbative chronic pulpitis.
IV. Pulpitis complicated periodontitis.
Chief complaints and chief clinical features. The main characteristic symptom of the acute pulp inflammation is spontaneous (i.e., unprovoked), intermittent, or continuous pain attacks. Sudden temperature changes (usually cold) elicit prolonged episodes of pain (i.e., pain remains after the thermal stimulus is removed). The pain attack arises suddenly, regardless of external irritants, sometimes provoked by chemical, thermal and mechanical irritants.
The pain differs from that of a hyperreactive pulp in that it is not just a short, uncomfortable sensation but an extended pain. Moreover, the pain does not necessarily ceases when the irritant is removed, but the tooth keep aching for minutes or hours, or days.
Pain may start spontaneously from such a simple act as lying down. This in itself explains the seeming prevalence of toothache at night. Some patients complain that the pulp hurts each evening, when they are tired. Others say that leaning over to tie shoes or going up or down stairs – any act that raises the cephalic blood pressure – will cause pain. The list of inciting irritants would not be complete without mentioning sucking and biting hot food or drink. Most often pain, however, is started when eating, usually something cold. The patient can tell which side is involved and frequently whether pain is in the maxilla or in the mandible. This may not be absolute, however, for pain, which may be referred from one arch to the other. Patients complain about aching of a maxillary molar when the maxillary lateral incisor has been found to be the offender. The patient may insist that a mandibular molar is aching, whereas examination reveals that a maxillary molar is the offender.
Pulp hyperemia. All minor pulp sensations were once thought to be associated with hyperaemia – increased blood flow in the pulp. Quite possibly, this will explain why the pain appears to be of a different intensity and character with applications of cold or heat, the cold producing a sharp hypersensitivity response and the heat producing transient hyperemia and dull pain. Pain arises spontaneously or as a result of irritant action, pulp attacks last for 1–2 minutes with large painless intervals (intermission) up to 6–12–24 hours. More often pain attacks arise at night.
Acute circumscription pulpitis. This pulpitis is characterized by spontaneous (i.e., unprovoked), intermittent, or continuous paroxysms of pain. The pain is frequently described as a “nagging” or a “boring” pain, which may at first be localized but finally becomes diffuse or referred to another area. The pain attack can be provoked by different irritants, usually the cold. Pain attack at first lasts 15–30 minutes, but with development of the inflammatory process in pulp its duration increases to 1–2 hours. Pain attacks increase and become more frequent at night. Painless intervals usually last 2–3 hours and then become shorter. Usually patients indicate the causal carious tooth, but in some cases the pain may be referred from one arch to the other.
Acute diffuse pulpitis. It is characterized by spontaneous pain and development of acute pain attack, reffered from one arch to the other and along the branches of n. trigeminus. The character of pain attack is like of neuralgic attacks. One-two days ago the duration of pain attack was 10–30 minutes and now pain attacks last for an hour. The durability of painless intervals decreased to 10–30 minutes. Pain attacks increase and become more frequent at night and at horizontal position of patient. Usually patients indicate on the causal carious tooth, but in some cases the pain may be referred from one arch to the other.
Acute purulent pulpitis. Acute purulent pulpitis is usually a result of further development of diffuse pulp inflammation. It is characterized by the spontaneous pain and development of acute pain attack, reffered from one arch to the other and along the branches of n. trigeminus. Pain attack increases, pain becomes pulsative, continuous with remission only for some minutes. At night pain attack becomes more intensive. The pain arises and increases as a result of cold irritants (hot meals, temperature more than 37 °C). Cold irritants relieve the pain.
Acute traumatic pulpitis. The main cause of this form of acute pulpitis is careless preparation of carious cavity, which results in perforation of pulp chamber with insignificant pulp trauma by rotary instrument (burs). Enough often it occurs during acute caries course preparation of carious cavity or removal of leather decalcinated dentin during excavation. As a result a bleeding point perforation appears. Through this perforation dentist may see pink pulp.
Chronic fibrous pulpitis. Unlike the acute form of pulpitis at chronic fibrous pulpitis patients feel a heaviness in the tooth. Pain appears in reply to action of thermal, chemical and mechanical irritants, intensity of which usually depends on the location of carious cavity. At the opened pulp chamber of the tooth and on the central location of carious cavity a “sucking” in the tooth can cause a quickly passing aching pain. Unlike caries the pain at chronic fibrous pulpitis lasts 30–90 minutes after cessation of irritant action.
Chronic hypertrophic pulpitis. This form of pulpitis often develops in children and young people. Patients complain of pain and appearance of blood from the carious cavity when chewing – as a result of a trauma or a food lump or at “sucking” in the tooth. Objectively in the affected tooth there is a large carious cavity filled with fleshy tumor formation. This overgrowing pulp bleeds and is little sensitive when probing, but the area of the root canals entrance is painful. Circling around the “polypus” with a probe (determination for “area of growth”), it is possible to make sure in its connection with the pulp. The dull pain is a result of action of cold irritants.
Chronic gangrenous pulpitis. Spontaneous pain is absent, when there is perforation of the carious cavity floor. The unpleasant feeling of expansion in the tooth is the permanent sign of gangrenous pulpitis. The pain usually slowly arises under influence of thermal (hot) irritants and lasts for a short time. Spontaneous pain arises and is observed when the pulp chamber is closed and the exudates cannot flow from the inflamed pulp.
In affected tooth there is a large carious cavity filled with softened dentin. The pulp chamber in most patients is opened and filled with products of pulp disintegration with an unpleasant smell. The reaction on the superficial probing is absent. The deep probing is painful. The leathery dentin covering these lesions may be removed with a spoon excavator, often without anesthesia and without great discomfort. The pulp remains revealed, covered with a grey scum of surface necrosis. Some crown discoloration may accompany pulp necrosis in anterior teeth, but this diagnostic sign is not reliable.
Chronic concremental pulpitis. The causative factor of this form of pulpitis are denticles – calcified deposits in the dental pulp. Usually they are located in the pulp chamber or root canals. It may be composed either of irregular dentine (true denticle) or ectopic calcification of pulp tissue. Denticle is formed in teeth, located in the back (molars, premolars), most often in persons over 40 years. These formations cause the permanent irritation of nervous endings of pulp, resulting in chronic inflammation.
Patients complain of spontaneous pain and development of acute pain attack, referred from one arch to the other and along the branches of n. trigeminus. The character of pain attack is like of neuralgic attacks. Pain attacks increase and become more frequent at night and under vibration. Clinical features resemble trigeminal neuralgia. Pain attack lasts 15–30 minutes. Vertical percussion is painful and may provoke pain attack.
Exacerbative chronic pulpitis. Every form of chronic pulpitis may be exacerbated. Often this is fibrous pulpitis, more rarely – chronic gangrenous pulpitis. Exacerbative chronic pulpitis is characterized by spontaneous pain and development of acute pain attacks, referred from one arch to the other and along the branches of n. trigeminus. Pain attacks increase and become more frequent at night and at horizontal position of patient. The pain attack can be provoked by different irritants, usually the cold. Duration of pain attack may be different: at first it lasts 15–30 minutes, but with development of the inflammatory process in the pulp its duration increases to 1–2 hours. When inflammation develops in root pulp, vertical percussion becomes painful.
Pulpitis complicated apical periodontitis. The clinical features combined clinical signs of pulpitis and apical periodontitis. For example it may be signs of acute diffuse or purulent pulpitis and signs of apical periodontitis. The durability of pain attack was 10–30 minutes and now attacks last about an hour. The durability of painless intervals decreases to 10–30 minutes. Pain attacks increase and become more frequent at night and at horizontal position of patient. Usually patients indicate on the causal caries tooth.
These signs of pulpitis combine with signs of apical periodontitis. There can be edema of soft facial tissues (lips, cheeks), especially on the site of affected tooth. There is hyperemia and edema in the area of tooth apex, sometimes hyperemia is present in the gums surrounding areas. In some cases the periosteal abscess may develop. Horizontal and vertical percussion of the tooth is very sensitive. The tooth mobility in medial, distal and vertical directions is observed.
Pulpitis tratment
Now two main methods of pulpitis treatment are developed: biological and operative (surgical).
The biological method of pulpitis treatment is directed to make pulp healthy with renewal of its function. One of important values is its complete renewal or saving its basic functions: formative, nutritive, reparative. It saves the valuable hard tooth tissue structure, makes protective, barrier actions and prevents the development of apical periodontitis.
The carrying out of conservative (biological) method of treatment of pulpitis consists in: preparation the carious cavity, complete removal of carious dentin and irrigation carious cavity with warm antiseptic solution, placing the medicamental paste on the carious cavity floor. It contains antibiotics, sulfonamides, corticosteroids, calcium hydroxide preparations, enzymes and their inhibitors, nitrofuranes, etc. Carious cavity must be closed with temporary hermetic dressing (artificial dentin, zink-eugenol cements, etc.). After 7–14 days, at the second patient visit, if pain is absent, temporary dressing will be removed and changed for permanent composite or amalgam restoration.
The main treatment of pulp inflammation consists of removing the vital pulp from pulp chamber (pulp amputation) and root canal. This is called pulp extirpation or pulpectomy. Total pulpectomy, extirpation of the pulp near the apical foramen, is indicated when the root apex is fully formed and the foramen is sufficiently closed to enable obturation with conventional filling materials.
The performance of a well-executed pulpectomy consists of the following steps: use of regional anesthesia, preparation of the carious cavity, complete removal of carious dentin, excavation of the coronal pulp (amputation), extirpation of the radicular pulp, root canal preparation, thorough debridement of the root canal system, obturation the root canal, placing permanent composite or amalgam restoration.
Apical periodontitis
Apical periodontitis – disease, that arises in periodontal ligament tissues as a result to actions of different irritant factors with development of local inflammation. As a results – damage of periodontal ligament tissues, pathologic mobility of the tooth and even loss of the tooth. Clinical features of apical periodontitis are enough different, therefore it is necessary to study main etiologic causes of development of the disease. The prevalence of apical periodontitis consists of between 15–30 % among all dental patients.
Etiologic irritant factors of apical periodontitis are quite various, their nature is of substantial value for appearance and development of pathological process. Therefore the doctor must define the etiologic factors of disease and carry out its treatment taking into account the etiology. Localization of process is no less important. Inflammation can spread to apical part of periodontal ligament, as a result apical periodontitis develops, or spread to its marginal part, and then marginal (regional) periodontitis develops. The most widespread is apical periodontitis.
Apical periodontitis depending on clinical and radiographic manifestations is classified as infectious (living, microbial irritants) and noninfectious (nonliving irritants) genesis.
Infectious apical periodontitis is the most widespread in dental practice. The main cause of its development is action of different microorganisms and their toxins, present in the carious cavity, pulp chamber, root canals.
The most common causative factors in periodontitis development (infectious inflammation) are associations of aerobic and anaerobic microorganisms. Microorganisms and their toxins get into periodontal ligament in various ways.
The most widespread (main) way – through a root canal. More often infection gets into periodontal space at the diffuse forms of pulp inflammation – at acute purulemnt pulpitis, chronic gangrenous pulpitis. Bacteria and their toxins get into periodontal space and cause inflammatory reaction of periodontal ligament.
Quite often the inflammatory process spreads from periodontal space into adjoining bone tissue of the jaw. In the bone develops a purulent process – pus penetrates into the bone tissue through Haversian and Vollkmann`s canals and gathers under a periosteum. At acute purulent apical periodontitis it is possible to distinguish 4 successive phases:
The periodontal phase – purulent process in the limits of periodontal space, reactive inflammation in the alveolar bone.
The endostal phase – pus in the alveolar bone, with infiltration of periosteum.
The subperiostal phase – pus under periosteum (subperiostal abscess).
The submucous phase – destruction of periosteum, pus in soft tissues (submucous abscess).
Acute and chronic periodontitis is one of the main causes of premature loss of teeth. The prevalence of different forms of apical periodontitis is between 15 to 30 %. The lesion often develops and enlarges as a result to inadequate treatment of the root canal. Generally, the necrotic pulp gradually releases toxious agents with low-grade pathogenicity or in low concentration that results in the development of chronic apical periodontitis. This pathosis is a long-standing, “smoldering” lesion and it is usually accompanied with radiographically visible periradicular bone resorption.
In Ukraine and Russia the classification of apical periodontitis by I. G. Lucomsky (1955) is used. In accordance with this classification all forms of apical periodontitis are subdivided into 3 main groups.
I. Acute apical periodontitis:
- Acute serous apical periodontitis.
- Acute purulent apical periodontitis.
II. Chronic apical periodontit:
- Chronic fibrous apical periodontitis.
- Chronic granulating apical periodontitis.
- Chronic apical granulomatous periodontitis.
III. Exacerbative chronic periodontitis.
Clinical features and diagnostic of apical periodontitis
Acute serous apical periodontitis. This clinical form develops mainly as complication of pulp inflammation or as a result of inadequate root canal debrigement when treating pulpitis.
Clinical features. At first patients complain about the weight and tension in the tooth. The tooth seems to be greater and longer than others. Gradually quite strong spontaneous pain appears. The pain is permanent, localized, not irradiate, increases at night and does not almost decrease with ordinary analgetics. As a process develops constantly, pain intensity grows. Pain varies from slight tenderness to excruciating pain in contact with opposing teeth.
The affected tooth can be damaged, that does not exclude trauma (for example when using an orthodontic appliance). More often, however, it is caries, with necrotic pulp, perforation of pulp chamber or large restoration. Enamel loses its natural translucency which is characteristic for intact enamel and becomes dark-grey. There is hyperemia and edema in the area of tooth apex, and sometimes in the adjoining areas of the gums. The tooth is sensitive to vertical percussion. The reason of such reaction is the inflammation in periodontal space and irritation of nervous receptors of periodontal ligament. Palpation of gingiva in the area of tooth apex (especially frontal teeth) is painful. Regional lymphatic nodes are enlarged and painful during palpation.
The acute purulent apical periodontitis usually develops after serous one. This pathologic process is a diffuzed inflammation of the periodontal ligament in the apical region.
Sensitivity to percussion is the principal clinical feature of the acute purulent apical periodontitis. Pain is pathognomonic and varies from slight tenderness to excruciating pain in contact with opposing teeth. Regardless of the causative agents, acute purulent apical periodontitis is associated with exudation of plasma and emigration of inflammatory cells from the blood vessels into the periradicular tissues. Radiographs show little variation, ranging from normal to a “thickening” of the periodontal ligament space in teeth associated with acute purulent apical periodontitis.
The affected tooth can be damaged or change its color, sometimes there is a large carious cavity or restoration. The pulp chamber in most cases is not perforated, the pulp is necrotic. In root canals the gangrenous disintegration of pulp tissue is revealed, quite often pus goes out under pressure. Horizontal and vertical percussion of tooth are very sensitive. Tooth mobility in medial, distal and vertical directions is observed.
There is significant edema of the soft tissues of the face (lips, cheek), especially on the site of the affected tooth. There is hyperemia and edema in the area of tooth apex, sometimes in the adjoining areas of gums. In some cases the periosteal abscess may develop. In some cases pus gathered in periodontal space can pour out through the root canal of the tooth. Also pus may penetrate into the bone tissue of the jaws and as a result the limited osteomyelitis develops. The toxins and inflammation mediators may penetrate into regional lymphatic nodes, which enlarge and become painful during palpation.
Chronic fibrous apical periodontitis is asymptomatic apical periodontitis and may be preceded by acute serous apical periodontitits or by apical abscess. The clinical features of chronic fibrous apical periodontitis are unremarkable. Patients usually report no significant pain, and tests reveal little or no pain on percussion.
The affected tooth may be carious or devital (pulpless tooth, tooth from which the pulp was removed or replaced with filling material). Palpation of surrounded gingiva in the area of apex is painless.
Radiographic findings are the diagnostic key. Chronic fibrous apical periodontitis (asymptomatic apical periodontitis) is usually associated with periradicular radiolucent changes. These changes range from irregular thickening of the periodontal ligament to its hypercementosis.
Chronic granulating apical periodontitis. Its prevalence makes 65–70 % of all cases of chronic apical periodontitis.
When this form of chronic apical periodontitits develops, bone and periodontal ligament can be replaced by inflammatory granulation tissue. This process is associated with formation of new vessels, fibroblasts, and sparse, immature connective tissue fibers.
Patients feel some painfulness during chewing and pressure. The affected tooth may be damaged, carious or devital (pulpless tooth). The tooth usually changes its color (grey or, even, dark grey). The tooth may be slightly sensitive under vertical percussion. There is some chronic hyperemia of gingiva in the area of the root apex. Palpation in the area of tooth apex depending on the stage of the process is accompanied by more or less expressed pain.
This form of apical periodontitis is also referred to as suppurative apical periodontitis. It is associated with gradual egress of irritants from the root canal system into the periradicular tissues and formation of the exudate. Asymptomatic apical abscess is associated with either continuously or intermittently draining sinus tract. This is visually evident as a stoma on the oral mucosa or occasionally as a fistula on the skin of the face. The exudate can also drain through the gingival sulcus of the involved tooth.
As a result to granulation tissue growing the fistula can form on the gingiva or skin at the tooth apex area. When pressing pus drops appear from the fistula. Sometimes in the area of fistula it is possible to see one or several scars. This form of chronic apical periodontitis may be exacerbated with developing clinical feature resembling acute apical periodontitis.
Radiographic findings express irregular thickening of the periodontal space, destruction of compact cortical plate of alveolar bone with developing large radiolucent area in periradicular tissue.
Chronic apical granulomatous periodontitis is the limited inflammation of periodontal ligament with formation of a round lesion. This condition is almost invariably a sequela of pulp necrosis.
The clinical features of chronic apical granuloma are unremarkable. Patient usually report no significant pain, and tests reveal little or no pain on percussion. Palpation of superimposed tissues may not cause discomfort. The affected tooth has necrotic pulp and therefore cannot respond to electrical or thermal stimuli. The tooth changes its color, can be damaged or restored. Vertical percussion is often painless. However percussion of the affected tooth in comparison with neighbouring teeth may be more sensitive. The ginigva in the tooth apex area does not change its color and painless during palpation.
Radiographic findings express periradicular limited round radiolucent area. There is thickening of bone tissue around the radiolucent area as a result of its sclerotic changes.
A sudden egress of bacterial irritants into the periradicular tissues can precipitate chronic apical periodontitis and its more severe sequelae – exacerbative chronic apical periodontitits.
Exacerbation of inflammation can develop regardless of different forms of chronic apical periodontitis, but more often in granulating periodontitis and rarer – fibrous periodontitits. The exacerbative chronic apical periodontitis occurs much more often than acute. Its clinical features are similar to symptoms of acute apical periodontitis. The peculiarity of clinical features of exacerbative chronic apical periodontitis consists in destruction of both periodontal ligament and periradicular bone.
Patients may or may not have swelling. When it is present, the swelling may be localized or diffuse. Clinical examination of the tooth with exacerbative chronic apical periodontitis shows varying degrees of sensitivity to percussion and palpation. The tooth may be damaged, carious or restored. There is no pulp reaction to cold, hot, or electrical stimuli as the involved tooth has necrotic pulp. The tooth is very sensitive to vertical and horizontal percussion. Pathologic mobility of the affected tooth may develop.
There can be a significant edema of the soft facial tissues (lips, cheeks), especially on the site of the affected tooth. There is hyperemia and edema in the area of tooth apex, sometimes hyperemia is present in the adjoining areas of gums. In some cases the periosteal abscess may develop. The regional lymphatic nodes enlarge and become painful during palpation.
Radiographic findings are similar to different forms of chronic apical periodontitis (fibrous, granulation, granuloma).
Treatment of apical periodontitis
The methods of apical periodontitis treatment can be divided into 4 groups:
- Conservative – aimed at preserving anatomic and functional value of the affected tooth.
- Conservative-surgical – aimed at preserving basic functions of tooth. Removing of part of the root or periradicular tissues, destroyed during the pathological process, and which cannot be treated, is expected.
- Surgical – removing of the affected tooth (extraction) and pathologically changed alveolar bone.
- Physical.
Conservative treatment of periodontitis is carried out with purpose to remove the source of periodontal ligament contamination (pathologically changed pulp tissues, dentin, microflora of root canal and dentinal tubules) with careful instrumentation, medical treatment of root canals and their obturation. Removal of the infection source should allow the inflammation of periodontal ligament to subside and symptoms to dissipate. These stimulate the regeneration of periodontal ligament and periradicular tissues.
Indications for conservative treatment:
- Acute and chronic apical periodontitis of one-rooted teeth (with good negotiate canals) and absence of significant changes in periradicular tissues.
- Acute and chronic apical periodontitis of multy-rooted teeth (with good negotiate palatinal canals of upper teeth and good distal canals of lower teeth) and absence of significant changes in periradicular tissues.
The main tasks of conservative treatment are:
- Pain elimination.
- Drainage of periodontal space.
- Conduction of medicinal (antibacterial and anti-inflammatory) treatment of root canals.
- Stopping further spread of inflammatory process in periradicular tissues.
- Restoration of anatomical form and function of teeth.
Treatment of acute infectious apical periodontitis. The acute infectious apical periodontitis has very short phase of intoxication, but strongly expressed exudation, that develops quite rapidly. Exudate formed in periodontal space and periradicular tissues can spread into adjoining tissues in various ways: through a root canal, through the alveolar bone of jaw under periosteum from vestibular or lingual (palatal) side. The main goals of acute infectious apical periodontitis (both serous and purulent) treatment are: pain reducing, performing the drainage for releasing purulence (exudates), conducting antimicrobial and antibacterial treatment, stopping the spread of inflammation in periradicular tissues, regeneration of periodontal ligament and periradicular tissues with restoration of tooth anatomic form and functions.
After cleaning the root canal the dentist reaches the tooth apex and apical foramen. Once the tooth is opened for treatment, drainage is carried out throughout the canal and remains open. Warm saline or antiseptic rinses are used for approximately 24–48 hours after the drainage procedure.
At secondary appointment (visit) such stages of medical treatment are carried out: thorough final preparation of carious cavity (tooth), root canal preparation, obturation of root canal, radiographic studies necessary for assessing the quality of root canal filling, placing temporary or permanent restoration (composites, amalgam, inlay, artificial crown) after the intraorifice barrier was placed.
Treatment of chronic apical periodontitis. The main goals of treatment are: elimination of the source of periodontal ligament contamination, further suppression of pathologic microflora of root canals and its diverse ramifications; providing conditions for regeneration of periradicular tissues; hyposensibilization of patient’s organism.
The next goals of treatment are thoroughly preparation of the carious cavity, providing access to pulp chamber and root canals, root canal preparation. At this stage the preparation is fully performed, including canal negotiation, canal shaping, and, finally, apical preparation. After preparation is complete the medicaments such as calcium hydroxide (antiseptics, sorbents, enzymes, etc.) are placed with a long cotton pellet and temporary filling is placed.
At secondary appointment. There are obturation of root canal, radiographic studies necessary for assessing the quality of root canal filling, placing temporary or permanent restoration (composites, amalgam, inlay, artificial crown) after the intraorifice barrier was placed.
Conservative-surgical methods of apical periodontitis treatment
Several factors have resulted in a significant impact on the indications for and the application of endodontic surgery. Even though the success rate of nonsurgical endodontic treatments is high, failures do occur. There is a few absolute contraindications to endodontic surgery. Most contraindications are relative, and they are usually limited to three areas: (1) the patient’s medical status, (2) anatomic considerations, and (3) the dentist’s skills and experience.
Surgical drainage is indicated for purulent and/or hemorrhagic exudate forms within the soft tissue or alveolar bone as a result of symptomatic periradicular abscess. A significant reduction of pain and a decrease in the disease duration will follow the pressure reduction and the elimination of by-products of inflammation and infection. Surgical drainage may be accomplished by (1) incision and drainage (I & D) of the soft tissue or (2) trephination of the alveolar cortical plate.
Endodontic surgery encompasses surgical procedures performed to remove the causative agents of periradicular pathosis and to restore the periodontium to a state of biologic and functional health.
These procedures may be classified as follows (the most frequently used):
- Root-end resection.
- Root resection (amputation).
- Hemisection.
Chapter 7. Diseases of periodontal tissues
Inflammatory and inflammatory-dystrophic diseases of periodontium
“Periodontology” is the specialty that studies the tooth-supporting tissues – “periodontium”. The periodontium is made up of those tissues that surround each tooth and anchor each tooth into the alveolar process (Latin: para = adjacent to; Greek: odus = tooth).
The periodontium consists of the investing and supporting tissues of the tooth (gingiva, periodontal ligament, cementum, alveolar bone). The cementum is considered to be part of the periodontium because, along with the bone, it serves as the support for the fibers of the periodontal ligament. The periodontium is subject to morphologic and functional variations, as well as changes associated with aging.
Periodontal Diseases
Gingivitis – Periodontitis
There are numerous diseases that affect the periodontium. By far the most important of these are plaque-associated gingivitis (gingival inflammation without attachment loss) and periodontitis (inflammation-associated loss of periodontal supporting tissues).
Gingivitis is limited to the marginal, supracrestal soft tissues. It is manifested clinically by bleeding upon probing of the gingival sulcus, and in more severe cases by erythema and swelling, especially of the interdental papillae.
Gingivitis is characterized by plaque-induced inflammation of the papillary and marginal gingivae. Clinical symptoms include bleeding on probing, erythema, and eventual swelling. Gingivitis may be more or less expressed depending on the plaque – a biofilm – (quantity/quality) and the host response. Deeper-lying structures (alveolar bone, periodontal ligament) are not involved. Gingivitis may be a precursor to periodontitis, but this does not always occur.
Periodontitis can develop from a pre-existing gingivitis in patients with compromised immune status, the presence of risk factors and pro-inflammatory mediators, as well as presence of a predominately periodontopathic microbial flora. The inflammation of the gingiva may then extend into the deeper structures of the tooth-supporting apparatus. The consequences include destruction of collagen and loss of alveolar bone (attachment loss). The junctional epithelium degenerates into a “pocket” epithelium, which proliferates apically and laterally. A true periodontal pocket is formed. Such a pocket is a predilection site and a reservoir for opportunistic, pathogenic bacteria; these bacteria sustain periodontitis and enhance the progression of the disease processes.
Periodontitis is usually a very slowly progressing disease (Locker & Leake 1993; Albandar et al. 1997), which in severe cases – particularly when untreated – can lead to tooth loss. Enormous variation in the speed of progression of periodontitis is observed when one differentiates between individual patients. In addition to the quantity and composition of the bacterial plaque, individually varying influences also play important roles: patient’s systemic health, patient’s genetic constitution, psychically influenced immune response status, ethnic and social factors, as well as risk factors such as smoking and stress
In the aggressive forms of periodontitis, the manifestation of tissue loss on individual teeth occurs in successive acute phases rather than in a gradual, chronic progression. Phases of progression and quiescence alternate. Destructive phases may occur rapidly one after another, or longer quiescent phases may be noticeable.
Gingival recession
Gingival recession is not actually a “disease,” but rather an anatomic alteration that is elicited by morphology, improper oral hygiene (aggressive scrubbing), and possibly functional overloading.
Teeth do not fall out due to classical gingival recession, but patients may experience cervical hypersensitivity and esthetic complications. If gingival recession extends to the mobile oral mucosa, adequate oral hygiene is often no longer possible. Secondary inflammation is the consequence.
In addition to classical gingival recession, apical migration of the gingiva is often observed in patients with longstanding, untreated periodontitis, and it may be a consequence of periodontitis therapy in elderly patients (“involution”). These three periodontal disorders – gingivitis, periodontitis, gingival recession – are observed world-wide; they affect almost the entire population of the globe to a greater or lesser degree. In addition to these common forms of oral pathology, more rarely defects and diseases of periodontal tissues occur. All of these diseases were comprehensively classified at the international World Workshop in 1999.
Classification of diseases of the periodontium
Disease classifications are useful for the purposes of diagnosis, prognosis, and treatment planning. Different classifications of periodontal diseases have been used over the years and have been replaced as new knowledge improved our understanding of the etiology and pathology of the diseases of the periodontium.
Traditionally, periodontal diseases have been divided into two major categories: gingival diseases and periodontal diseases. The former includes diseases that attack only the gingiva, whereas the latter includes diseases that involve the supporting structures of the tooth.
Gingival diseases
Gingivitis (inflammation of the gingiva) is the most common form of gingival disease. Inflammation is almost always present in all forms of gingival diseases, because bacterial plaque, which causes inflammation, and irritating factors, which favor plaque accumulation, are often present in the gingival environment.
This has led to the tendency to designate all forms of gingival disease as gingivitis, as if inflammation were the only disease process involved.
The role of inflammation in gingival diseases varies in three ways:
Inflammation may be the primary and only pathologic change. This is, by far, the most prevalent type of gingival disease.
Inflammation may be a secondary feature, superimposed on systemically caused internal disease. For example, inflammation commonly complicates gingival hyperplasia caused by the systemic administration of phenytoin.
Inflammation may be the precipitating factor responsible for clinical changes in patients with systemic conditions that of themselves do not produce clinically detectable gingival disease. Gingivitis in pregnancy is an example.
Types of gingival disease
Gingival inflammation may be localized in all gingiva (generalized gingivitis) and may be located on a part of gingiva (localized gingivitis). In cases when inflammation affected one or two interdental papillae it’s called papillitis.
The most common type of gingival disease is the simple inflammatory involvement caused by bacterial plaque attached to the tooth surface. This type of gingivitis, called chronic marginal gingivitis or simple gingivitis, may remain stationary for indefinite periods of time or may proceed to destroy the supporting structures (i.e., periodontitis). The reasons for these different behaviors are not clear.
These other types of gingival disease include the following:
- Acute necrotizing ulcerative gingivitis, as well as gingival changes seen in acquired immunodeficiency syndrome (AIDS) patients.
- Acute herpetic gingivostomatitis and other viral, bacterial, or fungal diseases.
- Allergic gingivitis.
- Skin diseases that also involve the gingival tissues, inducing characteristic types of gingival disease, such as in lichen planus, pemphigus, erythema multiforme, and other dermatoses.
- Gingivitis that is initiated by bacterial plaque, but in which the tissue response is modified by systemic factors. Such is the case with nutritional deficiencies, endocrine diseases such as diabetes, and conditions such as pregnancy, puberty, and hematologic and immunologic problems.
- Gingival enlargement, in which the gingival response to a variety of pathogenic agents results in an increase in volume. Drug-associated changes such as those induced by phenytoin, cyclosporine, and other drugs are included in this group.
- Different benign and malignant tumors may appear in the gingiva either as primary tumors or as metastases.
Diseases of the tooth-supporting structures
There are several different diseases that involve the tooth-supporting tissues. Many older classifications considered them in terms of the pathologic changes they produced (e.g., inflammatory, degenerative, or neoplastic). Although there are degenerative and neoplastic periodontal diseases, the most common disease, by far, is initiated by plaque accumulation in the gingivodental area and is basically inflammatory in character. Initially it is confined to the gingiva and is called chronic marginal gingivitis. Later the supporting structures become involved, and now the disease is termed periodontitis. There is a continuum of changes from marginal gingivitis to periodontitis, and the term periodontal disease has been used genetically to refer to the entire process and more specifically to refer to periodontitis. The term chronic destructive periodontitis, however, is more accurate designation for this disease.
The periodontal tissues can also be involved by other nosologic entities unrelated to plaque; many of these fall into the degenerative or neoplastic categories. These diseases often involve other organs or systems and are considered periodontal manifestations of systemic diseases; these may have their initiation in the gingival tissues, in the underlying supporting structures, or both.
Periodontitis
Periodontitis is the most common type of periodontal disease and results from extension of the inflammatory process initiated in the gingiva to the supporting periodontal tissues. Synonyms, which are not currently in use, include Schmutz pyorrhea (Gottlieb), paradentitis (Weski, Beck), paradentosis, periodontoclasia, pericementitis, parodontitis, alveolar pyorrhea, alveoloclasia, Riggs’ disease, and chronic suppurative periodontitis.
Periodontitis has been classified according to the rate of progression (slowly progressive and rapidly progressive) and according to the age at onset (adult periodontitis and early-onset periodontitis). Other forms are necrotizing ulcerative periodontitis and refractory periodontitis.
Classification of chronic destructive periodontitis
I. Periodontitis
A. Slowly progressive periodontitis.
B. Rapidly progressive periodontitis:
• Adult onset periodontitis.
• Early onset periodontitis:
a. Prepubertal periodontitis.
b. Juvenile periodontitis.
C. Necrotizing ulcerative periodontitis.
D. Refractory periodontitis:
II. Trauma from occlusion.
III. Periodontal atrophy.
IV. Periodontal manifestations of systemic diseases.
In Ukraine there is periodontal diseases classification by N. Danylevsky (1994):
I. Inflammatory diseases:
- Gingivitis.
This is mainly such forms as catarrhal, hypertrophic or ulcerous inflammation.
- Localised periodontitis.
This is such forms as catarrhal, hypertrophic or ulcerous inflammation.
II. Distrophic-inflammatory diseases:
- Generalized periodontitis:
- Chronic or exacerbative course.
- Degree of development: I, II, III degree.
- Periodontosis.
III. Progressive idiopathic diseases.
IV. Productive periodontal diseases.
Gingival inflammation (gingivitis)
Catarral gingivitis
It develops more often as a result of acute injury caused by fish bones, toothbrush bristle, dental instruments when treating teeth, etc. The most common local etiological factors are overhanging restorations edges and food impaction.
Acute catarrhal gingivitis. Patients often complain of pain, gum reddening and bleeding.
The act of discoloring at acute gingival inflammation differ in both nature and distribution from those at chronic gingivitis. The discoloration may be marginal, diffuse or patch-like, depending on the underlying exacerbation. Color changes according to the intensity of the inflammation. In all instances there is an initial bright red erythema.
On probing the hyperemia, edema, bleeding may be revealed. Some of the former stipping gingival papillae are lost.
Chronic catarrhal gingivitis. Thus, chronic inflammation intensifies red or bluish red; this is caused by vascular proliferation and reduction of keratinization owing to epithelial compression with the inflamed tissue. Venous stasis will add a bluish hue. Originally light red, the color changes to varying shades of red, reddish blue, and deep blue with increasing chronic inflammatory process. The changes start in the interdental papillae and gingival margin and spread to the attached gingiva.
Both chronic and acute inflammations produce changes in the normal firm and supple consistency of the gingiva. As noted, at chronic gingivitis both destructive (edematous) and reparative (fibrotic) changes coexist, and the consistency of the gingiva is determined by their relative predominance
Gingival enlargement (hypertrophic gingivitis)
Chronic inflammatory gingival enlargement is caused by prolonged exposure to dental plaque. Factors that favor plaque accumulation and retention include poor oral hygiene, abnormal relationships of adjacent teeth and opposing teeth, lack of tooth function, cervical cavities, overhanging margins of dental restorations, improperly contoured dental restorations or pontics, food impaction, irritation from clasps or saddle areas of removable prostheses, nasal obstruction, orthodontic therapy involving repositioning of teeth, and habits such as mouth breathing and pressing the tongue against the gingiva. In some cases inflammation initiated by dental plaque on background system diseases which include some hormonal conditions (e.g., pregnancy and puberty).
Hypertrophic gingivitis has chronic course and is rarely exacerbated. The enlargement is limited to interdental papillae or marginal gingiva.
Patients usually do not complain of pain, rarely it arises from mechanical irritants. Overgrowing gingival papillae densely fill interdental spaces. The gingival papillae tissue is mulberry shaped, firm, pale pink, and resilient, with a minutely lobulated surface. On probing bleeding may be revealed.
The gingival papillae enlargement may be traumatized by teeth-antagonists and interfere with occlusion. Depending on gingival enlargement the following degrees are distinguished: I degree – enlargement within the limits of 1/3 heights of tooth crown; II degree – within the limits of 1/2 and III degree – covers more than 2/3 heights of tooth crown.
Clinical features. Chronic inflammatory gingival enlargement arises as a slight ballooning of the interdental papillae and/or marginal gingiva. At the early stages it forms a life preserver-like bulge around the involved teeth. This bulge increases in size until it covers a part of the crown. The enlargement is usually papillary or marginal and may be localized or generalized. It progresses slowly and painlessly unless it is complicated by acute infection or trauma.
Gingival fibromatosis is a rare condition of undetermined etiology. It has been designated by such terms as gingivomatosis, elephantiasis, diffuse fibroma, familial elephantiasis, idiopathic fibromatosis, hereditary gingival hyperplasia, hereditary gingival fibromatosis, and congenital familial fibromatosis.
Clinical features. The enlargement affects the attached gingiva as well as the gingival margin and interdental papillae, in contrast to phenytoin-induced hyperplasia, which is often limited to the gingival margin and interdental papillae. The facial and lingual surfaces of the mandible and maxilla are usually affected, but the involvement may be limited to one of the jaws. The enlarged gingiva is pink, firm, and almost leathery in consistency and has a characteristic minutely pebbled surface. In severe cases the teeth are almost completely covered, and the enlargement spreads in oral vestibule. The jaws seem to be distorted because of the bulbous enlargement of the gingiva. Secondary inflammatory changes are common at the gingival margins.
Acute necrotizing ulcerative gingivitis (ANUG) is inflammatory destructive disease of the gingiva that has characteristic signs and symptoms.
Etiology (Bacterial Flora). Plaut and Vincent in 1894 and 1896, respectively, introduced the concept that necrotizing ulcerative gingivitis is caused by specific bacteria, namely, fusiform bacillus and spirochetal organism.
Local predisposing factors are: dental plaques, calculus, defects in dental restorations and prostheses, malocclusion, etc. A poor diet has been mentioned as a predisposing systemic factor in NUG and its sequelae in developing.
Clinical Features. Necrotizing ulcerative gingivitis most often occurs as an acute disease. Its relatively mild and more persistent form is referred to as subacute disease. Recurrent disease is marked by periods of remission and exacerbation. A reference is sometimes also made to chronic necrotizing ulcerative gingivitis.
Oral signs. Characteristic lesions are punched out, crater-like depressions at the crest of the interdental papillae, subsequently extending to the marginal gingiva and rarely to the attached gingiva and oral mucosa. The surface of the gingival craters is covered by a gray, pseudomembranous slough, demarcated from the remainder of the gingival mucosa by a pronounced linear erythema. In some cases, the lesions of the pseudomembrane surface are denuded, exposing the gingival margin, which is red, shiny, and hemorrhagic. The characteristic lesions may progressively destroy the gingiva and underlying periodontal tissues.
Spontaneous gingival hemorrhage or pronounced bleeding on the slightest stimulation are additional characteristic clinical signs. Other signs often found are: fetid odor and increased salivation.
Patients are usually ambulatory and have a minimum of systemic complications. Local lymphadenopathy and a slight elevation in temperature are common features of the mild and moderate stages of the disease. In severe cases there may be marked systemic complications such as high fever, increased pulse rate, leukocytosis, loss of appetite, and general lassitude. Systemic reactions are more severe in children. Insomnia, constipation, gastrointestinal disorders, headache, and mental depression sometimes accompany the condition.
In very rare cases, severe sequelae such as noma or gangrenous stomatitis have been described.
Gingivitis treatment
The treatment of acute gingival disease entails the alleviation of the acute symptoms and elimination of all other periodontal diseases, both chronic and acute, throughout the oral cavity. Treatment is not complete if periodontal pathologic changes or factors capable of causing them are still present. The most severe is necrotizing ulcerative gingivitis, therefore, its treatment is described below.
The treatment of NUG consists in: (1) alleviation of acute inflammation by reducing the microbial load and removal of necrotic tissue; (2) treatment of chronic disease either underlying the acute involvement or elsewhere in the oral cavity; (3) alleviation of generalized symptoms such as fever and malaise, and (4) correction of systemic conditions or factors that contribute to the initiation or progression of the gingival changes.
Sequence of Treatment
Treatment of NUG should follow an orderly sequence, according to specific steps in three clinical visits:
- Mouthrinse with a glassful of an equal mixture of 3 % hydrogen peroxide and warm water, chlorhexidine digluconate solution.
- Application of topical anesthetic: 2 % novocaine, lidocaine, prilocaine, articaine solution, etc.
- Removing necrotic tissue with application protheolitic enzymes (trypsinum, etc.).
- Antibacterial therapy: erythromycin (500 mg every 6 hours) or metronidazole (500 mg twice daily for 7 days).
- Anti-inflammatory therapy: ibuprofen, indomethacin, naproxen, ketorol, natri imefenaminatis, etc.
- Stimulation of regeneration: ascorbic acid (vitamin C), methyluracilum, etc.
- Stimulation of epithelization: vitamin A and its preparations (oleumrosae, etc.).
Systemic antibiotics and topical antimicrobials
Antibiotics are administered systemically only in patients with systemic complications or local adenopathy. Antibiotics are not recommended for NUG patients who do not have these complications. A large variety of drugs have been used in the treatment of NUG. Topical drug therapy is only an adjunctive measure; no drug, when used alone, can be considered complete therapy. When used, systemic antibiotics also reduce the oral bacterial flora and alleviate the oral symptoms, but they are only an adjunct to the complete local treatment that the disease requires. Patients treated by systemic antibiotics alone should be cautioned that the acute painful symptoms may recur after the drug is discontinued.
Generalized periodontitis
Periodontitis can develop from a pre-existing gingivitis in patients with compromised immune status, the presence of risk factors and pro-inflammatory mediators, as well as the presence of a predominately periodontopathic microbial flora. The inflammation of the gingiva may then extend into the deeper structures of the tooth-supporting apparatus. The consequences include destruction of collagen and loss of alveolar bone (attachment loss). The junctional epithelium degenerates into a “pocket” epithelium, which proliferates apically and laterally. A true periodontal pocket is formed. Such a pocket is a predilection site and a reservoir for opportunistic, pathogenic bacteria; these bacteria sustain periodontitis and enhance the progression of the disease processes.
Periodontitis is usually a very slowly progressing disease, which in severe cases – particularly when untreated – can lead to tooth loss. Enormous variation in the speed of progression of periodontitis is observed when one differentiates between individual patients. In addition to the quantity and composition of the bacterial plaque, individually varying influences also play important roles: patient’s systemic health, patient’s genetic constitution, psychically influenced immune response status, ethnic and social factors, as well as risk factors such as smoking and stress.
In the aggressive forms of periodontitis, the manifestation of tissue loss on individual teeth occurs in successive acute phases rather than in a gradual, chronic progression. Phases of progression and quiescence alternate. Destructive phases may occur rapidly one after another, or longer quiescent phases may be in noticeable.
Etiologic risk factors for gingival and periodontal diseases
Oral Hygiene. The strong positive association that exists between poor oral hygiene and gingival and periodontal disease makes poor oral hygiene the primary etiologic agent. Statistically as well as clinically, bacterial plaque is a primary etiologic factor for periodontal disease. Therefore, poor oral hygiene is important risk factor in highly susceptible individuals and is of less importance in individuals with strong host resistance.
The incidence and severity of periodontal disorders are lower in individuals who receive regular dental care. The prevalence and severity of disease increase in patients which neglect dental care.
Small amounts of plaque that are not discernible on the tooth surface may be detected by running a periodontal probe or explorer along the gingival third of the tooth. Another common method of detecting small amounts of plaque is the use of disclosing solutions
The strong association previously described between plaque and calculus and periodontal disease in its initial stages may be explained by the dynamics of plaque and gingivitis formation over time.
Microbiologic studies support the concept that chronic periodontitis is associated with specific bacterial agents. Microscopic examination of plaque from sites with periodontitis has consistently revealed elevated proportions of spirochetes. Cultivation of plaque microorganisms from sites of chronic periodontitis reveals high percentages of anaerobic (90 %) gram-negative (75 %) species.
The cause of gingival inflammation is bacterial plaque. Several factors previously considered to be of direct etiologic significance in periodontal disease are now known to act only by favoring plaque accumulation. These include calculus, faulty restorations, partial removable prostheses, and food impaction.
Although the acquired bacterial coatings have been demonstrated to be the major etiologic factor in periodontal disease, the presence of calculus is of great concern for clinician. The primary effect of calculus is not, as may have been originally thought, of mechanical irritation but of bacteria that cover it. However, these calcified deposits play major role in maintaining and accentuating periodontal disease by keeping plaque in close contact with the gingival tissue and creating areas where plaque removal is impossible.
Defects in dental restorations and prostheses, referred to as iatrogenic factors, are common causes of gingival inflammation and periodontal destruction. Inadequate dental procedures may also injure the periodontal tissues. Six characteristics of restorations and partial dentures are important from the periodontal viewpoint: margins of restorations, contours, occlusion, materials, design of removable partial dentures, and restorative procedures themselves.
Depending on its nature, malocclusion exerts a varied effect on the etiology of gingivitis and periodontal disease. Irregular alignment of teeth will make the plaque control difficult or even impossible. Uneven marginal ridges of contiguous posterior teeth have been found to have a low correlation with pocket depth, loss of attachment, plaque, calculus, and gingival inflammation.
Nutrition. The nutrients, that have been specifically associated with the periodontal tissues, are: vitamins A, B complex, C, and D, and calcium and phosphorus. Deficiencies in each of these nutrients and their effects on the periodontium have been clearly demonstrated in properly designed animal studies.
Protein deficiency also accentuates the destructive effects of local irritants and occlusal trauma on the periodontal tissues, but the initiation of gingival inflammation and its severity depend on the local irritants.
Hormonal disturbances may affect the periodontal tissues directly, as periodontal manifestations of endocrine diseases; modify the tissue response to plaque in gingival and periodontal diseases; or produce anatomic changes in oral cavity that may favor plaque accumulation or trauma from occlusion. Diabetes is an extremely important disease from the periodontal standpoint. A variety of periodontal changes have been described in diabetic patients, such as a tendency toward abscess formation, diabetic periodontoclasia, enlarged gingiva, sessile or pedunculated gingival polyps, polypoid gingival proliferations, and loose teeth.
In aged individuals, arteriosclerotic changes characterized – by intimal thickening, narrowing of the lumen, thickening of the media, and hyalinization of the media and adventitia, with or without calcification, are common in vessels throughout the jaws, as well as in areas of periodontal inflammation. Both periodontal disease and arteriosclerosis increase with age, and it has been hypothesized that the circulatory impairment induced by vascular – changes may increase the patient’s susceptibility to periodontal disease.
The clinical manifestations of periodontal diseases occur because of a complete interaction between the etiologic agents, in this case, specific bacteria found in dental plaque and the host tissues. There are many different factors which, locally or systemically, can influence the diseases course by modifying the process inherent in the bacterial-host interaction.
Clinical features of generalized periodontitis
Clinical features of generalized periodontitis can be presented in cardinal signs or complex of symptoms (I. Lucomsky, 1945).
They include:
- symptomatic gingivitis;
- periodontal pocket;
- trauma from occlusion (traumatic occlusion);
- progressive resorption of alveolar bone.
Symptomatic gingivitis develops on the background of other complex of symptoms. There are mainly such forms as catarrhal, hypertrophic or ulcerous inflammation. Catarrhal gingivitis develops in more than 70 % of patients with generalized periodontitis. Characteristic clinical features are: exudative inflammation of gingival mucosa, hyperaemia, epithelial cells desquamation, increasing vessels permeability, chronic or exacerbative course.
Another clinical feature of symptomatic gingivitis is hypertrophic gingivitis, mainly the granulating form. It is characterized by gingival enlargement, especially of interdental papillae, red or bluish red color, marked softness and friability, with ready fragmentation and bleeding when probing and pinpoint surface areas of redness and desquamation. The lesion is mulberry shaped, soft, red, and resilient, with a minutely lobulated.
Symptomatic ulcerative gingivitis usually has chronic course. Characteristic lesions are punched out, crater-like depressions at the crest of the interdental papillae, subsequently extending to the marginal gingiva and rarely to the attached gingiva and oral mucosa. The surface of the gingival craters is covered by a gray, pseudomembranous slough, demarcated from the remainder of the gingival mucosa by a pronounced linear erythema. In some cases, the lesions of the pseudomembrane surface are denuded, exposing the gingival margin, which is red, shiny, and hemorrhagic. The characteristic lesions may progressively destroy the gingiva and underlying periodontal tissues. Spontaneous gingival hemorrhage or pronounced bleeding on the slightest stimulation are additional characteristic clinical signs.
V-shaped symptomatic gingivitis develops in places with sustained severe mechanical irritation.
Periodontal pocket is one of the important clinical features of periodontal disease. Pockets can be classified as follows:
Gingival Pocket (Relative or False): This type of pocket is formed by gingival enlargement without destruction of the underlying periodontal tissues. The sulcus is deepened because of the increased bulk of the gingiva.
Periodontal Pocket (Absolute or True): This type of pocket occurs with destruction of the supporting periodontal tissues. Progressive pocket deepening leads to destruction of the supporting periodontal tissues and loosening and exfoliation of the teeth.
Trauma from occlusion. Trauma from occlusion may be a factor in determining the dimension and shape of bone deformities. It may be the second cause of periodontal destruction. Trauma from occlusion can result in bone destruction in the absence or presence of inflammation.
Trauma from occlusion is the occlusal interrelations of separate teeth groups or dental arches, which are characterized by supracontacts, interfering with closure in intercuspal position, uneven distribution of masticatory forces with pathologic teeth migration, pathological changes of periodontium, parafunctions of the masticatory musculature and temporomandibular joints.
Bone loss and bone destruction. The height of the alveolar bone is normally maintained by an equilibrium, regulated by local and systemic influences between bone formation and bone resorption. When resorption exceeds formation, bone height is reduced.
The level of bone is the consequence of past pathologic experiences, whereas changes in the soft tissue of the pocket walls reflect the present inflammatory condition. Therefore, the degree of bone loss is not necessarily correlated with the depth of periodontal pockets, the severity of ulceration of the pocket wall, or the presence or absence of pus.
After the inflammation reaches the bone by extension from the gingiva, it spreads into the marrow spaces and destroys the alveolar bone.
Alveolar bone resorption develops slowly and depends on its level resulting in different clinical symptoms: gingival recession and pathologic tooth mobility. Pathologic tooth mobility is important clinical feature of periodontal disease. The degrees of pathologic tooth mobility by D. Entin can be distinguished as follows: grade I – tooth mobility in vestibular-lingual direction; grade II – in vestibular-lingual and medial-distal direction; grade III – in vestibular-lingual, medial-distal direction and vertical direction.
Alveolar bone resorption leads to different degrees of gingival recession.
It is possible to define the approximate depth of resorption, which clinically depends on the size of gingival recession, however the most exactly it would be revealed by means of radiographic examination. The level of resorption of interdental septa is a clinical sign of pathologic process in periodontium. A few degrees of interdental septa resorption are distinguished: initial, I, II and III degree. At the initial degree the resorption of alveolar bone is insignificant and is not accompanied by atrophy of interdental septa, at I degree the resorption occupies one-third of the interdental septa; at II degree the loss of bone tissue extends to the half of the height of interdental septa, and at III degree the loss occupies more than 2/3 of the interdental septa heights.
Clinical features
The characteristic sings at chronic periodontitis are: gingival inflammation, which results in accumulation of plaque, and loss of periodontal attachment and alveolar bone, which in turn results in formation of a pocket. In many patients the gingival inflammation is not visible during the inspection and can be detected only when probing.
The disease is usually generalized, although some areas may be involved more deeply than others. Areas of deeper involvement are usually associated with poorer plaque control and can be found in relatively inaccessible sites such as furcation areas or malposed teeth.
Gingival bleeding, either spontaneous or easily provoked, is frequent, and inflammation-related exudate and suppuration from the pocket may also be revealed. When the pocket is sealed off, pus cannot drain, and an abscess may form. These localized areas of acute inflammation do not develop very often, but when they do, they need emergency care.
Pocket depths are variable, and both horizontal and angular bone loss can occur. Tooth mobility often occurs in neglected cases when bone loss is significant.
Symptoms. Chronic periodontitis is usually painless. Occasionally, exposed roots may be sensitive to the heat and/or cold in the absence of caries. Areas of localized dull pain, sometimes radiating deep into the jaw, are associated with chronic periodontitis. The presence of areas of food impaction may increase patient’ discomfort. Gingival tenderness or itching can also occur.
Acute pain may appear during the forming of periodontal abscess, and root caries or recurrent caries may result in pulpal symptoms.
Types. Mild periodontitis (I degree) is usually characterized by probing attachment loss of 2 to 4mm, minimal furcation invasions, and little tooth mobility. Along with various amounts of calculus supra – and subgingival plaque are present. Bleeding on gentle probing is frequently observed. Radiographic evidence of bone loss is minimal (usually less than 20 % of the total attachment). This stage of involvement can be localized to several teeth or generalized to many areas throughout the mouth.
Patients with moderate periodontitis (II degree) exhibit 4 to 7 mm of probing attachment loss, early to moderate furcation invasions, and slight to moderate tooth mobility. Radiographically evident bone loss is usually horizontal and may consist of up to 40 % of the total periodontal attachment on the tooth. Furcation radiolucencies may be evident. Bleeding on probing and purulence may be frequently observed.
Patients with severe periodontitis (III degree) have a probing attachment loss of 7 mm or more with significant furcation invasions, often through-and-through hole of the furcation. Excessive tooth mobility is usually observed. Radiographically evident bone loss exceeds 40 %, and angular bony defects are seen. Along with bleeding on probing purulent exudate can be present.
Radiographs in diagnosis of periodontal disease. The radiograph is a valuable aid in the diagnosis of periodontal disease, determination of the prognosis and evaluation of treatment outcome.
Radiographic changes in periodontitis:
- Fuzziness and a break in the continuity of the lamina dura at the mesial or distal aspect of the crest of the interdental septum have been considered as the earliest radiographic changes in periodontitis. These result from the extension of gingival inflammation into the bone causing widening of the vessel channels and reduction in calcified tissue at the septal margin.
- A wedge-shaped radiolucent area is formed at the mesial or distal aspect of the crest of the septal bone. The apex of the area is pointed in the direction of the root. This is produced by bone resorption of the lateral aspect of the interdental septum.
- The destructive process extends across the crest of the interdental septum and the height is reduced. Fingerlike radiolucent projections extend from the crest into the septum. They are the result of the deeper extension of the inflammation to the bone.
- The height of the interdental septum is progressively reduced by the extension of inflammation and the resorption of bone.
Treatment of periodontal diseases
General principles of treatment. Treatment of patients with periodontal diseases must be complex, purposeful and strictly individualized. It includs local and systemic treatment, effective conservative (medicamental), surgical, prosthetic, orthdontic and physical therapy methods and maintenance phase (recall). The complex treatment should generally be, primarily etiologic, pathogenetic and, finally, symptomatic.
The complex treatment of periodontal diseases may be divided into a few kinds or stages:
- Initial medication treatment (antibiotic coverage).
- Emergency treatment. Emergency procedures are performed in cases of acute necrotizing ulcerative gingivitis (ANUG), periodontal abscesses, periodontic-endodontic lesions (acute pulpitis, apical periodontitis), etc.
- Patient motivation and training to the rational oral hygiene.
- Complete elimination of all dental plaque, calculus, iatrogenic irritants and plaque-retentive areas; polishing root surfaces, old restorations, open furcations in multirooted teeth, etc.
Sequence of treatment. Following clinical examination and determination of prognosis a case presentation is made. The patient is informed about diagnosis, severity of disease, the necessity of treatment and phases of treatment. During the case presentation, dentists should begin to collect the subjective signs indicating the patient’s desire to cooperate.
Traumatic lesions of oral mucosa. Reasons. Clinic. Diagnostics. First aid
Mechanical injury
Acute mechanical injury (trauma mechanicum acutum) of mucosa membrane appears under the short-term strong influence – by chance with the biting, the impact or the injury by different objects. Most frequently mucosa membrane of the tongue, lips and cheeks along the line of teeth joining suffer. In this case at first pain appears, and on the place of injury hematoma, excoriation, erosion or ulcer can be formed. Frequently their sizes, form and localization on mucosa membrane coincide with the same of the traumatic agent.
Complaints:
- Insignificant pain, burning, smarting of mucous membrane in the region of the injury.
- Painful section of the mucous membrane changes its colour in the place of the injury.
- Slightly painful cyanotic formation, which arises after sudden injury. Sharp pain, bleeding from the damaged section.
Stages of the treatment:
- Elimination of the local traumatic factor and its consequences.
- Anesthetization.
- Antiseptic processing.
- Application of the epithelializing medicines.
Chronic mechanical injury (trauma mechanicum chronicum)
Complaints:
- sensation of discomfort, pain, swelling;
- frequent biting;
- presence of the old ulcer;
- growth in the hard palate, the gums, the tongue, under the prosthesis;
- whitish section of the mucous membrane in the place of the permanent traumatic factor.
Clinic:
- Lymph nodes are increased, painful during palpation. The manifestation of changes depends on gravity of the lesion.
- Inflammatory spot or erythema in the place of the injury.
- Localization of erosion corresponds to the traumatic agent, erosion is painful, localized on the hyperemized mucous membrane.
- Indolent ulcer is localized more frequently on the tongue, lips, cheeks along the line of teeth joining, and also in the limits of orthopaedic field. It is single, painful, surrounded with inflammatory infiltration, the bottom is most often uneven, covered with fibrinous fur. The decrease, the disappearance of painfulness, the appearance of papillary growths indicate about malignization.
- Papillomatous hyperplasia – papilloms with the soft, grainy, bright red surface under the prosthesis, they are more frequent localized in the region of the hard palate.
- With the habit to bite or to suck lips, tongue, and cheeks mucosa membrane (in essence along the line of teeth joining) acquires the unique form: it will swell, it has the white macerated surface in the form of either spots and large illegibly limited sections, or fringed form because of many small patches of the unevenly biting epithelium. Lesion has asymptomatic course, but during the deep removal the erosions are formed, they are painful in contact with chemical stimuli.
Treatment:
- The elimination of the traumatic agent.
- Anesthetization.
- Cleaning the surface of erosion and ulcer from the necrotic fur.
- Processing of ulcer and oral cavity by the solutions of the antiseptics.
- Stimulation of the epithelisation.
Chemical injury
Chemical damage (trauma chymicum) appears when chemical substances enter oral mucosa. It can be acute and chronic. Acute chemical damage appears when chemical substances with sufficiently high concentration enter oral mucosa. Most often this happens when using them erroneously at home, in industry, when attempting suicide, during a visit to a dentist. The burns of oral mucosa can arise during the contact with acids, alkalis, the use of arsenic paste, phenol, formalin, formalinresorcinol mixture, nitrate of silver. The clinical picture of lesion (hyperemia, edema, erosion, necrosis, and ulcer) depends on the nature of the chemical substance, its quantity, concentration and action time. With the burns of acids coagulation necrosis appears, with alkalis – colliquative necrosis (lesion is deeper and can affect all layers of soft tissues).
Clinic of the coagulation necrosis: Media damage:
- hyperemia;
- edema;
- necrosis of tissues;
- forming of dense necrotic film;
- erosion;
- ulcer in the limits of the layers of mucous membrane, rarely the necrosis of the part of the alveolar branch (in contact with arsenous acid);
- dense brown film (layer) is formed in contact with sulfuric acid, yellow – nitric, grey-white – other acids.
Clinic of the colliquative necrosis:
- hyperemia;
- edema;
- necrosis of tissues;
- forming of loose necrotic masses;
- deep ulcer, which affects all layers of mucous membrane.
Treatment
It is necessary to remove the damaging chemical substance at once and to wash the oral cavity with the dilute solution of the neutralizing agent. To treat acid burns soap water, 1 % lime water, burnt magnesia, 0.1 % solution of ammonium hydroxide (15 drops to the glass of water) are used. Alkalis is neutralized with 0.5 % solution of acetous or citric acid, and also with 0.1 % solution of hydrochloric acid (10 drops to a glass of water) and thus will stop further penetration of chemical substance into the tissues.
Further treatment of patients with chemical burns of oral mucosa carries out as treatment of the acute unspecific inflammatory process: prescribing anaesthetizing medicines, dilute solutions of the antiseptic medicines in the form of oral bathes, garglings, the accelerating epithelization medicines (1 % solution of citral or peach oil, metiluratsil ointment, vitamins A and E).
Infectious diseases of oral mucosa: ulcerous stomatitis, candidiasis of oral mucosa, viral lesions
Acute necrotizing ulcerative gingivitis
Acute necrotizing ulcerative gingivitis (ANUG) is an endogenous oral infection that is characterized by necrosis of the gingiva. Occasionally, ulcers of the oral mucosa also occur in patients with hematologic disease or severe nutritional deficiencies.
Studies have shown that the disease is accompanied by an overgrowth of organisms prevalent in normal oral flora and is not transmissible. The organisms most frequently mentioned as working symbiotically to cause the lesions are the fusiform bacillus and spirochetes. Plaque samples taken from ANUG patients demonstrate a constant anaerobic flora of Treponema spp, Selenomonas spp, Fusobacterium spp, and Bacteroides intermedius. The tissue destruction is thought to be caused by endotoxins that act either directly on the tissues or indirectly by triggering immunologic and inflammatory reactions.
Classic ANUG in patients without an underlying medical disorder is found most often in those between the ages of 16 and 30 years, and it is associated with three major factors:
- Poor oral hygiene with pre-existing marginal gingivitis or faulty dental restorations.
- Smoking.
- Emotional stress.
Systemic disorders associated with ANUG are diseases affecting neutrophils (such as leukemia or aplastic anemia), marked malnutrition, and HIV infection. Malnutrition-associated cases are reported from emergent countries where the untreated disease may progress to noma, a large necrotic ulcer extending from the oral mucosa through the facial soft tissues.
A fulminating form of ulcerative stomatitis related to ANUG is noma (cancrum oris), which predominantly affects children in sub-Saharan Africa. This disease is characterized by extensive necrosis that begins on the gingiva and then progresses from the mouth through the cheek to the facial skin, causing extensive disfigurement. The major risk factors associated with noma include malnutrition, poor oral hygiene, and concomitant infectious diseases such as measles. Living in close proximity to livestock is also believed to play a role, and Fusobacterium necrophorum, a pathogen associated with disease in livestock, has been isolated from over 85 % of noma lesions. The mortality rate without appropriate therapy exceeds 70 %.
Clinical manifestations
The onset of acute forms of ANUG is usually sudden, with pain, tenderness, profuse salivation, a peculiar metallic taste, and spontaneous bleeding from the gingival tissues. The patient commonly experiences a loss of the sense of taste and a diminished pleasure from smoking. The teeth are frequently thought to be slightly extruded, sensitive to pressure, or to have a “woody sensation.” At times they are slightly movable. The signs noted most frequently are gingival bleeding and blunting of the interdental papillae. The typical lesions of ANUG consist of necrotic punchedout ulcerations, developing most commonly on the interdental papillae and the marginal gingivae. These ulcerations can be observed most easily on the interdental papillae, but ulceration may develop on the cheeks, the lips, and the tongue, where these tissues come in contact with the gingival lesions or following trauma. Ulcerations also may be found on the palate and in the pharyngeal area. When the lesions have spread beyond the gingivae, blood dyscrasias and immunodeficiency should be ruled out by ordering appropriate laboratory tests, depending upon associated signs and symptoms.
The ulcerative lesions may progress to involve the alveolar process, with sequestration of the teeth and bone. When gingival hemorrhage is a prominent symptom, the teeth may become superficially stained a brown color, and the mouth odor is extremely offensive. The tonsils should always be examined since these organs may be affected. The regional lymph nodes usually are slightly enlarged, but occasionally the lymphadenopathy may be marked, particularly in children.
The constitutional symptoms in primary ANUG are usually of minor significance when compared with the severity of the oral lesions. Significant temperature elevation is unusual, even in severe cases, and, when it exists, other accompanying or underlying diseases should be ruled out, particularly blood dyscrasias and AIDS. HIV-infected patients with NUG have rapidly progressing necrosis and ulceration first involving the gingiva alone, and then NUP with the periodontal attachment and involved alveolar bone. The ulcerated areas may be localized or generalized and often are very painful. In severe cases, the underlying bone is denuded and may become sequestrated, and the necrosis may spread from the gingiva to other oral tissues.
Treatment
The therapy of ANUG uncomplicated by other oral lesions or systemic disease is local débridement. At the initial visit, the gingivae should be débrided with both irrigation and periodontal curettage. The extent of the débridement depends on the soreness of the gingivae. The clinician should remember that the more quickly the local factors are removed, the faster is the resolution of the lesions. Special care should be taken by the clinician to débride the area just below the marginal gingivae. Complete débridement may not be possible on the first visit because of soreness. The patient must return, even though the pain and other symptoms have disappeared, to remove all remaining local factors.
Treatment of ANUG is not finished until there has been a complete gingival curettage and root planing, including removal of overhanging margins and other predisposing local factors. After the first visit, careful home care instruction must be given to the patient regarding vigorous rinsing and gentle brushing with a soft brush. Patients should be made aware of the significance of such factors as poor oral hygiene, smoking, and stress.
Antibiotics are usually not necessary for routine cases of ANUG confined to the marginal and interdental gingivae. These cases can be successfully treated with local débridement, irrigation, curettage, and home care instruction including hydrogen peroxide (approximately 1.5 to 2 % in water) mouth rinses three times a day and chlorhexidine 12 % rinses. Antibiotics should be prescribed for patients with extensive gingival involvement, lymphadenopathy, or other systemic signs, and in cases in which mucosa other than the gingivae is involved. Metronidazole and penicillin are the drugs of choice in patients with no history of sensitivity to these drugs. Patients whose lesions have extended from the gingivae to the buccal mucosa, tongue, palate, or pharynx should be placed on antibiotics and should have appropriate studies to rule out blood dyscrasias or AIDS. After the disease is resolved, the patient should return for a complete periodontal evaluation. Periodontal treatment should be instituted as necessary. The patient must be made aware that, unless the local etiologic factors of the disease are removed, ANUG may return or become chronic and lead to periodontal disease.
Mycotic lesions
Candidiasis or candidomikosis of oral mucosa is the disease, caused by fungi – the saprophytes of the oral cavity (Candida albicans, C. pseudotropicalis, C. tropicalis, C. crusei, C. quilliermondi) – which with weakening the resistance of organism and barrier function of oral mucosa, with the development of dysbacteriosis become pathogenic.
The state of the decreased immunological reactivity can be caused by:
- action of antibiotics, corticosteroids and cytostatic means;
- irradiation;
- development of tumors;
- blood diseases;
- pathology of gastrointestinal tract;
- disturbance of exchange of substances (diabetes, hypovitaminoses);
- AIDS, etc.
Acute pseudomembranous candidiasis
Acute pseudomembranous candidiasis of oral mucosa (oral moniliasis; candidosis acuta, soor) develops in children’s infancy, weakened by infectious diseases, by bronchitis, dyspepsias, and also in premature children. It develops in older weakened by rachitis, exudative diathesis, hypovitaminoses, etc. Causative agent of oral moniliasis is Candida Albicans. Besides autoinfection, the infection can be transmitted through the mother’s nipples, contaminated dummy and baby food.
Clinic
In children’s infancy mother focuses attention on appearance of white spots or white coagulated fur, which in essence is accumulated in the retentional zones in the form of platelets or film (layer) on mucosa membrane of the cheeks, lips, the tongue, and the palate. If oral moniliasis is caused by Candida pseudotropicalis, fur has a foam nature.
With the mild course of oral moniliasis platelets are freely removed, leaving at its place the focus of hyperemia; with the severe – the centres of the stratification of fur merge into the continuous filmy surfaces, which in the course of time thicken and spread into all sections of oral mucosa. This fur is not easily scaled with scarifiness, and erythema, and sometimes – with bleeding erosions, revealed under it.
Acute atrophic candidiasis
Acute atrophic candidiasis (candidosis acuta atrophica) develops with the increased sensitivity of oral mucosa to the fungi of the class of Candida.
The clinical picture of acute atrophic candidiasis is characterized by xerostomia, fiery-red colour and burning of oral mucosa, absence of fur. Sometimes an insignificant number of crusts is formed on the red border of lips. If acute candidiasis is not treated, chronic (hyperplastic or atrophic) candidiasis develops.
Chronic hyperplastic candidiasis
Chronic hyperplastic candidiasis (candidosis chronica hyperplastica) develops in people, which assume cytostatics, antibiotics, in patients with tuberculosis, pathology of the blood, AIDS. It is characterized by appearance of white platelets, merging into the continuous coagulated bedding, which in the course of time thicken and become yellowish.
Depending on the topography of lesion candidiasis glossitis, cheilitis, angular cheilitis (perleche), palatinite are distinguished. The most frequently this disease occurs on mucosa membrane of the angles of mouth, on the back of tongue, the soft palate. Еhe course of chronic hyperplastic candidiasis is accompanied by dryness, hyperemia and edema of oral mucosa, the hypertrophy of the tongue papillae is possible in certain cases.
Chronic atrophic candidiasis
Chronic atrophic candidiasis (candidosis chronica atrophica) occurs more frequently in people, who use detachable plate prostheses and is characterized by reddening, edema, dryness and burning of mucosa membrane with the secretion of viscous saliva. The sufficiently frequent form of chronic atrophic candidiasis is candidiasis cheilitis (cheilitis candidosa) – the lesion of the entire surface of lips or its angular parts (candidiasis perleche).
Candidiasis cheilitis is characterized by edema, hyperemia, thinning, dryness of red border, with certain deepening of the transversely located grooves, with formation and rejection of fish-scales of different value from the surface of the lips.
Candidiasis perleche is characterized by maceration of skin in the area of angles of mouth, the presence of cracks, covered with a white coating, and also the burning and the pain when opening the mouth.
The treatment of candidiasis of oral mucosa is intended to eliminate the clinical signs of disease, remove the prerequisites of the development of fungi and appearance of candidiasis and increase of the resistibility of organism.
Viral lesions
Herpetic infection – one of the most common and not controlled viral infections of man is caused by the virus of herpes simplex.
The development of herpetic vesicle has 4 stages:
- Appearance of the hyperemized section on the skin and mucous membranes accompanied by more or less expressed sensation of burning, itch of numbness or tingling;
- Formation of vesicles in several hours after the appearance of hyperemia. Vesicles have semi-circling form and are filled with transparent contents, which then grow turbid, vesicular stage lasts from 4 to 7 days and is frequently accompanied by more or less expressed adenopathy;
- Formation of crusts from the scaled epidermis after vesicle collapse and its release from the contents. The zone of vesicle is hyperemized, sometimes edematic. On oral mucosa the erosions remain, which can for a second time be infected;
- Recovery. Crusts are separated and droped off. At the places of precipitations, which rapidly passed, the reddening remains.
Chronic recurrent herpes
After the transferred primary herpetic infection the virus remains in the human organism, obviously, during the entire life. Disease passes into the latent phase of prolonged virus carrying, which is frequently accompanied by relapses – a recurrent form. In oral cavity – this is chronic recurrent herpetic stomatitis, gingivostomatitis, recurrent herpes of lips and herpetic recurrent ganglionevritis.
Chronic recurrent herpes occur predominantly in adult and each tenth child (12.5 %), who had primary herpetic infection.
Fairly often, regardless of the season, and no matter how much time passed since the previous precipitation, relapse occurs after injuries (injection, the imposition of matrix, biting, separation and dental treatment for orthopedic purposes), supercooling, acute respiratory disease, acute respiratory viral disease, or a clear connection with the menstrual cycle, and the exacerbation of the chronic diseases of gastrointestinal tract is established.
Recurrent herpes of oral mucosa is more frequently localized on the hard palate, cheeks, the tongue. Precipitations are limited, with the typical dynamics of the process: vesicles appear in clusters, merge, burst, forming erosion with the polycyclic outlines. In the first twenty-four hours of existence the erosions are very painful and accompanied by the painful reaction of lymph nodes. The general state of patients, as a rule, is not disrupted.
Depending on the frequency of relapses the forms of recurrent herpes are distinguished:
- mild (1–2 relapses for a period of 3 years);
- moderate (1–2 relapses in 1 year);
- severe (4–5 relapses in a year or permanently).
A cytological examination reveals the neutrophilic leukocytes of different degree of dystrophia, and also the layers of epithelial cells with the phenomena of polymorphism and cell-monsters (gigantic polynuclear cells of herpes, the so-called cells of the ballooning degeneration).
Varicella-zoster virus infection
Varicella zoster virus (VZV) is a herpes virus, and, like other herpes viruses, it causes both primary and recurrent infection and remains latent in neurons present in sensory ganglia. VZV is responsible for two major clinical infections of humans: chickenpox (varicella) and shingles (herpes zoster [HZ]).
Chickenpox is a generalized primary infection that occurs the first time an individual contacts the virus. This is analogous to the acute herpetic gingivostomatitis of herpes simplex virus. After the primary disease is healed, VZV becomes latent in the dorsal root ganglia of spinal nerves or extramedullary ganglia of cranial nerves. A child without prior contact with VZV can develop chickenpox after contact with an individual with HZ. In 3 to 5 of every 1,000 individuals, VZV becomes reactivated, causing lesions of localized herpes zoster. The incidence of HZ increases with age or immunosuppression.
Patients who are immunocompromised due to HIV disease, cancer chemotherapy, immunosuppressive drug therapy, or hematologic malignancy have an increased susceptibility to severe and potentially fatal HZ. These HZ infections may be deep-seated and disseminated, causing pneumonia, meningoencephalitis, and hepatitis; however, otherwise normal patients who develop HZ do not have a significant incidence of underlying malignancy.
Clinical manifestations
General Findings. Chickenpox is a childhood disease characterized by mild systemic symptoms and a generalized intensely pruritic eruption of maculopapular lesions that rapidly develop into vesicles on an erythematous base. Oral vesicles that rapidly change to ulcers may be seen, but the oral lesions are not an important symptomatic, diagnostic, or management problem. HZ commonly has a prodromal period of 2 to 4 days, when shooting pain, paresthesia, burning, and tenderness appear along the course of the affected nerve. Unilateral vesicles on an erythematous base then appear in clusters, chiefly along the course of the nerve, giving the characteristic clinical picture of single dermatome involvement. Some lesions spread by viremia occur outside the dermatome. The vesicles turn to scabs in 1 week, and healing takes place in 2 to 3 weeks. The nerves most commonly affected with HZ are C3, T5, L1, L2, and the first division of the trigeminal nerve.
When the full clinical picture of HZ is present with pain and unilateral vesicles, the diagnosis is not difficult. Diagnostic problems arise during the prodromal period, when pain is present without lesions. Unnecessary surgery has been performed because of the diagnosis of acute appendicitis, cholecystitis, or dental pulpitis. A more difficult diagnostic problem is pain caused by VZ virus without lesions developing along the course of the nerve (zoster sine herpete; zoster sine eruptione). Diagnosis in these cases is based on clinical symptoms and serologic evidence of a rising antibody titer.
HZ may also occasionally affect motor nerves. HZ of the sacral region may cause paralysis of the bladder. The extremities and diaphragm have also been paralyzed during episodes of HZ. The most common complication of HZ is postherpetic neuralgia, which is defined as pain remaining for over a month after the mucocutaneous lesions have healed, although some clinicians do not use the term postherpetic neuralgia unless the pain has lasted for at least 3 months after the healing of the lesions. The overall incidence of postherpetic neuralgia is 12 to 14 %, but the risk increases significantly after the age of 60 years, most likely due to the decline in cell-mediated immunity.
Oral findings. Herpes zoster involves one of the divisions of the trigeminal nerve in 18 to 20 % of cases, but the ophthalmic branch is affected several times more frequently than are the second or third divisions. HZ of the first division can lead to blindness secondary to corneal scarring and should be managed by an ophthalmologist. Facial and intraoral lesions are characteristic of HZ involving the second and third divisions of the trigeminal nerve. Each individual oral lesion of HZ resembles lesions seen in herpes simplex infections. The diagnosis is based on a history of pain and the unilateral nature and segmental distribution of the lesions. When the clinical appearance is typical and vesicles are present, oral HZ can be distinguished clinically from other acute multiple lesions of the mouth, which are bilateral and are not preceded or accompanied by pain along the course of one trigeminal nerve branch.
HZ has been associated with dental anomalies and severe scarring of the facial skin when trigeminal HZ occurs during tooth formation. Pulpal necrosis and internal root resorption have also been related to HZ. In immunocompromised patients, large chronic HZ lesions have been described that have led to necrosis of underlying bone and exfoliation of teeth. HZ of the geniculate ganglion, Ramsay Hunt syndrome, is a rare form of the disease characterized by Bell’s palsy, unilateral vesicles of the external ear, and vesicles of the oral mucosa. Because oral lesions occurring without facial lesions are rare, isolated oral HZ can be misdiagnosed, particularly when erythema, edema, and nonspecific ulceration are seen without the presence of intact vesicles. In these cases, a cytology smear or viral culture is often necessary for diagnosis. An incorrect diagnosis can be made when prodromal pain is present prior to the appearance of the characteristic lesions. During this period, endodontic therapy, extractions, or other surgery may be performed unnecessarily. Similar problems occur in zoster sine eruptione.
Treatment
Management should be directed toward shortening the course of the disease, preventing postherpetic neuralgia in patients over 50 years of age, and preventing dissemination in immunocompromised patients. Acyclovir or the newer antiherpes drugs valacyclovir or famciclovir accelerate healing and reduce acute pain, but they do not reduce the incidence of postherpetic neuralgia.35 The newer drugs have greater bioavailability and are more effective in the treatment of HZ. The use of systemic corticosteroids to prevent postherpetic neuralgia in patients over 50 years of age is controversial; a recent review of the data indicated a reduction of pain and disability during the first 2 weeks but no effect on the incidence or severity of post-herpetic neuralgia. Some clinicians advocate the use of a combination of intralesional steroids and local anesthetics to decrease healing time and prevent postherpetic neuralgia, but a controlled study of this therapy has not been performed. Effective therapy for postherpetic neuralgia includes application of capsaicin, a substance extracted from hot chili peppers.
Topical capsaicin is safe but must be used for a prolonged period to be effective and may cause a burning sensation of the skin. When topical capsaicin therapy is ineffective, use of a tricyclic antidepressant or gabapentin is indicated. Chemical or surgical neurolysis may be necessary in refractory cases.
AIDS
AIDS syndromum immunodefectionis aguisitae – the syndrome of the acquired immunodeficiency is contagious immunological disease of virus etiology.
Etiology
AIDS is caused by virus from the family of the retroviruses of the subfamily of lentiviruses named by taxonomical committee of WHO (World Health Organization) HIV (Human immunodeficiency virus).
The mechanism of AIDS consists in the destruction by the virus of the immune system as a result of the infection and the loss of the T-helpers (T4), on cytoplasmic membrane of which there is the protein CD-4, which serves as receptor for HIV. With the introduction into the cell the virus changes it irreversibly, using genetic material of a cell for its own reproduction: formed DNA is included in the chromosomes of cells and is converted into provirus, which can exist in the inactive form or appear itself, synthesizing virus proteins. Becoming more active (during the total weakening of immunity), HIV begins to multiply rapidly, seizing T-helpers and causing their loss. As a result disruptions of equilibrium in the system T-helpers – T-supressors the latter begin to suppress immunity. Besides quantitative changes, in the system of T-lymphocytes the qualitative changes begin. The mechanism of the suppression of cellular immunity includes cytopathic action HIV, toxic action of its components, and also cytotoxic action of macroorganism on its own CD-4 the fraction of the T-lymphocytes, which acquired antigenic properties. On this background the opportunistic infections, whose development composes the clinical picture of AIDS, attack the defenceless organism.
Clinic
The existence of phases of course is characteristic for AIDS. The duration of incubative period varies from several (6–8) months to several years. Approximately for 50 % of patients it is 4 years.
CDC-centre (Georgia, the USA) and WHO (1988) proposed the following classification of the clinical stages of AIDS:
- Incubation.
- Acute HIV-infection.
- Virus carrying: a) the persisting infection; b) generalized infection.
- Lymphadenopathy.
- AIDS-associated complex.
- AIDS with the development of infection and tumors.
The classification of V. I. Pokrovskj (1989) distinguishes 4 stages in the course of the HIV-infection:
- Incubation.
- Stage of the primary manifestations: a) the phase of acute fever; b) asymptomatic phase; c) persisting generalized lymphadenopathy.
- Stage of secondary diseases:
- A. The loss of body mass is less than 10 %, the superficial fungus, bacterial or viral lesions of the skin and the mucous membranes, herpes Zoster, recurrent pharyngitis, sinusitises.
- B. Progressive loss body mass is more than 10 %, unexplained genesis diarrhea, fever for more than 1 months, hairy leukoplakia, pulmonary tuberculosis, repeated or steadfast bacterial, fungal, viral and protozoal lesions of the skin and the mucous membranes, repeated or disseminated herpes zoster, localized Kaposi’s sarcoma.
- C. The generalized bacterial, viral, protozoal parasitic diseases, pneumocystic pneumonia, candidiasis of the gullet, atypical micobacteriosis, extrapulmonary tuberculosis, cachexia, the disseminated Kaposi’s sarcoma, CNS lesions of different etiology.
- Terminal stage.
Reflill and Bourke (1988), as objective basis for spread of symptoms and stages of disease, development of its gravity, propose to use a number of T4 lymphocytes in 1 mm3 of the blood and the stages are the following:
- Incubation.
- Asymptomatic.
- Chronic lymphadenopathy for a period of 3–5 years – pre-AIDS.
- The subclinical disturbances of the immunity (in 1 mm3 of the blood – contained 400 T4-lymphocytes).
- The appearance of allergic reactions to the skin tests (the number of T4-lymphocytes in 1 mm3 of the blood is less than 300).
- Immunodeficiency followed by lesion of the skin and mucous membranes – absence of hypersensitivity of the delayed action (the number of T4-lymphocytes < 200).
- The generalized manifestations of immunodeficiency – HIV-indicator opportunistic infections and malignant tumors are developed (T4-lymphocytes < 100).
The clinical picture of AIDS, first of all, is caused by the T-cell immune deficiency. Reduction in the activity of immune system leads to the activation of saprophytic microflora.
The first manifestation of AIDS after being infected is a lesion of oral mucosa.
Rapidly progressive parodontitis, acute ulceronecrotic gingivostomatitis, angular cheilitis are observed. Centres in the periodontium tend to cause osteomyelitis. Fairly often a violent reaction to the endodontic interferences is developed. The appearance of these signs can indicate a problem for the persons of the risk group long before manifestations of candidiasis and hairy leukoplakia.
Depending on the frequency of distribution the diseases of oral mucosa are distinguished as follows: candidiasis (88 %), herpetic lesions (11–17 %), xerostomia (19–28 %), exfoliative cheilitis (9 %), ulcers (7 %), desquamative glossitis (6 %), hairy leukoplakia (5 %), the Kaposi’s sarkoma (from 4 to 50 %), hemorrhage.
Candidiasis of oral mucosa in case of AIDS has several forms: pseudo-membranous, at which a significant number of soft white centres are observed, which resemble flakes of the curdled milk and which can be easily removed by means of scarifying; hyperplastic – it resembles leukoplakia, accompanied by dense white lesions, soldered with the surface of the oral mucosa, and atrophic (erythematous). With this form the erythematous spots without the fur appear, on the background of which in some places the spots of hyperkeratosis can be revealed.
Among the bacterial infections fusospirochetosis takes place, which causes acute ulceronecrotic gingivitis in the frontal section. It occurs in patients with AIDS, carriers of antibodies, and seropositive persons. In the latter, furthermore, in the periapical tissues the exacerbations of the centres of secondary infection appear, and in the parodontium destructive changes are possible, up to the sequestration of the alveolar bone.
Secondary virus agents cause hairy leukoplakia. This group includes herpes viruses, welding dribbles and condylomas. Hairy leukoplakia resembles the mild form of leukoplakia and whitish hair growths, which cannot be removed by scaling. They are mainly located along the edge of the tongue and sometimes they resemble chronic hyperplastic candidiasis. Ulcers and aphthae in the oral cavity in case of AIDS are more frequently localized on the palate and are caused by Cryptococcus neoformans (yeast, that gemmate and does not form mycelium). Single mucous capsules sometimes are observed.
In homosexuals the early (first) manifestation of AIDS in the oral cavity are: painful ulcers on mucous membrane of the palate and the tongue, connected with the cytomegalovirus infections (group of the herpes viruses), with a characteristic slow protracted course, recurrence, the absence of the effectiveness of treatment with using conventional procedures. Simultaneously the ulcerous-herpetic lesions of lips in Klein’s zone, and also on mucous membrane of the nose are observed. It is established that all early manifestations of AIDS in the oral cavity are steady and are difficult to treat.
Vascular tumor – Kaposi’s sarcoma is the transmissible disease, which is characterized by multiple pigmented lesions. In patients with AIDS it is observed mainly in the oral cavity before the palate in 76 % of cases and is characterized by exophytic growth, painlessness, friable consistency (in the form of soft cyanotic nodule), high frequency of malignancy. Soft tissues have color from brown to bluish-red.
Berkitt’s lymphoma is localized on the lower jaw. Before its formation patients complain about the toothache, mucosal ulceration, growth of the submaxillary lymph nodes.
The resorption of the bone tissue at this time is roentgenologically observed.
In those, who abuse smoking, the epidermoid carcinoma is observed, which is localized on the tongue or at the bottom of the oral cavity. With AIDS other new formations develop – lymphoreticular sarcoma, planocellular cancer, etc. Radiation and chemotherapy of the described new formations in case of AIDS are ineffective.
Diagnostics
Early diagnostics of AIDS is extremely important, since the latent period between infection and appearance of clinical signs of AIDS can be sufficiently prolonged.
Taking into account the complexity of laboratory diagnostics at the proposal of WHO (World Health Organization) in certain cases the diagnosis of AIDS can be based on clinical symptomatology. All clinical symptoms are proposed to divide into two groups – serious and insignificant (WHO, 1986).
In adults AIDS is diagnosed in the presence of minimum two serious symptoms coupled with at least one insignificant symptom in the absence of apparent reasons for immunosuppression, such as cancer, the severe form of the alimentary insufficiency of nourishment and other states of the established etiology.
- Serious symptoms:
- decrease in body weight to 10 % and more;
- chronic diarrhea more than 1 month;
- fever lasting more than 1 month (interrupting or constant).
- Insignificant symptoms:
- persistent cough lasting more than 1 month;
- generalized multi-focal dermatitis;
- recurrent herpes Zoster;
- candidiasis of the oral cavity and throat;
- chronic progressive and disseminated herpes simplex;
- generalized lymphadenopathy.
When only Kaposi’s sarcoma or cryptococcal meningitis is present, the diagnosis of AIDS is established.
Indications for consideration of AIDS are:
- Malignant new formations (Kaposi’s sarcoma, lymphoma).
- Infections:
- Fungi: a) candidiasis, which involves oral mucosa, causing dysfunction of esophagus; b) cryptococcosis, which causes the diseases of lungs, CNS and the scattered infection.
- Bacterial infections (“atypical” micobacteriosis, caused by the forms, which differ from the agents of tuberculosis and leprosy).
- Viral infections: a) the cytomegalovirus, which causes the diseases of lungs, gastrointestinal tract, CNS; b) the herpes virus, which causes the chronic infection of mucous membranes ulcers, elevated temperature for a month and more; c) the progressive encephalopathy considered to be caused by papovavirus; d) viruses HTFV, which lead to the malignant regeneration of T-cells.
- Simplest and the helminths: a) pneumonia, caused Pneumocystis carinii; b) the toxoplasmosis, which causes pneumonia or lesion of CNS; c) cryptosporidiosis, which causes intestinal diarrhea for more than one month; d) strongiloidosis.
There are 3 methods to prove the presence of virus in the organism: the cultivation of virus, identification of virus antibodies, and development of caption of antibodies to virus antigens (test ELISA – enzime linked immunosorbent assay).
Treatment
For dealing with AIDS new approaches are developed. They are based on the basic researches, connected with the concepts, which have appeared recently and are develop rapidly, and also on the new technologies (intracellular immunity, genetic therapy). These technologies concerning AIDS develop in three directions.
The first direction is based on the injecting of the gene, which synthesizes the product, which then is separated from the cells.
Another direction is connected with the synthesis of peptide. They do not exceed the limits of cells and competitorily block key processes in development of HIV. The third direction is based on injecting into the cells of the genes, which code antisenses and ribozyms, which respectively block or destroy RNA virus.
Among the medicines, which are registered in the arsenal of preparations for treating this contingent of patients, besides azidothymidine ([AZT]), are widely used suromin, NRA-23, atsiclovir, correctors of immunity (interleukin-2, gamma globulin, the stimulator of the function of T-lymphocytes, isoprinosine). To maintain the immune status the bone marrow transplantation is conducted.
The basic thing for the stomatologist during the treatment of such patients is rendering to symptomatic therapeutic aid and the sanitation of the oral cavity.
Forecast
The determination of the level of T-helper lymphocytes and relationship of T4/T8 have a very important significance for the forecast of AIDS. When the level of T4 is less than 200 in 1 mm3 of the blood, mortality exceeds 50 % in the first year after the manifestation of the clinical symptoms of AIDS. Spontaneous remission is not described. Disease persistently progresses and causes death.
Manifestations of specific infection (syphilis, tuberculosis) on oral mucosa
Syphilis
Syphilis is a classic disease with protean manifestations. There has been a significant rise in the prevalence of syphilis both in the developed and developing world during the past two decades, mainly as a disease associated with HIV infection and sexual promiscuity. The disease is caused by T. pallidum, the syphilis spirochete. There is a very high likelihood of human to human transmission of syphilis through unprotected sexual activity.
Syphilis has an incubation period of 10 to 90 days (average 3 weeks) and is characterized by four main clinical stages: primary, secondary, tertiary, and late or quaternary.
Primary Syphilis
After the inital exposure to infection with T. pallidum, the spirochetes pass through the mucous membrane or skin and are then carried in the blood throughout the body. After an incubation period of about 3 to 4 weeks, there develops, at the site of entry, an ulcerated lesion called a primary chancre: a flat, red, indurated, highly infectious ulcer with serous exudate. The typical lesion is painless, und edema of the surrounding tissues is usually present. The regional lymph nodes become enlarged about 2 weeks after the appearance of the chancre and on examination are firm, painless, and discrete, with a rubbery consistency. The chancre disappears spontaneously within 3 to 8 weeks.
Secondary Syphilis
Approximately 2 months after healing, the secondary stage of syphilis usually develops, and in about one-third of patients, the primary chancre may be present at the same time. The signs of secondary syphilis are variable: generalized skin lesions in about 75 % of cases, mucosal ulcers in about 33 % of cases, generalized lymphadenopathy in about 50 % of cases, and systemic symptoms that are “influenza like”, including fever, headache, malaise, and general aches and pains. The skin lesions are found predominantly on the face, hands, feet, and genitalia and appear as dull red macular or papular spots.
Tertiary Syphilis
Reactivation of syphilis can occur at any time 2 or 3 years after the date of first infection, but such late lesions of syphilis are rarely seen today. The characteristic lesion is the gumma, which is usually localized, single or multiple, varying in size from a pinhcad to a lesion several centimeters in diameter. Gummas develop in the skin, the mucous membranes, and bones. These lesions are not infective as the tissue damage is due to a delayed type of hypersensitivity. The other organs involved in tertiary syphilis are the cardiovascular system and the nervous system.
Late or Quaternary Syphilis
This condition is seen one to two decades after primary syphilis. The two main clinical forms of late syphilis are cardiovascular syphilis and neurosyphilis, with resultant pathology of the aorta and the nervous system, respectively.
Latent Syphilis
This may be seen in some after many years without any symptoms. The disease lies dormant, without any clinical signs (except for positive serology), and may manifest as cardiovascular or neurosyphilis.
Congenital Syphilis T. pallidum
Is one of the few microorganisms that has the ability to cross the placental barrier; thus, the fetus may be infected during the second or third trimester from a syphilitic mother (either in the primary or secondary stage of syphilis). The disease will manifest in the infant as either (1) latent infection – no symptoms but positive serology; (2) early infection – lesions such as skin rashes, saddle nose, bone lesions, and meningitis appear up to the end of the second year of age; or (3) late infection – after the second year of age; lesions include Hutchinson’s incisors (notching of incisor teeth), mulberry molar teeth (due to infection of the enamel organ in the fetus), interstitial keratitis, bone sclerosis, arthritis, and deafness.
Oral considerations
Primary Syphilis. The normal site for the chancre is on the genitalia, but extragenital primary lesions occur in about 4 to 12 % of patients with syphilis. A chancre of the lip is the most common extragenital lesion, accounting for about 60 % of cases, and may present at the angles of the mouth. Most chancres in the male tend to be located in the upper lip and in the female on the lower lip. Other sites affected are the tongue and, to a lesser extent, the gingivae and tonsillar area. Intraoral chancres are usually slightly painful due to secondary bacterial infection, as are the enlarged lymph nodes in the submaxillary, submental, and cervical regions. The lesions are infectious, and transmission may occur by kissing, unusual sexual practices, and even intermediate contact with cups, glasses, and eating utensils. The differential diagnosis of primary syphilis includes ruptured vesicles of herpes simplex, traumatic ulcers, and carcinoma.
Secondary Syphilis. Characteristic slightly raised, grayish white, glistening patches on the mucous membrane, so-called “mucous patches”, of the tongue, soft palate, tonsil, or cheek but rarely the gingival tissues are common in the secondary stage. Lesions on the larynx and pharynx may lead to hoarseness. The surface of these lesions is covered with a grayish membrane, which can be easily removed and contains many spirochetes. The ulcers may coalesce to give the characteristic “snail tracks” and mucous patches in about a third of those affected. These lesions, like the primary chancre, are highly infectious. Maculopapular eruptions have been described in the mouth and are confined mainly to the palate, but, occasionally, the entire oral mucosa may be involved. In recent years, the secondary syphilitic lesions found in the mouth have been noted as often atypical, due, in many cases, to inadequate treatment as a result of antibiotic therapy for an unrelated infection. Other manifestations are generalized lymphadenopathy and condylomata (warts) of the anus and vulva; rarely, periostitis, arthritis, and glomerulonephritis may be seen. The differential diagnosis of secondary syphilis includes aphthous ulcers, erythema multiforme, lichen planus, and tonsillitis. The secondary-stage lesions heal 2 to 6 weeks after the time they first appear.
Tertiary Syphilis. The representative lesion of this stage is the “gumma”, which begins as a small, pale, raised area of the mucosa that ulcerates and rapidly progresses to a large zone of necrosis with denudation of bone and in the case of the palate may eventually perforate into the nasal cavity. The most common site for gumma formation is the hard palate, although the soft palate, lips, tongue, and face may be involved. The palatal lesions are usually midline, and in rare cases, the soft palate may be involved. Gummas are painless and have no infectivity.
Occasional cases of syphilitic osteomyelitis involving the mandible and, less commonly, the maxilla have been described. This condition represents a gummatous involvement of bone with extensive necrosis. The condition is characterized by pain, swelling, suppuration and sequestration, and both clinically and radiographically, the condition may resemble pyogenic osteomyelitis. If the lesion ossifies, then the radiographic appearance of the affected area may be similar to that of an osteogenic sarcoma.
Atrophic or interstitial glossitis is another oral manifestation of tertiary syphilis. Clinically, there is atrophy of the filiform and fungiform papillae, which results in a smooth, sometimes wrinkled lingual surface. This appearance is probably due to obliterative endarteritis of the lingual vasculature, leading to circulatory deficiency. Loss of the protective papillae subjects the dorsum of the tongue to many noxious stimuli, and leukoplakia frequently develops. The relationship between syphilitic glossitis and carcinoma of the tongue is not clear.
Syphilis very rarely affects the salivary glands, but both secondary and tertiary lesions have been described in the parotid glands. The other main salivary glands have also been involved either on their own or together with the parotid. Patients with general paresis of the insane may have perioral tremors and fine irregular tremors of the tongue and fingers. Although an association between oral squamous cell carcinoma and syphilis has been suggested in early studies, this relationship remains unproven.
Congenital Syphilis. The dental lesions of congenital syphilis are a result of infection of the developing tooth germ by T. pallidum. Since the deciduous teeth are usually well developed by the time the spirochetes invade the developing dental tissues, these teeth are minimally affected. The permanent teeth are at an early stage of development, and infection may result in the complete failure of development of a tooth or the production of malformed teeth. Early oral manifestations include diffuse maculopapular rash, periostitis (frontal bossing of Parrot), and rhinitis, whereas late features, manifesting at least 24 months after birth, comprise the hutchinsonian triad of interstitial keratitis of the cornea, sensorineural hearing loss, and dental anomalies. The most common dental manifestation of congenital syphilis is the so-called “mulberry molar” teeth, which are highly suggestive of prenatal syphilis. The first permanent molar teeth are usually involved and have roughened, dirty, yellow, hypoplastic, occlusal surfaces with poorly developed cusps and are smaller in size than normal. Hutchinson’s incisors are another manifestation of congenital syphilis. The upper central incisors are usually involved and have crescentic notches in the middle of their incisal edge. The tooth tends to be wider gingivally than at the incisal edge, giving a “screwdriver” appearance. The lower incisors show similar defects, but they are affected much less often than their maxillary counterparts. Of note, the maxillary incisors are more commonly affected than the mandibular ones. Infection of the developing bones of the face may lead to permanent facial deformities, which produce an open bite and a “dished” appearance to the face. Skin around the lips may show yellow discoloration soon after birth, leading to crack formation and eventual (Parrot’s) radial scars – rhagades – of the lips. Other, less common orofacial features include atrophic glossitis and a high, narrow palatal vault.
Diagnosis and Management
Exudate from primary or secondary lesions may be collected in fine capillary tubes and examined using dark-ground microscopy for typically motile T. pallidum. This technique has limited value in lesions affecting the mouth since the oral commensal Treponema microdentium closely resembles T. pallidum. However, specific immunofluorescence tests, if available, are helpful in diagnosis.
The laboratory diagnosis of syphilis is usually made by serology since T. pallidum cannot be routinely cultured in vitro. Ten milliliters of venous blood is sufficient to carry out all the serologic tests for syphilis. It is usual to carry out at least two different tests on each specimen of serum, and the interpretation of these complex test results should be left to an expert in genitourinary infections. Antigens used for syphilis serology are of two types: treponemal antibody-absorption test (FTA-Abs), which detects both IgM and IgG antibody, and ELISA. The last is increasingly used as a screening test to detect IgG antibody, although some false positives may result.
Differential Diagnosis
Primary and secondary syphilis include candidiasis, leukoplakia, hairy leukoplakia, lichen planus, aphthous ulcers, herpetic gingivostomatitis, erythema multiforme, TB, and trauma.
The most effective drug for syphilis is procaine benzyl-penicillin. Doxycycline or erythromycin can be used in patients who are sensitive to penicillin. Follow-up with regular clinical and serologic examinations is necessary for at least 2 years, and contact tracing is recommended.
Tuberculosis
There is a well-known phrase that states, “The more things change, the more they stay the same”. This expression continues to apply to tuberculosis (TB), a widespread infectious disease scourge traced back to the earliest of centuries. As a result of a resurgence of TB cases in the United States during the 1980s, attention refocused on the factors associated with the observed reversal of a previous declining disease trend; transmission modes of Mycobacterium tuberculosis, occupational infection risks associated with health care, and airborne-hazard infection control precautions. Despite dramatic improvements in public health measures associated with M. tuberculosis infection and disease, such as living conditions, nutrition, and antimicrobial chemotherapy, that resulted in an observed dramatic decline in the incidence of TB in the United States and certain other countries during the past century, TB remains a major public health concern for much of the world’s population.
Etiology and pathogenesis
The genus Mycobacterium contains a variety of species, ranging from human pathogens to relatively harmless organisms. As the major cause of TB, a chronic communicable disease, M. tuberculosis is by far the most historically prominent member of this group of bacteria. In addition to their very slow growth on special enriched media, these aerobic slender rods are characterized by their acid-fast staining feature. The unusually high lipid content of the cell wall confers the organisms with an ability to strongly retain a red dye (carbolfuchsin) after treatment with an acid-alcohol solution. This unique structure also allows the bacteria to survive outside a host’s body, suspended in airborne microdroplet nuclei for extended periods of time.
Contrary to a perception believed through the ages, M. tuberculosis is not a highly contagious bacterium. It does not synthesize potent exotoxins or extracellular enzymes, and it is not surrounded by an antiphagocytic capsule. Onset of infection appears to be related to the ability of tubercle bacilli to multiply within host cells and tissues while at the same time resisting host defenses. Infection with M. tuberculosis typically requires prolonged close contact of a susceptible host with an infectious source. The closeness of the contact with aerosolized bacilli and the degree of infectivity of the mycobacterial source are the most important considerations for infection. The overwhelming majority of primary human infections involve inhalation of mycobacteria-laden respiratory microdroplets. The diameter of these aerosolized droplets ranges from 1 to 5 microns. Dispersal of M. tuberculosis occurs via these droplets as a result of coughing, sneezing, or even speaking. Microdroplet nuclei are small enough to bypass protective host bronchial mucocilliary defenses, leading to mycobacteria subsequently replicating in both free alveolar spaces and within phagocytic cells. Repeated prolonged exposure to air that has been contaminated by droplets from a person with TB predisposes others to infection. This rationale is illustrated by the fact that people who live in the same home with an infected individual, or close friends or co-workers who routinely breathe the same mycobacteria-contaminated air from an undiagnosed or untreated person with pulmonary TB, have a high risk of acquiring infection. The organisms’ oxygen requirement predisposes the lungs as primary infection sites, with the potential for subsequent dissemination to other tissues. Cross-infection or spread of tubercle bacilli does not result from casual or sporadic exposure.
Onset of clinical disease is characterized by gradual infiltration of neutrophils, macrophages, and T lymphocytes. Distinctive granulomatous TB lesions called tubercles may appear anywhere in the lung parenchyma; however, they are most evident in the periphery. Because TB is the prototype microbial infection for inducing protective cellular immunity, the immunocompetence of the affected host plays a significant role in controlling the extent and severity of resultant disease. It is important to remember that most people infected with M. tuberculosis develop a positive type IV hypersensitive skin test reaction when challenged but do not progress to clinical disease. For those infected individuals who develop clinical symptoms, fatigue, malaise, weight loss, night sweats, and fever are most commonly noted in addition to positive chest radiograph manifestations. Pulmonary manifestations most frequently are chest pain, bloody sputum, and the presence of a prolonged productive cough of greater than 3 weeks’ duration.
Initial mycobacterial infection may progress to several different states depending on the extent of M. tuberculosis exposure and resistance of the patient. These include (1) asymptomatic primary tuberculosis, (2) symptomatic primary tuberculosis, (3) progressive primary tuberculosis, and (4) reactivation tuberculosis. A major risk factor for progression of initial infection with tubercle bacilli to more severe disease stages is the absence of an adequate host acquired cellular immune response to mycobacterial antigens. The ability of an infected individual to develop dual cellular and humoral immune responses against M. tuberculosis antigens thus greatly influences disease onset and progression.
Asymptomatic Primary Tuberculosis.
Individuals may be infected with M. tuberculosis without apparent clinical manifestations. When skin tested, individuals with asymptomatic primary tuberculosis display a positive tuberculin reaction indicating that they have been infected and have developed cell-mediated immunity against the bacteria. This protective immune response prevents the continued multiplication and dissemination of the bacteria, but it does not destroy all of the bacteria present. The remaining bacteria are sequestered within tubercles in the affected tissues and may be the source of bacteria that initiate reactivation tuberculosis.
Symptomatic Primary Tuberculosis.
In symptomatic primary tuberculosis, M. tuberculosis is spread via the lymphatics to cause granulomatous inflammation in both the lung periphery and hilar nodes, and it is accompanied by respiratory symptoms. The usual result is one of healing and development of cell-mediated immunity. The Ghon complex, a remnant of this infection, most often occurs in infants and children and is comprised of small calcified lung nodules and lymphadenopathy of the hilar lymph nodes.
Progressive Primary Tuberculosis.
A much more serious disease may develop in those individuals who are less resistant to tubercle bacilli. In these patients, microorganisms may spread throughout the body either (1) by means of the blood, resulting in miliary tuberculosis; (2) via the respiratory tissues, inducing a bronchopneumonia; or (3) through the gastrointestinal tract as a result of the organisms being coughed up. In miliary tuberculosis, foci of infection occur in distant organs and tissues but most frequently develop in the meninges, lungs, liver, and renal cortex. Although cell-mediated immunity may develop in some patients, others may not react (anergy) when skin tested with tuberculin protein preparations. Anergic patients have a poor prognosis for recovery and often die without rapid treatment.
Reactivation Tuberculosis
Reactivation tuberculosis occurs in individuals who have developed primary tuberculosis and who are asymptomatic, but who still carry the bacteria within tubercles. These patients exhibit positive tuberculin skin tests and thus demonstrate cellular immunity. Reactivation of disease is thought to be due to the activation of persistent bacteria in the tubercles of a previous infection, which become activated by some alteration in host resistance. Infection is characterized by tubercle formation, caseation, fibrosis, and further extension of the lesion. Progression may advance into a bronchus, leading to cavitation of the lung and secretion of an infectious sputum.
Oral manifestations
Oral manifestations of tuberculosis occur in approximately 3 % of cases involving long-standing pulmonary and/or systemic infection. The bacteria can infect oral tissues and lymph nodes (scrofula). Within the oral cavity, lesions can occur in the soft tissues and supporting bone and in tooth extraction sites, and may even affect the tongue and floor of the mouth.
When reviewing this information, it becomes apparent that progression of infection with tubercle bacilli to more severe disseminated stages occurs in the absence of adequate cellular immunity to infection. Thus, the ability of an infected individual to develop a dual immune response against M. tuberculosis antigens greatly influences disease onset and progression. These crucial protective responses are (1) acquired immunity to infection and (2) development of tuberculin hypersensitivity.
Diagnosis
A diagnosis of infection with M. tuberculosis relies on (1) development of a positive delayed hypersensitivity (tuberculin) skin reaction to purified protein derivative (PPD), a mycobacterial antigen isolated from bacterial cultures, and (2) demonstration of acid-fast mycobacteria in clinical specimens. Information obtained while collecting a patient’s medical history can provide evidence for suspicion of TB.
Treatment
Prior to the advent of antimicrobial chemotherapy, approximately 50 % of persons with active TB died within 2 years after onset of symptoms. Regimens of multiple antibiotics are currently used to treat patients with active TB to ensure tissue penetration and minimize emergence of resistant organisms. General guidelines for appropriate TB chemotherapy include necessity for long-term treatment interval (up to 2 years), initiation of treatment if sputum smear is positive for acid-fast bacilli, and patient compliance (a major factor in determining chemotherapy success).
Isoniazid (INH) is the antimycobacterial therapy cornerstone and is included in all routine drug regimens. People who develop a positive tuberculin skin reaction but do not have active disease, as well as close contacts of patients who develop TB, are placed on INH for 6 months to 1 year.
For treatment of patients with active TB, combinations of three or more drugs are chosen based on the nature and site of disease. In addition to INH, rifampin, pyrazinamide, and ethambutol are the most frequently applied drug combinations unless a specific instance of mycobacterial resistance is noted. Hepatotoxicity is a frequent adverse effect noted with prolonged administration of antimycobacterial chemotherapy.
Unfortunately, a major complication preventing successful elimination of acid-fast organisms in TB patients is non – compliance to the prolonged drug regimens. Patients often notice a substantial decline in symptoms within a few weeks of therapy and prematurely discontinue their medications. Consequently, bacterial strains causing multidrug-resistant tuberculosis (MDR-TB) have emerged and spread throughout the world.
Chemotherapy for tuberculosis: Combination therapy: usually 3–4 drugs to prevent resistance, chosen from the following: isoniazid, rifampin, ethambutol, rifabutin, streptomycin, pyrazinamide; Prolonged therapy – 6 months mi nimum – indicated for slow growth rate of bacteria, increasing incidence of Mycobacterium tuberculosis drug resistance.
Precancerous diseases of oral mucosa and lips. Risk factors of development of oncologic diseases
The processes, which precede the development of tumor, are called pretumorous, and with respect to cancer – precancerous. Precancerous processes differ from cancer in terms of absence of one or several symptoms, which make it possible to place the diagnosis of cancer.
The development of cancer is contributed by:
- chronic injuries;
- chronic inflammatory processes, accompanied by erosions and ulcers;
- proliferating processes;
- benign tumors.
Depending on frequency transition of cancer from obligatory and facultative diseases precancerous diseases are distinguished.
Obligatory precancerous diseases without treatment for different time periods surely lead to the development of cancer.
Facultative precancerous diseases do not always lead to cancer.
Obligatory precancers include:
- Bowen’s disease;
- Verruciform precancer of the red border of lips;
- Manganotti’s abrasive precancerous cheilitis;
- Limited precancerous hyperkeratosis of the red border of lips.
Facultative precancers include:
- erosive and verrucosa leukoplakia;
- papillomatosis;
- erosive-ulcerous and hyperkeratosic forms of lichen ruber planus and lupus erythematosis;
- chronic cracks of lips;
- skin horn;
- keratoacanthoma;
- post radiography stomatitis.
Bowen’s disease
Bowen’s disease (morben Bowen). It is potentially most malignant among all precancerous illnesses and is plotted in the concept of cancer in situ. Most frequently the soft palate, uvula, the retromolar region, the tongue are involved.
Clinic
A stricken area is usually one, rarely – two; it is the limited stagnant-red spot with smooth or velvety surface, with small papillary growths. As a result of the atrophy of mucous membrane the center will begin to slightly fall in comparison with the surrounding tissues.
The papillae of the tongue disappear near the lesion, if the lesion is localized in the tongue.
Disease runs an indeterminate time. In certain cases invasive increase rapidly begins, in others – it remains in the stage of cancer “in situ” for years.
Diagnostics
Diagnosis is confirmed by the histopathological study, which reveals the picture of intra-epithelial cancer: the polymorphism of the cells of prickly layer, an increase in the number of mitoses, their irregularity, gigantic and polynuclear cells, acanthosis, sometimes hyper – and parakeratosis.
The treatment of Bowen’s disease consists in the complete removal of stricken areas in the limits of healthy tissues. If it is impossible, short-distance radiation therapy is used.
Verruciform precancer
Verruciform precancer (praecancer of verrucosus). It appears almost exclusively on the red border of the lower lip. It has the type of the half-globular node – with a diameter of 4–10 mm, which is raised on 4–5 mm. On the top the node is covered with the tightly sitting gray fish-scales.
Treatment consists in the complete surgical removal of lesion in the limits of healthy tissues.
Manganotti’s abrasive precancerous cheilitis
Manganotti’s abrasive precancerous cheilitis (cheilitis abrasiva praecancrosa Manganotti). It is encountered predominantly in men older than 50 years of age. At Manganotti’s cheilitis age-specific trophic changes in the tissues and especially in lower lip are of great importance. In connection with this, in some people in response to the action of different stimuli, the torpid destructive processes are observed. In the pathogenesis of disease metabolic disorders, gastrointestinal tract dysfunction, hypovitaminosis A should be considered.
Clinic
The presence of one, rarely two and more erosions of rounded, oval or irregular shapes near the middle of red border of lip are characteristic. The surface of erosion is smooth, clear red. In some patients it is covered with a thin layer of epithelium or the crusts are formed on it. Infiltration of tissues at the base, around the erosion, is not observed. Erosions exist for a long time, sometimes they epithelialize, and then they again appear at the same or another place.
Treatment
It is necessary, first of all, to eliminate local irritating factors, and also detect and treat associated diseases of other organs and systems. If with a cytological examination the symptoms of the malignancy of Manganotti’s cheilitis are not revealed, then general and local treatment are carried out before the radical surgical intervention. The use of vitamin A concentrate, nicotinic acid, Nerobol is effective. Locally application of vitamin A concentrate, methyluracil, corticosteroid ointments, solkoseril are prescribed. If conservative treatment within 1 month does not lead to the epithelization of erosion, the surgical removal of stricken area is used.
Circumscribed precancerous hyperkeratosis of the red border of the lips
Circumscribed precancerous hyperkeratosis of the red border of lips (hyperkeratosis praecancrosa circumscripta). Middle-aged men predominate among the patients. Process is localized on the red border of the lower lip, on the side from the centre.
Clinic
The centre of keratinization has a polygonal form, with the size of 5–2 mm. It does not rise above the epithelium, but sometimes it will begin to fall back. Its surface is covered with thin, tightly fastened fish-scales.
Treatment consists in the surgical removal of stricken area in the limits of healthy tissues.
Dermatic horn
Dermatic horn (cornu cutaneum) is limited hyperplasia of the epithelium with the sharply pronounced hyperkeratosis, which in a form and density resembles a horn. It appears on the red border of the lip, more often on the lower one, in people older than 60 years.
Clinic is sufficiently typical. Lesion is a clearly limited centre with the diameter up to 10 mm, from which dirty or brown-gray protrusion of a cone-shaped form with a height not more than 10 mm, rises. A dermatic horn can exist for years, but malignancy at any time can begin. The appearance of inflammation and packing around the base of the horn, strengthening of the intensity of keratinization are the symptoms of malignancy.
Treatment consists in the surgical removal of stricken area in the limits of healthy tissues.
Keratoacantoma
Keratoacantoma (ceratoacantoma) – a benign epidermal tumor, which is most frequently localized on the red border of the lower lip, rarely – on the tongue.
Clinic
Disease begins with the formation on the lip or the tongue of sulfur-red nodule with the crateriform deepening in the centre, filled with horny masses. Within a month the tumor reaches the maximum size (25 × 10 mm). Most frequently it disappears itself in 6–8 months, and an atrophic pigmented scar is formed on its place or it can be transformed into cancer.
The treatment of keratoacantoma is surgical – removal in the limits of healthy tissues.
Allergic lesions of oral mucosa
Chronic recurrent aphthous stomatitis (RAS)
RAS is a disorder characterized by recurring ulcers confined to the oral mucosa in patients with no other signs of disease. Many specialists and investigators in oral medicine no longer consider RAS to be a single disease but, rather, several pathologic states with similar clinical manifestations. Immunologic disorders, hematologic deficiencies, and allergic or psychological abnormalities have all been implicated in cases of RAS.
RAS affects approximately 20 % of the general population, but when specific ethnic or socioeconomic groups are studied, the incidence ranges from 5 to 50 %. RAS is classified according to clinical characteristics: minor ulcers, major ulcers (Sutton’s disease, periadenitis mucosa necrotica recurrens), and herpetiform ulcers. Minor ulcers, which comprise over 80 % of RAS cases, are less than 1 cm in diameter and heal without scars. Major ulcers, are over 1 cm in diameter and take longer to heal and often scar. Herpetiform ulcers are considered a distinct clinical entity that manifests as recurrent crops of dozens of small ulcers throughout the oral mucosa.
Clinical manifestations
The first episodes of RAS most frequently begin during the second decade of life and may be precipitated by minor trauma, menstruation, upper respiratory infections, or contact with certain foods. The lesions are confined to the oral mucosa and begin with prodromal burning any time from 2 to 48 hours before an ulcer appears. During this initial period, a localized area of erythema develops. Within hours, a small white papule forms, ulcerates, and gradually enlarges over the next 48 to 72 hours. The individual lesions are round, symmetric, and shallow (similar to viral ulcers), but no tissue tags are present from ruptured vesicles (this helps to distinguish RAS from disease with irregular ulcers such as EM, pemphigus, and pemphigoid). Multiple lesions are often present, but the number, size, and frequency of them vary considerably. The buccal and labial mucosae are most commonly involved. Lesions are less common on the heavily keratinized palate or gingiva. In mild RAS, the lesions reach a size of 0.3 to 1.0 cm and begin healing within a week. Healing without scarring is usually complete in 10 to 14 days.
Most patients with RAS have between two and six lesions at each episode and experience several episodes a year. The disease is an annoyance for the majority of patients with mild RAS, but it can be disabling for patients with severe frequent lesions, especially those classified as major aphthous ulcers. Patients with major ulcers develop deep lesions that are larger than 1 cm in diameter and may reach 5 cm. Large portions of the oral mucosa may be covered with large deep ulcers that can become confluent. The lesions are extremely painful and interfere with speech and eating. Many of these patients continually go from one clinician to another, looking for a “cure”. The lesions may last for months and sometimes be misdiagnosed as squamous cell carcinoma, chronic granulomatous disease, or pemphigoid. The lesions heal slowly and leave scars that may result in decreased mobility of the uvula and tongue and destruction of portions of the oral mucosa. The least common variant of RAS is the herpetiform type, which tends to occur in adults. The patient presents with small punctate ulcers scattered over large portions of the oral mucosa.
Diagnosis
RAS is the most common cause of recurring oral ulcers and is essentially diagnosed by exclusion of other diseases. A detailed history and examination by a knowledgeable clinician should distinguish RAS from primary acute lesions such as viral stomatitis or from chronic multiple lesions such as pemphigoid, as well as from other possible causes of recurring ulcers, such as connective tissue disease, drug reactions, and dermatologic disorders. The history should emphasize symptoms of blood dyscrasias, systemic complaints, and associated skin, eye, genital, or rectal lesions. Laboratory investigation should be used when ulcers worsen or begin past the age of 25 years. Biopsies are only indicated when it is necessary to exclude other diseases, particularly granulomatous diseases such as Crohn’s disease or sarcoidosis.
Patients with severe minor aphthae or major aphthous ulcers should have known associated factors investigated, including connective-tissue diseases and abnormal levels of serum iron, folate, vitamin B12, and ferritin. Patients with abnormalities in these values should be referred to an internist to rule out malabsorption syndromes and to initiate proper replacement therapy. The clinician may also choose to have food allergy or gluten sensitivity investigated in severe cases resistant to other forms of treatment. HIV-infected patients, particularly those with CD4 counts below 100/mm3, may develop major aphthous ulcers.
Treatment
Medication prescribed should relate to the severity of the disease. In mild cases with two or three small lesions, use of a protective emollient such as Orabase or Zilactin is all that is necessary. Pain relief of minor lesions can be obtained with use of a topical anesthetic agent or topical diclofenac, an NSAID frequently used topically after eye surgery.
In more severe cases, the use of a high-potency topical steroid preparation, such as fluocinonide, betamethasone or clobetasol, placed directly on the lesion shortens healing time and reduces the size of the ulcers. The effectiveness of the topical steroid is partially based upon good instruction and patient compliance regarding proper use. The gel can be carefully applied directly to the lesion after meals and at bedtime two to three times a day, or mixed with an adhesive such as Orabase prior to application. Larger lesions can be treated by placing a gauze sponge containing the topical steroid on the ulcer and leaving it in place for 15 to 30 minutes to allow for longer contact of the medication. Other topical preparations that have been shown to decrease the healing time of RAS lesions include amlexanox paste and topical tetracycline, which can be used either as a mouth rinse or applied on gauze sponges. Intralesional steroids can be used to treat large indolent major RAS lesions. It should be emphasized that no available topical therapy decreases the onset of new lesions. In patients with major aphthae or severe cases of multiple minor aphthae not responsive to topical therapy, use of systemic therapy should be considered. Drugs that have been reported to reduce the number of ulcers in selected cases of major aphthae include colchicine, pentoxifylline, dapsone, short bursts of systemic steroids, and thalidomide. Each of these drugs has the potential for side effects, and the clinician must weigh the potential benefits versus the risks. Thalidomide has been shown to reduce both the incidence and severity of major RAS in both HIV-positive and HIV-negative patients, but this drug must be used with extreme caution in women during childbearing years owing to the potential for severe life-threatening and deforming birth defects.
Erythema multiforme
Erythema multiforme (EM) is an acute inflammatory disease of the skin and mucous membranes that causes a variety of skin lesions – hence the name “multiforme”. The oral lesions, typically inflammation accompanied by rapidly rupturing vesicles and bullae, are often an important component of the clinical picture and are occasionally the only component. Erythema multiforme may occur once or recur, and it should be considered in the diagnosis of multiple acute oral ulcers whether or not there is a history of similar lesions. There is also a rare chronic form of EM. EM has several clinical presentations: a milder self-limiting form and severe life-threatening forms that may present as either Stevens –Johnson syndrome or toxic epidermal necrolysis (TEN).
Etiology
EM is an immune-mediated disease that may be initiated either by deposition of immune complexes in the superficial microvasculature of skin and mucosa, or cell-mediated immunity.
The most common triggers for episodes of EM are herpes simplex virus and drug reactions. The drugs most frequently associated with EM reactions are oxicam nonsteroidal antiinflammatory drugs (NSAIDs); sulfonamides; anticonvulsants such as carbamazepine, phenobarbital, and phenytoin; trimethoprim-sulfonamide combinations, allopurinol, and penicillin. A majority of the severe cases of Stevens – Johnson syndrome or TEN are caused by drug reactions.
Clinical manifestations
General Findings. EM is seen most frequently in children and young adults and is rare after age 50 years. It has an acute or even an explosive onset; generalized symptoms such as fever and malaise appear in severe cases. A patient may be asymptomatic and in less than 24 hours have extensive lesions of the skin and mucosa. EM simplex is a self-limiting form of the disease and is characterized by macules and papules 0.5 to 2 cm in diameter, appearing in a symmetric distribution.
The most common cutaneous areas involved are: hands, feet, and extensor surfaces of the elbows and knees. The face and neck are commonly involved, but only severe cases affect the trunk. Typical skin lesions of EM may be nonspecific macules, papules, and vesicles. More typical skin lesions contain petechiae in the center of the lesion. The pathognomonic lesion is the target or iris lesion, which consists of a central bulla or pale clearing area surrounded by edema and bands of erythema.
The more severe vesiculobullous forms of the disease, Stevens – Johnson syndrome and TEN, have a significant mortality rate. EM is classified as Stevens – Johnson syndrome when the generalized vesicles and bullae involve the skin, mouth, eyes, and genitals.
The most severe form of the disease is TEN, (tone epidermal neurolysis), which is usually secondary to a drug reaction and results in sloughing of skin and mucosa in large sheets. Morbidity, which occurs in 30 to 40 % of patients, results from secondary infection, fluid and electrolyte imbalance, or involvement of the lung, liver, or kidneys. Patients with this form of the disease are most successfully managed in burn centers, where necrotic skin is removed under general anesthesia and healing takes place under sheets of porcine xenografts.
Oral lesions commonly appear along with skin lesions in approximately 70 % of EM patients. In some cases, oral lesions are the predominant or single site of disease. When the oral lesions predominate and no target lesions are present on the skin, EM must be differentiated from other causes of acute multiple ulcers, especially primary herpes simplex infection. This distinction is important because corticosteroids may be the treatment of choice in EM, but they are specifically contraindicated in primary herpes simplex infections. When there are no skin lesions and the oral lesions are mild, diagnosis may be difficult and is usually made by exclusion of other diseases. Cytologic smears and virus isolation may be done to eliminate the possibility of primary herpes infection. Biopsy may be performed when acute pemphigus is suspected. The histologic picture of oral EM is not considered specific, but the finding of a perivascular lymphocytic infiltrate and epithelial edema and hyperplasia is considered suggestive of EM. The diagnosis is made on the basis of the total clinical picture, including the rapid onset of lesions. The oral lesions start as bullae on an erythematous base, but intact bullae are rarely seen by the clinician because they break rapidly into irregular ulcers. Viral lesions are small, round, symmetric, and shallow, but EM lesions are larger, irregular, deeper, and often bleed. Lesions may occur anywhere on the oral mucosa with EM, but involvement of the lips is especially prominent, and gingival involvement is rare. This is an important criterion for distinguishing EM from primary herpes simplex infection, in which generalized gingival involvement is characteristic.
In full-blown clinical cases, the lips are extensively eroded, and large portions of the oral mucosa are denuded of epithelium. The patient cannot eat or even swallow and drools blood-tinged saliva. Within 2 or 3 days the labial lesions begin to crust. Healing occurs within 2 weeks in a majority of cases, but, in some severe cases, extensive disease may continue for several weeks.
Treatment
Mild cases of oral EM may be treated with supportive measures only, including topical anesthetic mouthwashes and a soft or liquid diet. Moderate to severe oral EM may be treated with a short course of systemic corticosteroids in patients without significant contraindications to their use. Systemic corticosteroids should only be used by clinicians familiar with the side effects, and, in each case, potential benefits should be carefully weighed against potential risks. Young children treated with systemic steroids for EM appear to have a higher rate of complications than do adults, particularly gastrointestinal bleeding and secondary infections. Adults treated with short-term systemic steroids have a low rate of complications and a shorter course of EM. The protein-wasting and adrenal-suppressive effects of systemic steroids are not significant when used short-term, and the clinical course of the disease may be shortened. An initial dose of 30 mg/d to 50 mg/d of prednisone or methylprednisolone for several days, which is then tapered, is helpful in shortening the healing time of EM, particularly when therapy is started early in the course of the disease. It should be noted that the efficacy of this treatment has not been proven by controlled clinical trials and is controversial.
Patients with severe cases of recurrent EM have been treated with dapsone, azathioprine, levamisole, or thalidomide. EM triggered by progesterone, also referred to as autoimmune progesterone dermatitis and stomatitis, has been oophorectomy has been necessary to cure the disorder. Antiherpes drugs such as acyclovir or valacyclovir can be effective in preventing susceptible patients from developing herpes-associated EM, if the drug is administered at the onset of the recurrent HSV lesion. Prophylactic use of antiherpes drugs is effective in preventing frequent recurrent episodes of HSV-associated EM. Systemic steroids are recommended for management of Stevens-Johnson syndrome and are considered life saving in severe cases.
Pemphigus vulgaris
PV is the most common form of pemphigus, accounting for over 80 % of cases. The underlying mechanism responsible for causing the intraepithelial lesion of PV is the binding of IgG autoantibodies to desmoglein 3, a transmembrane glycoprotein adhesion molecule present on desmosomes.
Typical lesions of recurrent intraoral herpes simplex virus infection in patients with normal immunity are clusters of small vesicles and ulcers on the heavily keratinized oral mucosa. Ulcerative, Vesicular, and Bullous Lesions gus foliaceus, but these antibodies are also detected in patients with long-standing PV. Evidence for the relationship of the IgG autoantibodies to PV lesion formation includes studies demonstrating the formation of blisters on the skin of mice after passive transfer of IgG from patients with PV. The mechanism by which antidesmoglein antibodies cause the loss of cell-to-cell adhesion is controversial. Some investigators believe that binding of the PV antibody activates proteases, whereas more recent evidence supports the theory that the PV antibodies directly block the adhesion function of the desmogleins.
The separation of cells, called acantholysis, takes place in the lower layers of the stratum spinosum. Electron microscopic observations show the earliest epithelial changes as a loss of intercellular cement substance; this is followed by a widening of intercellular spaces, destruction of desmosomes, and finally cellular degeneration. This progressive acantholysis results in the classic suprabasilar bulla, which involves increasingly greater areas of epithelium, resulting in loss of large areas of skin and mucosa.
Pemphigus has been reported coexisting with other autoimmune diseases, particularly myasthenia gravis. Patients with thymoma also have a higher incidence of pemphigus. Several cases of pemphigus have been reported in patients with multiple autoimmune disorders or those with neoplasms such as lymphoma. Death occurs most frequently in elderly patients and in patients requiring high doses of corticosteroids who develop infections and bacterial septicemia, most notably from Staphylococcus aureus.
Clinical Manifestations
The classical lesion of pemphigus is a thin-walled bulla arising on otherwise normal skin or mucosa. The bulla rapidly breaks but continues to extend peripherally, eventually leaving large areas denuded of skin. A characteristic sign of the disease may be obtained by application of pressure to an intact bulla. In patients with PV, the bulla enlarges by extension to an apparently normal surface. Another characteristic sign of the disease is that pressure to an apparently normal area results in the formation of a new lesion. This phenomenon, called the Nikolsky sign, results from the upper layer of the skin pulling away from the basal layer. The Nikolsky sign is most frequently associated with pemphigus but may also occur in epidermolysis bullosa.
Some patients with pemphigus develop acute fulminating disease, but, in most cases, the disease develops more slowly, usually taking months to develop to its fullest extent.
Oral Manifestations
Eighty to ninety percent of patients with pemphigus vulgaris develop oral lesions sometime during the course of the disease, and, in 60 % of cases, the oral lesions are the first sign. The oral lesions may begin as the classic bulla on a noninflamed base; more frequently, the clinician sees shallow irregular ulcers because the bullae rapidly break. A thin layer of epithelium peels away in an irregular pattern, leaving a denuded base. The edges of the lesion continue to extend peripherally over a period of weeks until they involve large portions of the oral mucosa. Most commonly the lesions start on the buccal mucosa, often in areas of trauma along the occlusal plane. The palate and gingiva are other common sites of involvement.
It is common for the oral lesions to be present up to 4 months before the skin lesions appear. If treatment is instituted during this time, the disease is easier to control, and the chance for an early remission of the disorder is enhanced. Frequently, however, the initial diagnosis is missed, and the lesions are misdiagnosed as herpes infection or candidiasis. Zegarelli and Zegarelli studied 26 cases of intraoral PV. The average time from onset of the disease to diagnosis was 6–8 months. They also noted that several patients had coexisting candidiasis, which sometimes masked the typical clinical picture of the pemphigus lesions. There is also a subgroup of pemphigus patients whose disease remains confined to the oral mucosa. These patients often have negative results on direct immunofluorescence (DIF). If a proper history is taken, the clinician should be able to distinguish the lesions of pemphigus from those caused by acute viral infections or erythema multiforme because of the acute nature of the latter diseases. It is also important for the clinician to distinguish pemphigus lesions from those in the RAS category. RAS lesions may be severe, but individual lesions heal and recur. In pemphigus, the same lesions continue to extend peripherally over a period of weeks to months. Lesions of pemphigus are not round and symmetric like RAS lesions but are shallow and irregular and often have detached epithelium at the periphery. In early stages of the disease, the sliding away of the oral epithelium resembles skin peeling after a severe sunburn. In some cases, the lesions may start on the gingiva and be called desquamative gingivitis. It should be remembered that desquamative gingivitis is not a diagnosis in itself; these lesions must be biopsied to rule out the possibility of PV as well as bullous pemphigoid,mucous membrane pemphigoid, and erosive lichen planus.
Laboratory Tests
PV is diagnosed by biopsy. Biopsies are best done on intact vesicles and bullae less than 24 hours old; however, because these lesions are rare on the oral mucosa, the biopsy specimen should be taken from the advancing edge of the lesion, where areas of characteristic suprabasilar acantholysis may be observed by the pathologist. Specimens taken from the center of a denuded area are nonspecific histologically as well as clinically. Sometimes several biopsies are necessary before the correct diagnosis can be made. If the patient shows a positive Nikolsky sign, pressure can be placed on the mucosa to produce a new lesion; biopsy may be done on this fresh lesion.
A second biopsy, to be studied by DIF, should be performed whenever pemphigus is included in the differential diagnosis.
Treatment
An important aspect of patient management is early diagnosis, when lower doses of medication can be used for shorter periods of time to control the disease. The mainstay of treatment remains high doses of systemic corticosteroids, usually given in dosages of 1 to 2 mg/kg/d. When steroids must be used for long periods of time, adjuvants such as azathioprine or cyclophosphamide are added to the regimen to reduce the complications of long-term corticosteroid therapy. Prednisone is used initially to bring the disease under control, and, once this is achieved, the dose of prednisone is decreased to the lowest possible maintenance levels. Patients with only oral involvement also may need lower doses of prednisone for shorter periods of time, so the clinician should weigh the potential benefits of adding adjuvant therapy against the risks of additional complications such as blood dyscrasias, hepatitis, and an increased risk of malignancy later in life. There is no one accepted treatment for pemphigus confined to the mouth, but one 5-year follow-up study of the treatment of oral pemphigus showed no additional benefit of adding cyclophosphamide or cyclosporine to prednisone versus prednisone alone, and it showed a higher rate of complications in the group taking the immunosuppressive drug.
Most studies of pemphigus of the skin show a decreased mortality rate when adjuvant therapy is given along with prednisone. One new immunosuppressive drug, mycophenolate, has been effective when managing patients resistant to other adjuvants. The need for systemic steroids may be lowered further in cases of oral pemphigus by combining topical with systemic steroid therapy, either by allowing the prednisone tablets to dissolve slowly in the mouth before swallowing or by using potent topical steroid creams. Other therapies that have been reported as beneficial are parenteral gold therapy, dapsone, tetracycline, and plasmapheresis.
Plasmapheresis is particularly useful in patients refractory to corticosteroids. A therapy described by Rook and colleagues involves administration of 8-methoxypsoralen followed by exposure of peripheral blood to ultraviolet radiation.
Pemphigus vegetans
Pemphigus vegetans, which accounts for 1 to 2 % of pemphigus cases, is a relatively benign variant of pemphigus vulgaris because the patient demonstrates the ability to heal the denuded areas. Two forms of pemphigus vegetans are recognized: the Neumann type and the Hallopeau type. The Neumann type is more common, and the early lesions are similar to those seen in pemphigus vulgaris, with large bullae and denuded areas. These areas attempt healing by developing vegetations of hyperplastic granulation tissue. In the Hallopeau type, which is less aggressive, pustules, not bullae, are the initial lesions. These pustules are followed by verrucous hyperkeratotic vegetations.
Biopsy results of the early lesions of pemphigus vegetans show suprabasilar acantholysis. In older lesions, hyperkeratosis and pseudoepitheliomatous hyperplasia become prominent. Immunofluorescent study shows changes identical to those seen in PV.
Oral Manifestations
Oral lesions are common in both forms of pemphigus vegetans and may be the initial sign of disease. Gingival lesions may be lace-like ulcers with a purulent surface on a red base or have a granular or cobblestone appearance. Oral lesions that are associated with inflammatory bowel disease and resemble pemphigus vegetans both clinically and histologically are referred to by some authors as pyostomatitis vegetans.
Treatment
Treatment is the same as that for PV.
Lichen ruber planus
Lichen ruber planus (Lichen ruber planus) is the chronic disease, which is manifested on the skin and the mucous membranes by formation of the keratinized papules.
LRP oral mucosa is usually encountered in people of middle age, predominantly in women. Very rarely this illness can be found at younger age, and also in children.
Elements of lesion
Separate papules which appear on the skin are more often miliary. Their base is slightly infiltrated, round, oval, and sometimes elongated. Here at first the papules have lusterless colour, then they turn pink, reddish and even lilac-violet; sometimes long-existing papule turn brown. Since the papules are cornification, they slightly rise above the surrounding skin.
The favourite places of the precipitations of papules LRP on the skin are flexible surfaces. On the hands – this is the region of radiocarpal joint. The development of disease is possible on mucosa membrane in different parts of gastrointestinal tract.
LRP of oral mucosa has predominantly two localizations:
- The most typical is the distal part of the cheek or the pear-shaped region, where the polygonal papules, after merging between themselves, form a figure in the form of fern leaves or grid; they are clearly defined and can be palpated.
- The tongue (dorsal and lateral surface), in which the signs of disease are represented very diversely: the polygonal knots, which form an area either covered with scar-like strips as grids, the atrophic sections of oral mucosa, or hypertrophic papules.
Treatment
The complex therapy LRP includes two groups of the measures:
- General action.
- Action directed to the LRP centre.
The general directions of the therapy of all LRP forms are: the liquidation of keratosis and inflammation, and the normalization of the process of callusing the epithelium, and also the elimination of intra- and para focal complications (erythema, erosions, bubbles, welding dribbles, ulcers).
Local treatment consists in the elimination of the irritating factors.
Changes in the oral mucosa at diseases of internal organs and systems
Changes in the oral mucosa at diseases of gastrointestinal tract
Changes in the tongue. They are the most typical at diseases of gastrointestinal tract. Among these signs the furred tongue is most frequently revealed. The disturbance of the process of cornification and destruction of epithelial cells in the tongue papillae, as a result of the neurotrophic disorders, play an important role in the formation of fur on the tongue. The nature of food, the composition of microflora, the oral hygiene influence the accumulation of fur. If the epithelium detachment is not observed, the keratinized cells remain, dead leukocytes and microorganisms of saliva are joined and form fur. In this case the favorable conditions for multiplication of microorganisms are created, in particular, a significant amount of fungi is formed. All of this is the basis of fur. Fur is revealed with gastritis, stomach ulcer and duodenal ulcer, new formations in the stomach and other illnesses.
Edema of the tongue is the second sign of gastrointestinal diseases. It does not cause subjective sensations in patient. Edema of the tongue is observed in case of chronic bowel diseases, which is explained by the disturbance of the sucking ability in the gut and gut barrier function. The changes in the different groups of the papillae of the tongue are observed at diseases of gastrointestinal tract. Depending on their state hyper- and hypoplastic glossitis are distinguished.
Hyperplastic glossitis is observed in patients in case of gastritis with increased acidity. It is accompanied by the hypertrophy of papillae, presence of fur, a slight increase in size of the tongue as a result of edema.
Hypoplastic glossitis is characterized by the atrophy of papillae, sometimes sharply expressed, in consequence of which it become varnished, with bright spots and strips. The atrophy of the tongue papillae causes the sensation of burning, tingling, pain when eating. Such changes in the tongue papillae are observed in case of gastritis with lowered secretion, ulcer, gastroenteritis, biliary tract disease.
The intensive exfoliation of the epithelium of the tongue is fairly often observed at diseases of gastrointestinal tract.
Changes of oral mucosa. The most frequent manifestation of the disease of gastrointestinal tract is a change in colour of oral mucosa. The catarrhal stomatitis is observed at hyperacidic and normacidic gastritis, ulcer, enterocolitis. Characteristic pigmentation of oral mucosa occurs in case of liver disease: entire mucosa turns pink, and the soft palate turns yellowish.
The treatment of changes of oral mucosa in case of digestive system diseases is symptomatic. At the same time, it provides for the normalization of the function of these organs, hyposensitizing therapy, vitamin therapy (groups B, C, A, PP), and oral cavitysanitation.
Lesions of the oral mucosa at cardiovascular pathology
Changes of oral mucosa at cardiovascular diseases depend on the degree of insufficiency of blood circulation, state of vascular wall, etc.
Cyanosis of oral mucosa, lips and the tongue of bright red or crimson color are characteristic for the acute period of myocardial infarction.
The appearance of trophic changes of oral mucosa, up to the formation of ulcers, is observed predominantly in patients with the decompensated defects of heart and the disturbance of blood circulation of III, sometimes II degree. Trophic ulcers are localized predominantly in the rear of the mouth, on the cheek mucosa, alveolar branch, on the tongue, on the mucous a pear-shaped area, etc.
Ulcers have different sizes (2–5 mm and more). They are covered with pale gray fur with the fetid smell; it is sharply painful when touching and eating. The inflammatory reaction in the surrounding tissues is absent.
The treatment of such changes of oral mucosa provides for the liquidation of the insufficiency of blood circulation in combination with the local symptomatic therapy.
Changes in the oral mucosa at endocrine diseases
Diabetes mellitus
The most characteristic changes in the oral cavity are xerostomia, catarrhal stomatitis and glossitis, fungal stomatitis, mycotic perleche, paresthesias of oral mucosa, trophic disorders, Lichen ruber planus.
Dentist conducts the treatment of a patient together with the endocrinologist. The symptomatic treatment is prescribed with the expressed changes in the oral cavity taking into account their manifestation.
Myxedema is developed with the insufficiency of the function of the thyroid gland. The face of patient takes the unique form: lips and nose are thickened, upper eyelids are sharply edematic, and facial expression is indifferent. In patients anemia, edema and dryness of oral mucosa are observed. Myxedema is accompanied by a marked increase of the tongue, which is sometimes not placed in the oral cavity, an increase of the lips, gums.
Dentist conducts the sanitation of the oral cavity and symptomatic treatment if necessary.
Pregnancy gingivitis is an inflammation of gums, which first appears during pregnancy or is exacerbated by pregnancy. The development of the disease is connected with restoring of hormonal balance during this period. In the first half of pregnancy the catarrhal gingivitis is noted. In the second half – the course of disease is heavy, with the development of proliferating process in the gums. In the initial stage of gingivitis the gingival edge becomes clear red, swells, bleeds easily. Gradually the affected gum becomes dark red, cyanotic, increases and with the presence of local stimuli the hypertrophic gingivitis develops. Hypertrophic gingivitis in pregnancy tends to polypous growth of separate papillae. Sometimes false epulis develop. The hypertrophied gum covers the entire dental crown, bleeds easily.
Treatment. The local treatment of pregnancy gingivitis is conducted through the principles of the treatment of catarrhal or hypertrophic gingivitis.
Itsenko-Cushing disease. The oral mucosa in such patients is edematic, the imprints of teeth on the tongue and the cheeks are observed. Appearing trophic disorders lead to the appearance of erosions and ulcers which are characterized by a prolonged course. Candidiasis is frequently observed.
Treatment is carried out together with the endocrinologist. The sanitation of the oral cavity and symptomatic therapy depending on clinical manifestations is indicated.
Addison’s disease is caused by curtailment in production of hormones of the adrenal cortex. The most characteristic feature of the disease is the specific pigmentation of the skin and oral mucosa. The changes in the mucous membrane of the oral cavity in case of diseases of internal organs and systems are: small spots or bluish, grayish black strips. Patients do not subjectively feel it. Changes in the mouth and on the skin appear as a result of the deposit of the large number of melanin.
Manifestations on oral mucosa with the diseases of the blood and hematopoietic organs
Iron-deficiency (hypochromic) anemia (chlorosis). Patients with early chlorosis complain about the disturbance of gustatory senses, sense of smell, reduction in appetite, nausea. The oral mucosa is without the noticeable disturbances, except for color change – it becomes pale. All symptoms are more expressed with late chlorosis. Patients complain about painful sensations in the tongue and oral mucosa when eating sour or spicy food, dryness in the oral cavity, paresthesia (burning, tingling, prickling and bursting the tongue open), and the presence of angular heilitis.
The clinical picture of hypochromic anemia is multiple lesions of carious teeth, their increased abrasion, and loss of the natural luster of enamel. Mucosa membrane of lips, cheeks and gums is pale, edematic. The tongue is edematic, papillae are atrophied, especially in its front part. It becomes clear red and smooth, as if polished, deep folds appear. Sometimes hemorrhages and cracks in the angles of the mouth are observed.
Treatment
The symptomatic therapy of manifestations on mucous membrane is prescribed.
Hypoplastic anemia appears under the action of the exogenous physical (irradiation) and chemical factors, and drugs as well as endogenous aplasia of bone marrow. On the background of particularly pale oral mucosa different heavy hemorrhages appear. Interdental papillae are edematic, cyanotic, sometimes bleeding, deep parodontal pockets are revealed. On oral mucosa, besides petechiae, also erosions, ulcers, necrotic sections are observed.
Treatment
Dentist conducts the symptomatic treatment of the manifestations of hypoplastic anemia.
B12 – folate deficient anemia (malignant anemia, pernicious anemia, Addison – Birmera disease) is characterized by the disturbance of erythropoiesis. The clinical picture of disease consists of the triad: the dysfunction of the gastrointestinal tract, hemopoietic and nervous systems. One of the early symptoms of the disease is the pallor of the skin and oral mucosa with a yellowish tint. Sometimes on oral mucosa petechial hemorrhages are observed. The most characteristic lesion of oral mucosa in case of malignant anemia is hunter’s glossitis. The back of the tongue in this case takes the form of the smooth, bright, polished surface as a result of the atrophy of mushroom-shaped filamentary papillae, thinning of epithelium and atrophy of muscles. Painful, sharply limited strips and spots of clear red color of inflammatory nature appear at the back and the tip of the tongue.
Treatment is carried out in the hematology clinics. Locally symptomatic treatments, sanitation of oral cavity are carried out.
Leucosis is the malignant disease of the hemopoietic organs, which appears as a result of progressive cellular hyperplasia in the hemopoietic organs, when the processes of cellular division (proliferation) prevail above the processes of ripening (differentiation). Pathomorphological substratum of disease is leukemia blast cells, which correspond to primordial elements of one of the hematopoietic lineage.
The clinical picture of acute leucosis determines 4 leading syndromes: hemorrhagic, hyperplastic, anaemic and intoxicating. Hemorrhagic syndrome is manifested in the form of petechiae, ecchymosis, hematomas on the skin and mucous membrane, or the profuse bleedings.
In the oral cavity the most characteristic are: acute bleeding of gums, presence of hemorrhages on mucous membrane of cheeks along the line of the joining of teeth, in the tongue, the palate. Severe hemorrhages and hematomas sometimes are revealed. Hyperplastic processes are manifested in the increase of the lymph nodes, liver, spleen, tonsils. Frequently hyperplasia is combined with ulceronecrotic changes in the gums. Furthermore, necroses are revealed also in the tonsils, the pear-shaped area and other parts of oral mucosa. Its tendency toward the propagation in the adjacent sections is the special feature of necrotic process in case of sharp leucosis, in consequence of which the unlimited ulcers of irregular outlines, covered with gray necrotic fur appear. Reactive changes around the ulcer are absent or are weakly expressed. The development of ulceronecrotic processes in the oral cavity is connected with sharp reduction in the resistibility of tissues caused by reduction in the phagocytic activity of leukocytes and immune properties of blood serum.
Patients with acute leucosis complain about pain in the intact teeth and the jaws (together with pain in other bones), which is explained by the direct lesion of the bones in case of the leukemic process.
Treatment is conducted in the hematology hospitals. The treatment of leukosis stomatitis is symptomatic. The extraction of teeth is contraindicated.
The chronic leucosis appear more rarely than acute, development is more favorable; course is prolonged.
Chronic myeloleukemia passes two stages: benign (lasts several years) and malignant (terminal), which lasts for 3 -6 months. The basic sign of chronic myeloleukemia in the oral cavity are hemorrhagic manifestations, but with considerably smaller intensity, than in case of acute leucosis. Bleeding of gums appears not spontaneously, but only with the traumatization, the removal of teeth. In the period of excerbation the ulceronecrotic lesions of oral mucosa are observed.
Chronic lymphoid leukosis is characterized by slow beginning and prolonged latent course.
In the initial stage of disease an increase in groups of lymph nodes is observed. At the developed stage the generalized increase of lymph nodes is observed, the pallor of the skin and the mucous membranes, leukemic infiltrations of gums, the tongue, and hyperplasia of interdental papillae appear. Sometimes the growth of gingival edge reaches the level of the joining of teeth.
Treatment is conducted in the hematology departments. Local treatment consists in care of the oral cavity, full-fledged sanitation, symptomatic therapy.
Agranulocytosis is a syndrome, which is characterized by the significant decrease in the number or absence of neutrophilic granulocytes in the peripheral blood. Ulceronecrotic process in the lips, the gums, the tongue, mucous membrane of cheeks and other sections develop. Ulceronecrotic process can spread into the gullet. The absence of the inflammatory reaction of tissues around the centre of necrosis is important for diagnostics. Frequently necrotic process is combined with candidiasis.
Treatment is conducted in the hematology departments. Local treatment is symptomatic; it includes the antiseptic treatment of oral cavity, anesthetization, removal of necrotic tissues, and prescription of the preparations, which stimulate regeneration.
Erythremiya (polycythemia, the Vaquez’ disease)
Erythremiya appears at the age of 40–60 years, predominantly in men.
Disease begins unnoticeably, and develops slowly. Increased fatigue, bleeding of gums, hemorrhages from the nose are noted. Characteristic symptom for patients is dark-cherry polycythemia of oral mucosa. Lips, the tongue, buccal mucosa are clear red because of the increased content of reduced hemoglobin in the capillaries. Mucous membrane in the region of alveolar branches is friable, with the cyanotic tint; when pressing bleeds easily, interdental papillae are hyperemized, and of dark-cherry colour. Expressive color boundary – cyanosis of soft palate and pale color of hard palate (Cooperman’s symptom) is characteristic. The itching of the skin and paresthesia of oral mucosa due to the increased filling of vessels and the irritation of the interoceptors of capillaries by the blood is possible.
Treatment is conducted by hematologist, making periodic bloodlettings and using the cytostatic therapy with radioactive phosphorus or mielosan.
Thrombocytopenic purpura (Verlgof disease)
The basic clinical symptom of disease is hemorrhages from the skin and oral mucosa, as well as nose and gums, that appear spontaneously or under the effect of the insignificant injury. In general in case of thrombocytopenic purpura the oral mucosa is pale, edematic, atrophied; the thinning of epithelium, erosions or ulcers form.
Treatment is conducted in the hematology departments.
Changes in the oral mucosa at hypo- and avitaminoses
Hypovitaminosis C
The insufficiency of vitamin C is always manifested by changes in the oral cavity. Scorbutic stomatitis is one of the earliest and frequent symptoms of the disease.
Three stages of scorbutic stomatitis are distinguished:
- scorbutic stomatopatia – the initial stage;
- scorbutic reparative stomatitis – the developed stage;
- scorbutic ulcerous stomatitis – the complicated stage.
Initial stage is characterized by expressed gingivitis on the background of pale anemic oral mucosa: gum becomes infiltrated, gingival edge acquires dark red color, and bleeds easily. Sometimes single, scattered petechia in gum and oral mucosa is observed. Simultaneously petechiae can be revealed on the extremities, in the shin region. Patients complain about general weakness, sleepiness, rheumatic pain in extremities, headache, and rapid fatigue. Initial stage is frequently accompanied by iron-deficiency anemia.
The developed stage of the disease is characterized by the significant inflammation of gums. Gum is sharply edematic, enlarged, and friable; it covers a significant part of the dental crowns. Gingival edge acquires cyanotic tint, it bleeds considerably when pressing. On the edge of gingival papillae the blood clots are frequently accumulated. On oral mucosa the plural petechiae, ecchimozis are observed. The tongue is furred, swells sharply, and the teeth imprints on its edges are observed. Teeth are loosening.
Petechiae, ecchymozis and massive hemorrhages are observed on the mucous membrane of cheeks, palate and in different parts of body. The general state of patients deteriorates, they become adynamic, the face is pale with the earthen tint.
The third, complicated stage of the disease appears with the connection of secondary fusospirillary infection, in consequence of which scorbutic ulcerous stomatitis develops. The granulations grown on the gingival edge reach the cutting edge or the occlusal surface of teeth; areas of necrosis and pitting appear on the gums. Gums bleed intensively; they are covered with necrotic fur, with the fetid smell. Ulcerous process extends to tongue, cheeks, lips, hard and soft palate. Teeth are loosening and fall out. The general state of patients is extremely heavy. Without the treatment the disease can end lethally.
Treatment
At the initial stage of the disease with correct treatment under the dispensary conditions scorbutic gingivitis disappears in 5-7 days. At the developed and complicated stages of the disease patients subject to hospitalization.
Local treatment: the sanitation of oral cavity is indicated, careful oral hygiene, removal of dental calculus and plaque, irrigation of the oral cavity by the dilute solution of potassium permanganate, the solution of citral, 1 % solution of galaskorbin.
Hypovitaminosis A
Vitamin A (retinol) is of great importance in the processes of growth and development of organism; it regulates the processes of ripening and keratinization of the epithelium, increases resistance of oral mucosa to the action on it of different traumatic and irritating factors, ensures the normal functioning of the organ of vision, favors the normal functioning of salivary and sweat glands. The clinical manifestations of hypovitaminosis are caused by reduction in the barrier properties of the skin and oral mucosa, the disruption of the normal differentiation of epithelial tissues. At hypovitaminosis A oral mucosa is pale, turbid, dry, loses its characteristic luster. On mucous membrane of cheeks, the hard and soft palate the whitish stratifications, which resemble the mild form of leukoplakia appear. Keratinization of epithelium of the excretory ducts of salivary glands occurs. This leads to a decrease in secretion of saliva – hyposalivation.
Treatment – products rich in vitamin A (butter, milk, egg yolk, sour cream, liver), or carotene, which is converted in the organism into the vitamin A (carrot, apricots, peaches, black currant). Fish oil (3 tablespoons per day for adult person, 3 teaspoons – for the child) is prescribed.
Hypovitaminosis PP
In the oral cavity the clinical manifestations of hypovitaminosis PP flow in several stages: the first stage is connected with the appearance of erythema; it is observed already in the prodromal period. Patients complain about the sensation of burning in the area of mucosa of lips, cheeks and especially the tongue. Oral mucosa becomes hyperemized, the tongue is swollen, and filamentary papillae are atrophied. The general state: weakness, headache, insomnia, loss of appetite appear. The pain in the mouth, like neuralgic, appears in stage II. Inflammatory process extends to entire oral mucosa. The tongue becomes clear red and edematic, with a raspberry-coloured tint, resembling the colour of cardinal’s mantle – “cardinal” tongue; the surface layers of the epithelium desquamate, thus the tongue becomes bright, smooth, specular. Sometimes cracks appear on it – “chess tongue”. At this stage the general state of the patient worsens, diarrhea, dermatitis, depression, dystrophia appear. At the stage III the general state of patient is severe. In the oral cavity with the appearance of fuzospirill symbiosis the ulcerous stomatitis develops.
Treatment is specific: saturation of the organism by nicotinic acid (daily dose of 150 mg), and at the 3rd stage dose increases to 300 mg, vitamins of group B: thiamine (20–50 mg), riboflavin (10–20 mg), pyridoxine (50 mg) are prescribed.
Hypovitaminosis B1
A deficiency of vitamin B1 (thiamine) causes the disease, known as beri-beri. Changes in the oral cavity are not always sufficiently characteristic. The lack of thiamine is sometimes accompanied by the neuralgia of trigeminal nerve, increased by painful sensitivity of oral mucosa. Some patients complain about the pain. Frequently bubble lesions of oral mucosa develop, it is more similar to herpetic stomatitis. Phials are localized on the hard palate and on the tongue.
Treatment is specific: saturation of organism by thiamine. Local treatment is symptomatic.
Hypovitaminosis B2
In the absence or deficiency of riboflavin (vitamin B2) in the food ariboflavinosis develops. The disease is characterized by the inflammation of the lips (angular cheilitis), glossitis, and conjunctivitis.
Angular cheilitis begins with the reddening in the angles of the mouth, and then the painful cracks appear, which resemble perleche. Lips become red, swollen, cracks and erosions appear on their surface. Simultaneously glossitis develops, which is accompanied by sharp painfulness. Filamentary papillae atrophy, thus clear red hypertrophied mushroom-shaped papillae appear across the back of the tongue. As a result of the atrophy of filamentary papillae the tongue becomes smooth, shiny; because of the decreased salivation it seems dry, with many grooves, increased in size. Besides glossitis, conjunctivitis appears, sometimes iritis, eyelids are inflamed, epiphora, burning in the eyes, visual acuity decrement are observed.
Treatment consists in saturation of organism by vitamins of group B (B1, B2, B12). Local treatment is symptomatic.
Chapter 8. Anatomical and functional peculiarities of the maxillofacial area and neck
Face of the embryo appears to develop by the end of the 1st prenatal month of embryogenesis. This process takes place due to the fusion of 5 processes: 2 paired maxillary and mandible as well as odd one – frontal. All these comprise the 1stbranchial arch and define the oral cavity (see Fig. 8.1).

Fig. 8.1. Stages of maxillofacial genesis. Frontal view (Petten et all, 1959).
A – 4-week embryo (3.5 mm): 1 – frontal process, 2 – nasal placode, 3 – pharyngeal membrane, 4 – maxillary process, 5 – mandibular arch, 6 – hyoid arch.
B – 5-week embryo (6.5 mm): 1 – frontal process, 2 – nasal fossa, 3 – oral orifice, 4 – maxillary process, 5 – mandibular arch, 6 – hyoid arch.
C, D – 5½-week (9 mm) and 6-week (12 mm) embryo: 1 – medial nasal process, 2 – lateral nasal process, 3 – naso-lacrimal groove, 4 – maxillary process, 5 – mandibular, 6 – hyomandibular fissure.
E – 7-week (19 mm) embryo: 1 – lateral nasal process, 2 – medial nasal process, 3 – auditory humps around of hyomandibular fissure, 4 – hyoid bone, 5 – larynx cartilage.
F – 7,5-week (28 mm) embryo: 1 – lateral nasal process, 2 – medial nasal processes, 3 – external ear, 4 – hyoid bone, 5 – larynx cartilage
Neuroanatomy of the maxillofacial area
The maxillofacial area takes nerve supply from motor, sensory and vegetative (sympathetic and parasympathetic) nerves.
Cranial nerves give innervation:
I (olfactory) – sense of smell, V (trigeminal), VII (facial), IX (glossopharyngeal), X (vagus), XII (hypoglossal).
Sensory nerves: V (trigeminal), IX (glossopharyngeal), X (vagus), branches from cervical plexus (major auricular and minor occipital nerves).
Motor nuclei of the brainstem give nerve fibers to the jaw muscles (V trigeminal), to mimic muscles (VII facial), to the muscles of the palate and pharynx, (X vagus), to the muscles of the tongue (XII – hypoglossal).
The trigeminal nerve is a mixed nerve; it has four nuclei of which two sensory and one motor nucleus are in the mezencephalon, while the sensory (proprioceptive nucleus) is in the mesencephalon. The processes of cells contained in the motor nucleus (nucleus motorius) emerge from the pons on the line separating the pons from the middle cerebellar peduncle and connecting the place of emergence of the trigeminal and facial nerves (linea trigeminofacialis), forming the motor root of the nerve, radix motoria. Next to it, the sensory root, radix sensoria, enters the brain matter.
Both roots comprise the trunk of the trigeminal nerve which on emergence from the brain penetrates under the dura mater of the middle cranial fossa and is distributed onto the superior surface of the pyramid of the temporal bone at its apex where the trigeminal impression (impressiotrigemini) is located. Here the dura mater separates to form a small cavity for it, cavum trigeminale. In this cavity the sensory root has a large semilunar (or Gasser’s) ganglion, ganglion trigeminale (s. semilunare Gasseri). The central processes of the cells of this ganglion comprise the sensory root and run to the sensory nuclei: superior sensory nucleus (nucleus sensoriusprincipalis n. trigemini), spinal nucleus (nucleus tractusspinalis n. trigemini) and mesencephalic nucleus (nucleus tractusmesencephalicis n. trigemini), while the peripheral processes are part of the three main branches (divisions) of the trigeminal nerve emerging from the convex edge of the ganglion.
The maxillary nerve (n. maxillaris) is the second branch of the trigeminal Nerve, which is illustrated on Fig. 8.2. It emerges from the cranial cavity through the foramen rotundum into the pterygopalatine fossa; here it is directly continuous with the infraorbital nerve (n. infraorbitalis) which passes through the inferior orbital fissure into the orbital sulcus and canal on the inferior orbital wall and then emerges through the infraorbital foramen onto the face where it ramifies into a bundle of branches.

Fig. 8.2. Neuroanatomy of the maxillary nerve:
1 – gangliontrigeminale; 2 – n. maxillaris; 3 – foramen rotundum; 4 – n. infraorbitalis; 5 – rr. alveolares superiores posteriores; 6 – r. alveolaris superior medius; 7 – rr. alveolaressuperioresanteriores;
8 – n. zygomaticus; 9 – r. zygomaticotemporale; 10 – r. zygomaticofacial; 11 – rr. ganglionares ganglion pterygopalatinum
These branches join partly with the branches of the facial nerve and innervate the skin of the lower eyelid, the lateral surface of the nose and the upper lip. The following branches arise from the maxillary nerve and its continuation is the infraorbital nerve.
The zygomatic nerve (n. zygomaticus) goes to the skin of the cheek and the anterior part of the temporal area. It anatomizes with the lacrimal nerve (from the first branch of the trigeminal nerve).
The superior dental nerves (nn. alveolares superiors) form a plexus in the maxilla – the superior dental plexus (plexus dentalis superior) from which superior dental branches arise to the upper teeth and the superior gingival branches to arise the gums.
The ganglionic branches (nn. pterygopalatine, several (two-three) short branches connecting the maxillary nerve with the pterygopalatine ganglion.
The sphenopalatine ganglion (ganglion pterygopalatinum) is located in the pterygopalatine fossa medially and down from the maxillary nerve. In this ganglion, which relates to the vegetative nervous system, the parasympathetic fibres are interrupted; they run from the vegetative nucleus of the sensory root of the facial nerve (n. intermedius) to the lacrimal gland and to the mucous glands of the nose and palate as part of the nerve itself and further as the greater superficial petrosal nerve (a branch of the facial nerve).
The sphenopalatine ganglion gives off the following (secretory) branches.
(1) Nasal branches (rami nasalesposteriores) pass through the sphenopalatine foramen to the mucosal glands of the nose; the largest of these, the long sphenopalatine nerve (n. nasopalatine) passes through the incisive canal to the mucous glands of the hard palate; (2) the palatine nerves (nn. palatini) descend along the greater palatine canal and, after passing through the greater and lesser palatine foramina, innervate the mucosal glands of the hard and soft palates.
In addition to the secretory fibres, the nerves arising from the sphenopalatine ganglion contain also sensory nerves (from the second branch of the trigeminal nerve) and sympathetic fibres. Thus, the fibres of the sensory root (the parasympathetic part of the facial nerve) which pass along the greater superficial petrosal nerve, through the sphenopalatine ganglion, innervate the glands of the nasal cavity and palate and the lacrimal gland. The last pathway runs from the sphenopalatine ganglion through the ganglionic branches of the maxillary nerve (nn. pterygopalatini) into the zygomatic nerve and from it through an anastomosis into the lacrimal nerve.
The Mandibular nerve is the third division of 5th cranial nerve, begins from ganglion trigeminale, which is illustrated on Fig. 8.3. The mandibular nerve (n. mandibularis) contains, in addition to the sensory root, the whole motor root of the trigeminal nerve. The motor root arises from the motor nucleus and passes to the muscles originating from the maxillary arch. As a result the mandibular nerve innervates the muscles attached to the mandible, the skin covering it and other derivatives of the maxillary arch. On emerging from the cranium through the foramen ovale, it divides into two groups of branches.

Fig. 8.3. Neuroanatomy of the mandibular nerve:
1 – Trigeminal nerve, 2 – Gasserian ganglion, 3 – Mandibular nerve,
4 – Buccal nerve, 5 – Maxillary nerve, 6 – Ophthalmic nerve, 7 – Auriculotemporal nerve, 8 – Inferior alveolar nerve, 9 – Lingual nerve, 10 – Mental nerve (Stanley F. Malamed)
A. Muscle branches
Go to the muscles of the same name; nerve to the masseter (n. massetericus), deep temporal nerves (nn. temporalesprofundi), nerves to the medial and lateral pterygoid muscles (nn. pterygoideimedialis and lateralis), nerve to the tensor tympani muscle (n. tensoris tympani), nerve to the tensor palatine muscle (n. tensorisvelipalatini), mylohyoid nerve (n. mylohyoideus); the latter arises from the inferior dental nerve (n. alveolaris inferior), a branch of the mandibular nerve and also innervates the anterior belly of the digastric muscle.
B. Sensory branches
The buccal nerve (n. buccalis) goes to the mucosa of the cheek.
The lingual nerve (n. lingualis) descends along the medial side of the m. pterygoideusmedialis and lies under the mucous membrane of the floor of the oral cavity. After giving off the sublingual nerve to the mucosa of the floor of the mouth, it innervates the mucosa of the anterior two thirds of the back of the tongue. At the place where the lingual nerve passes between both pterygoid muscles, it is joined by a small thin branch of the facial nerve, chorda tympani, which emerge from the squamotympanic fissure. It contains parasympathetic secretory fibres that arise from the superior salivary nucleus of the sensory root of the facial nerve and pass to the hypoglossal and submaxillary salivary glands. It also contains gustatory fibres from the first two thirds of the tongue. The fibres of the lingual nerve itself distributed in the tongue are the conductors of general sensitivity (sense of touch, pain, and temperature).
The inferior dental nerve (n. alveolaris inferior), together with the artery of the same name, passes through the foramen mandibulae into the mandibular canal where after forming the inferior dental plexus it gives off branches to all the lower teeth. At the front end of mandibular canal the inferior dental nerve gives off a thick branch, the mental nerve (n. mentalis), which emerges through the foramen mentale and spreads in the skin of the chin and the lower lip. The inferior dental nerve is a sensory nerve with a small addition of motor fibres which leave it at the foramen mandibulae as part of the mylohyoid nerve (see above).
The auriculotemporal nerve (n. auriculotemporal) penetrates into the upper part of the parotid gland and, turning upward, passes to the temporal area accompanying the superficial temporal artery. Along the way the nerve gives off secretory branches to the parotid and salivary glands (whose origin is discussed below) and sensory branches to the temporomandibular articulation, to the skin of the anterior part of the concha of the auricle and the external acoustic meatus. The terminal branches of the auriculotemporal nerve supply the skin of the temple.
In the area of the third branch of the trigeminal nerve there are two ganglia belonging to the vegetative system by means of which the salivary glands are innervated. One of them, the otic ganglion (ganglion oticum), is a small round body located under the foramen ovale on the medial side of the mandibular nerve. It receives parasympathetic secretory fibres in the composition of the lesser superficial petrosal nerve which is a continuation of the tympanic nerve originating from the glossopharyngeal nerve. These fibres are interrupted in the ganglion and pass to the parotid gland by means of the auriculotemporal nerve, with which the otic ganglion is joined. Another small ganglion, the submandibular ganglion (ganglion submandibulare), is located at the anterior edge of the m. pterygoideusmedialis, above the submandibular salivary gland, under the lingual nerve. The ganglion is connected with the lingual nerve by branches. By means of these branches the fibres of chorda tympani pass to the ganglion where they terminatetheir continuation become the fibres arising from the submandibular ganglion, which innervate the submaxillary and sublingual salivary glands
The facial (7th) nerve
The facial nerve (n. facialis, s. intermediofacialis) is a mixed nerve. As a nerve of the second visceral arch it innervates the muscles developing from it, namely, all the facial-expression and part of the sublingual muscles. It also contains the efferent (motor) fibres emerging from its motor nucleus that pass to these muscles, and the afferent (proprioceptive) fibres arising from their receptors. It includes gustatory (afferent) and secretory (efferent) fibres belonging to the n. intermedius. The way of the facial nerve in the facial canal is presented on Fig. 8.4:

Fig. 8.4. The way of facial nerve:
1 – n. stapedius, 2 – foramen stylomastoideum, 3 – ganglion geniculi, 4 – ganglion pterygopalatinum, 5 – chorda tympani, 6 – n. lingualis, 7 – n. petrosus major
Anatomy and function of the salivary glands
The salivary glands are divided into major and minor glands. The major glands are paired parotid, submandibular, and sublingual glands. The minor glands are scattered throughout the oral and pharyngeal submucosa (including palate, lip, pharynx, nasopharynx, larynx, parapharyngeal space). All glands in general are derived from epithelial cells and consist of parenchyma (the secretory unit and associated ducts) and stroma (the surrounding connective tissue that penetrates and divides the gland into lobules).
Parotid gland
The parotid glands are the largest of the major salivary glands. They lie in the preauricular area extending from the zygomatic arch downwards to between the angle of the mandible and the mastoid process (Fig. 8.5).

Fig. 8.5. Anatomy of the parotid gland
The inferior portion, also known as the tail of the parotid, extends down to the anterior margin of the sternocleidomastoideus muscle. The anterior border corresponds approximately to the ascending ramus of the mandible. Each parotid gland is divided by the facial nerve into a superficial lobe and a deep lobe. Superficial lobe arise lateral to the facial nerve, and a deep lobe arises deep to the facial nerve, into the parapharyngeal space. This is an artificial division and no true anatomical plane exists between the superficial and the deep lobe. A normal parotid gland consists of 80 % superficial lobe and 20 % deep lobe.
The facial nerve enters the parotid gland from the stylomastoid foramen. Before entering the posterior portion of the parotid gland, three motor branches are given of to innervate the posterior belly of the digastric muscle, the stylohyoid muscle, and the postauricular muscles. Shortly after entry (approximately 1.3 cm from the stylomastoid foramen), the facial nerve divides into an upper and lower division. The upper division gives off a temporal branch that supplies the muscles of the forehead and eye, a zygomatic branch that supplies the muscles of the eye, and occasionally a buccal branch that supplies the muscles of the nostril and upper lip. The lower division gives off a mandibular branch that supplies the muscles of the lower lip and a cervical branch that supplies platysma in the neck. The lower division often also gives off the buccal branch.
Other nerves, located within the parotid gland are the great auricular nerve and auriculotemporal nerve. The great auricular nerve is a sensory branch of the cervical plexus, which innervates the posterior portion of the pinna and the lobule. The nerve parallels the external jugular vein along the lateral surface of the sternocleidomastoid muscle to the tail of the parotid gland, where it splits into anterior and posterior branches. The great auricular nerve is often injured during parotidectomy, which can result in long-term sensory loss in the lobule. The auriculotemporal nerve is a branch of the mandibular nerve. After exciting from the foramen ovale, the nerve traverses superiorly to innervate the skin and scalp immediately anterior to the ear. Its course runs through the parotis, parallel to the superfcial temporal vessels and anterior to the external auditory canal.
The parotid gland is drained by the parotid duct, which opens into the mouth opposite the second upper molar tooth.
An accessory parotid gland may also be present lying anteriorly over the masseter muscle between the parotid duct and zygoma.
Submandibular gland
The submandibular gland is the second largest major salivary gland. It is located in the submandibular triangle bordered anteriorly by the digastric muscle, posteriorly by the stylomandibular ligament and superiorly by the mandibular body (Fig. 8.6). Also lying within the triangle are the submandibular lymph nodes, facial artery and vein, mylohyoid muscle, and the lingual, hypoglossal, and mylohyoid nerves. The submandibular gland has both mucous and serous cells. It is drained by the submandibular duct (Wharton’s duct), which goes forwards and upwards and opens laterally to the frenulum in the floor of the mouth behind the lower incisors. The marginal mandibular branch of the facial nerve, the lingual nerve and the hypoglossal nerve are closely linked to the submandibular gland and can be injured during surgical interventions on the submandibular gland. The marginal mandibular nerve supplies the muscles of the lower lip and damage to this nerve will leave the patient with deformity. The lingual nerve supplies sensation to the anterior two-thirds of the tongue, whereas the hypoglossal nerve supplies motor function to the tongue muscles.
Sublingual gland
The sublingual gland is the smallest of the major salivary glands and lies under the mucosa of the floor of the mouth near the lingual frenulum, superior to the mylohyoid muscle and deep to the sublingual folds (Fig. 8.6). It is closely associated with the lingual nerve, which lies medial to the gland. Sublingual gland consists mainly of mucous acinarcells, and drains into the mouth by small ducts (located on the sublingual fold), as well as by ducts that open directly into the submandibular gland duct. The openings for the sublingual gland, or the sublingual caruncles, are located near the midline in the ventral tongue.

Fig. 8.6. Anatomy of the submandibular and sublingual glands
Minor Salivary Glands
The number of minor salivary glands ranges from 600 to 1000. Their size is usually from 1 to 5 mm. Located in the submucose space of the lips, tongue, buccal area, and palate, they can also be found along the tonsils, supraglottis, larynx, and paranasal sinuses. Each gland has a single duct which secretes, directly into the oral cavity, saliva which can be serous, mucous or mixed.
Physiology of salivary Glands
Normal function and health of the mouth depend on normal secretion of saliva by the major and minor glands. This function is very important for digestion, lubrication, and protection of the oral cavity. About 1-1.5 l of saliva is produced by an adult each day. The parotid gland produces a serous secretion whereas the sublingual and submandibular gland produces two-thirds mucous and one-third serous secretion. In the unstimulated salivation, the submandibular gland produces most saliva but on stimulation most saliva (two thirds of secretion) is produced by the parotid gland. Saliva participates in the digestion of carbohydrates and fats through two main enzymes (lipase, amylase). The mucus constituent of saliva facilitates the lubrication of food particles during the act of chewing. Lubrication eases the processes of swallowing assists taste and is important for speech. The antibacterial properties of saliva are due to its many protective organic constituents SIgA. lysozyme, lactoferrin, ext. Saliva also serves as a protective buffer for the mouth by diluting harmful substances and lowering the temperature of solutions that are too hot.
Anatomy of the temporomandibular joint
The temporomandibular joint (Fig. 8.7) is the joint of the jaw and is frequently referred to as TMJ. There are two TMJs, one on either side, working in unison. The name is derived from the two bones which form the joint: the upper temporal bone which is part of the cranium (skull), and the lower jaw bone called the mandible. The TMJ is a ginglymoarthrodial joint, referring to its dual compartment structure and function (ginglymo- and arthrodial). The condyle articulates with the temporal bone in the mandibular fossa. The mandibular fossa is a concave depression in the squamous portion of the temporal bone.

Fig. 8.7. Anatomy of the temporomandibular joint:
1 – lateral pterygoid muscle (superior belly),
2 – lateral pterygoid muscle (inferior belly),
3 – mandibular fossa,
4 – articular cartilage,
5 – disc – intermediate zone,
6 – disc – iposterior band,
7 – disc – anterior band,
8 – articular cartilage,
9 – mandibular condyle,
10 – bilaminar (retrodiscal) zone,
11 – posterior capsule,
12 – anterior capcule (superior attachement),
13 – anterior capcule (inferior attachement)
Capsule and articular disc
The capsule is a fibrous membrane that surrounds the joint and incorporates the articular eminence. It attaches to the articular eminence, the articular disc and the neck of the mandibular condyle. The unique feature of the TMJs is the articular disc. The disc is composed of fibrocartilagenous tissue (like the firm and flexible elastic cartilage of the ear) which is positioned between the two bones that form the joint.
The TMJs are one of the only synovial joints in the human body with an articular disc, another being the sternoclavicular joint. The disc divides each joint into two. The lower joint compartment formed by the mandible and the articular disc is involved in rotational movement (opening and closing movements). The upper joint compartment formed by the articular disk and the temporal bone is involved in translational movements (sliding the lower jaw forward or side to side). The part of the mandible which mates to the undersurface of the disc is the condyle and the part of the temporal bone which mates to the upper surface of the disk is the glenoid (or mandibular) fossa.
The anterior portion of the disc splits in the vertical dimension, coincident with the insertion of the superior head of the lateral pterygoid. The posterior portion also splits in the vertical dimension, and the area between the split continues posteriorly and is referred to as the retrodiscal tissue. Unlike the disc itself, this piece of connective tissue is vascular and innervated, and in some cases of anterior disc displacement, the pain felt during movement of the mandible is due to the condyle pressing on this area.
There are three ligaments (Fig. 8.8, 8.9) associated with the TMJ: one major and two minor ligaments. The major ligament, the temporomandibular ligament, is actually the thickened lateral portion of the capsule, and it has two parts: an outer oblique portion (OOP) and an inner horizontal portion (IHP). The minor ligaments, the stylomandibular and sphenomandibular ligaments are accessory and are not directly attached to any part of the joint. The stylomandibular ligament separates the infratemporal region (anterior) from the parotid region (posterior), and runs from the styloid process to the angle of the mandible. The sphenomandibular ligament runs from the spine of the sphenoid bone to the lingula of mandible.

Fig. 8.8. The temporomandibular joint:
1 – temporal bone, 2 – zygomatic process, 3 – mandible

Fig. 8.9. The temporomandibular (exterior sight) joint (interior sight):
1 – spine of sphenoid bone, 2 – sphenomandibular ligament, 3 – mandibular foramen, 4 – mylohyoid groove, 5 – capsula, 6 – temporomandibular ligament, 7 – styloid process, 8 – stylomandibular ligament
These ligaments are important in that they define the border movements, or in other words, the farthest extents of movements, of the mandible. However, movements of the mandible made past the extents functionally allowed by the muscular attachments will result in painful stimuli, and thus, movements past these more limited borders are rarely achieved in normal function.
Sensory innervation of the temporomandibular joint is derived from the auriculotemporal and masseteric branches of V3 (otherwise known as the mandibular branch of the trigeminal nerve). These are only sensory innervation, recall that motor is to the muscles.
Its arterial blood supply is provided by branches of the external carotid artery, predominately the superficial temporal branch. Other branches of the external carotid artery namely: the deep auricular artery, anterior tympanic artery, ascending pharyngeal artery, and maxillary artery – may also contribute to the arterial blood supply of the joint.
The specific mechanics of proprioception in the temporomandibular joint involve four receptors. Ruffini endings function as static mechanoreceptors which position the mandible. Pacinian corpuscles are dynamic mechanoreceptors which accelerate movement during reflexes. Golgi tendon organs function as static mechanoreceptors for protection of ligaments around the temporomandibular joint. Free nerve endings are the pain receptors for protection of the temporomandibular joint itself. In order to work properly, there is neither innervation nor vascularization within the central portion of the articular disc. Had there been any nerve fibers or blood vessels, people would bleed whenever they moved their jaws; however, movement itself would be too painful.
Jaw movements
During jaw movements, only the mandible moves. Normal movements of the mandible during function, such as mastication, or chewing, are known as excursions. There are two lateral excursions (left and right) and the forward excursion, known as protrusion. The reversal of protrusion is retrusion.
The mandible is moved primarily by the four muscles of mastication: the masseter, medial pterygoid, lateral pterygoid and the temporalis. These four muscles, all innervated by V3, or the mandibular division of the trigeminal nerve, work in different groups to move the mandible in different directions. Contraction of the lateral pterygoid acts to pull the disc and condyle forward within the glenoid fossa and down the articular eminence; thus, action of this muscle serves to open the mouth. The other three muscles close the mouth; the masseter and the medial pterygoid by pulling up the angle of the mandible and the temporalis by pulling up on the coronoid process.
Chapter 9. Examination and methods of diagnostics in oral and maxillofacial surgery. Anaesthesia in oral surgery
History
A full and accurate history is of paramount importance in assessment of a patient. In some cases, the history may provide the diagnosis while in the remainder it will give essential dues to the nature of the problem. The approach to history bating needs to be tailored 1o the type of complaint being investigated.
It is important to have a systematic approach to taking a history. A consistent series of questions will avoid inadvertently missing an important clue. Use “open” rather than “closed” (those usually eliciting a yes/no response) questions wherever possible to avoid leading the pattern. Record the patient’s own responses rather than paraphrasing. The history will cover: the complaint, the history of the complaint, past dental history, social and family history, medical history.
Examination. Extra-oral examination
Like history taking, examination necessitates a systematic approach. As a general rule, use your eyes first, then your hands to examine a patient.
Start with the extra-oral examination before proceeding to examine the oral cavity.
Take time to look at the patient. This may seem obvious but will identify swellings, skin lesions and facial palsies. Facial pallor may indicate anaemia, or that the patient may be about to faint. This process of observation will start while you are taking the history.
Visual areas would cover: general patient condition, symmetry, swellings, lips/perioral tissues.
Palpation would cover: lymph nodes, temporomandibular joint (TMJ), salivary glands, problem-specific examination.
Lymph node examination
The major lymph nodes of the maxillofacial area and neck are shown on Fig. 9.1. The submental, submandibular and internal jugular nodes (jugulo-digastric and jugulo-omohyoid node being the largest) are of particular importance because these receive lymph drainage from the oral cavity. Examination of the nodes should be systematic, although the order of examination is not critically important.

Fig. 9.1. The principal lymph nodes in the head and neck (Ben Pansky illustration)
To palpate the nodes, the examiner should stand behind the patient while he/she is seated in an upright position. Use both hands (left hand for the left side of the patient etc.). A common sequence would be to start in the submental area, working back to the submandibular nodes then further back to the jugulo-digastric node.
Then continue by palpation of the parotid area downwards to the retromandibular area and down the cervical chain of nodes. When a node is perceived as enlarged, record the texture: a hard node of a metastasising malignancy contrasts well with a tender, softer node in an inflammatory process.
A detailed examination of the TMJ is probably only needed when a specific problem is suspected from the history. As with the TMJ, examination of the salivary glands is only required when the history suggests this is relevant.
The examination will be made in the light of the symptoms reported by the patient but the examiner may detect swelling, sensory or motor disturbance that the patient has not noticed.
The procedure for examination of a swelling or a lump must encompass a range of observations: anatomical site, shape and size, colour, single or multiple, surface texture/warmth, tenderness, fluctuation, sensation/pulsation.
Consistency can be informative, ranging from swelling of a lipoma, through “cartilage hard” pleomorphic adenomas and “rubbery hard” nodes in Hodgkin’s disease to the “rock hard” nodes of metastatic malignancy. Tenderness and warmth on palpation indicates an inflammatory process. Fluctuation indicates the presence of fluid. To fluctuation, place two fingers on the swelling and press down with one finger. If fluid is present, the other finger will record an upward pressure. Pulsation in a swelling will indicate direct (i.e. it is a vascular) or indirect involvement (i.e. in immediate contact) of an artery. The presence of sensory disturbance is usually identified initially by the patient in the history. It is important to identify the extent of the affected area and the degree of alteration in sensation. It is best to use a fairly fine, but bluntended, instrument for this at first, for example the handle of a dental mirror. First, run the instrument gently over what is assumed to be a normal area of that the patient knows what to expect. Then repeat this over the symptomatic area, asking the patient to say whether they can feel anything. Record the area of altered sensation in the notes using a drawing.
The degree of alteration in sensation can be assessed by using different “probes”. A teased-out piece of cotton wool can be used or, where anaesthesia appears to be profound, a sharp probe can be (carefully) tried.
The extent of the area of paraesthesia or anaesthesia will tell you the particular nerve, or branch of a nerve, involved (Fig. 9.2). This will, in turn, inform you about the possible location of the underlying lesion. For example, a patient with disturbed sensation of the upper lip has a lesion affecting the maxillary division of the trigeminal nerve. If this is the sole site of sensory deficit, it suggests a lesion closer to the terminal branches of this cranial nerve (e.g. in the maxillary sinus). In contrast, if sensory deficiencies are simultaneously present in other branches of the nerve, it suggests that the lesion is more centrally located.

Fig. 9.2. Cutaneous sensory innervation of the head and neck by the trigeminal and cervical nerves.
Trigeminal nerve: V1 ophthalmic division, V2 maxillary division, V3 mandibular division. Cervical nerve: C2–C4 branches
While paralysis or motor disturbance may be reported as a symptom by the patient, it may initially be identified during an examination. In the maxillofacial area, the motor nerves that are likely to be under consideration are the facial nerve, the hypoglossal nerve (see below) and the nerves controlling the muscles that move the eyes. Disturbance in function of the facial nerve will result in effects on the muscles of facial expression. Paralysis of the lower face indicates an upper motor neurone lesion (stroke, cerebral tumour or trauma). Paralysis of all the facial muscles (on the affected side) indicates a lower motor neurone lesion. The latter is seen in a large number of conditions but, for the dentist, important causes include Bell’s palsy (Fig. 9.3), parotid tumours, a misplaced inferior dental local anaesthetic and trauma.

Fig. 9.3. Sensory innervation of the oral cavity is principally from the trigeminal nerve (V) while the glossopharyngeal nerve (IX) supplies the posterior third of the tongue. NB Taste sensation in the anterior two-thirds of the tongue is provided by fibres of VII nerve origin passing through the lingual nerve.
ASA – Anterior superior alveolar nerve.
PSA – Posterior superior alveolar nerve
Intra-oral examination
Again, a systematic approach is essential to avoid being distracted by the first unusual finding you encounter. The examination must include lips, cheeks, parotid gland orifices, buccal gingivae, lingual gingivae and alveolar ridges in edentulous areas, hard palate, soft palate, dorsal surface of the tongue, ventral surface of the tongue, floor of mouth, submandibular gland orifices and, finally, the teeth. Clinicians will have their own sequence of examination, but it is the thoroughness of the examination that is important, not the order in which the areas of the mouth are examined.
Once the general intra-oral examination is complete, a problem-specific examination can proceed. This is tailored to the clinical problem.
The examination of an intra-oral swelling or lump is essentially the same as that described above as part of the extra-oral examination. Most oral swellings are inflammatory, caused by periapical or periodontal infections. However, the minority of oral swellings and lumps that are non-dental encompasses a wide range of conditions, the details of which form a significant part of this book.
Examination of an ulcer should include assessment of eight important characteristics: site, single/multiple, size, shape, base of the ulcer, edge, pain, time period.
Visual inspection is essential but palpation is also an important part of the examination of an ulcer. Gloves must be worn for palpation and the texture of the ulcer base; margin and surrounding tissues should be ascertained by gentle pressure. Malignant neoplasms tend to ulcerate, and these often feel firm, hard or even fixed to deeper tissues. A raised margin is a suspicious finding, as the presence of necrotic, friable tissue in the ulcer base and bleeding on lightly pressing. Healing traumatic ulcers tend to be painful on palpation and they feel soft and gelatinous.
The finding of an ulcer on examination may necessitate taking additional history, for example, if a traumatic ulcer is suspected, direct questioning may prompt the patient to recall the injury.
If multiple ulcers are detected, this may lead to further enquiries about any previous history of recurrent oral ulceration or specific gastrointestinal diseases. It is surprising how often ulceration is discovered that the patient is not aware of. When an ulcer is found, it is vital that a detailed record of the history and examination findings is made. Any oral mucosal ulcer that does not heal within 3 weeks should be considered as possibly malignant and urgent referral must be arranged.
Certain ulcers have a tendency to occur in particular oral sites, for example squamous cell carcinomas are most common on the lower lip, in the floor of mouth and the lateral border of the tongue. On the other hand traumatic ulcers are most common on the lateral border of the tongue and buccal mucosa in the occlusal plane. Ulceration on the lower lip is also a common site for traumatic ulceration, particularly following administration of an inferior dental block or after a sports injury. Site is also important in diagnosis, for example, minor aphthae are restricted to lining mucosa and can be ruled out if ulceration is occurring on the hard palate or gingiva.
Size and shape can also be helpful, for example linear fissure-type ulcers may be seen in Crohn’s disease, though aphthae are more usual. The shape of a traumatic ulcer may reveal the cause, for example semicircular ulcers are sometimes caused by the patient’s fingernail. Bizarre persistent ulceration is sometimes a result of deliberate self-harm, unusual habits or taking recreational drugs; in such cases, diagnosis can be difficult as the patient may deny knowledge of the causation. Minor aphthae have characteristic size and site features, which can distinguish them from major and herpetic form aphthae.
Pain, as mentioned above, is a feature of inflammatory and traumatic ulcers, while in the early stages a malignant ulcer is often painless. Advanced malignant ulcers eventually tend to become painful as a result of infection and involvement of adjacent nerves. Presentation with a painful traumatic ulcer is common in dentistry. The cause should be eliminated if possible (e.g. smoothing or replacement of an adjacent fractured restoration) symptomatic treatment such as analgesic mouthwash prescribed and most importantly, review arranged to ensure that healing has occurred.
Paraesthesia/anaesthesia
The principles of examination are described above for extra-oral examination. Once again, you need good anatomical knowledge of the nerves supplying different parts of the oral cavity to interpret the possible site of the underlying pathological process.
Within the oral cavity, motor disturbance is seen in the tongue (due to damage to the function of the hypoglossal nerve) and the soft palate (due to lesions affecting the vagus nerve). With hypoglossal nerve lesions, there is deviation of the tongue towards the affected side in protrusion attempting. There is also a problem with speech, with “lingual” sounds such as “l”, “t” and “d”.
Tooth problems
Tooth problems are, of course, the most common problems facing the dentist. The context is usually pain or swelling. A standard method of examination helps in a diagnosis. You should not simply hammer the suspect tooth with the mirror handle and take a radiograph as your method of assessment! Indeed, careful examination may establish a diagnosis and thus avoid any need for radiography or other special tests. Examination will involve:visual, probe restorations, assess mobility, periodontal probing, thermal tests, pressure tests.
Visual examination will reveal gross caries, the presence of restorations, signs of tooth deposit and gingivitis. A probe will allow tactile assessment of restoration margins.
Mobility should be assessed manually Periodontal probing should be carried out to assess pockets, the presence of calculus/overhangs and, ultimately, bone loss.
A basic test of vitality should always be performed using a cotton wool pledget soaked with ethyl chloride (cold stimulus) and sometimes heated gutta-percha (hot stimulus). While these are usually sufficient to reveal a hypersensitive tooth with pulpitis, an electrical pulp test can be used to assess vitality in some cases.
Pressure sensitivity should be assessed using direct finger pressure and, when this does not evoke a response, can be supplemented by percussion using a dental mirror handle. This will assess whether periodontitis is present or not. However, if a single cusp is tender to percussion, this may be indicative of cracked cusp syndrome.
Special investigations
Evidence-based laboratory medicine
Whenever special tests are undertaken, it is important to consider medicolegal issues, informed consent, appropriateness of the test and the evidence base for the use of any particular laboratory investigation. It is always necessary to have a differential clinical diagnosis in mind when requesting an investigation. Certain tests, such as those for human immunodeficiency virus (HIV) infection, require pre-test counselling and informed consent; such tests should be undertaken only by specialists in the field. When requesting a test, it is vital to possess the knowledge and skills so that the result can be acted upon appropriately. In some situations, for example suspected oral cancer, it may be wise to refer the patient directly to a specialist for a biopsy.
Most laboratories can advise on current codes of practice relating to the above issues and may give reference ranges and advice, for example about a particular biopsy result. Sending pathological material through the post is potentially hazardous and current regulations must be followed. It should be remembered that laboratory tests require considered interpretation in conjunction with the patient’s history. Some tests have low sensitivities – for example certain cytology tests, and a negative result cannot be relied upon to exclude disease. The test may need to be repeated, or an alternative test with a higher sensitivity used. Other tests have low specificity and a positive result does not necessarily indicate that disease is present. Examples include low-titre autoantibodies, which may be detected in the serum but which can be of no clinical significance. The receiver-operator curve (ROC) for any laboratory test can be plotted to guide clinical use. Use of resources is also important, particularly when expensive reagents or complex procedures are required.
Microbiology. Diagnosis of infection and determination of sensitivity of the infectious agent to pharmacotherapeutic agents are the principal requirements for microbiology teste in dentistry.
Viruses. Most often a clinical diagnosis is adequate for acute or recurrent viral oral infections such as herpes simplex. A viral swab can be used to collect virus from fresh vesicles and must be forwarded in special transport medium to the virology laboratory. Other virus infections such as glandular fever can be detected by looking for a rising litre of antibodies in the patient’s serum.
Bacteria. Bacterial infections in the oral cavity, jaws and salivary glands may be identified by forwarding a swab or specimen of pus to the laboratory, with a request for culture and antibiotic sensitivity.
Fungi. Candida sp. is the most common organism to cause oral fungal infection. Often clinical diagnosis is adequate; for example in denture-related stomatitis, the clinical history and appearance of the mucosa may be sufficient. Direct smears from the infected mucosa and the denture-fitting surface can be stained by the periodic acid-Schiff or Gram’s method. The presence of typical pseudohyphae indicates candidal proliferation consistent with infection. Swabs or oral rinses can be used to discriminate the various Candida species and heavy growth suggests infection rather than carriage.
Aspiration biopsy
Fluid from suspected cysts can be collected with a standard gauge needle and syringe: radicular cysts contain brown shimmering fluid because of the presence of the cholesterol crystals, whereas odontogenickeratocysts contain pale greasy fluid, which may include keratoticsquames. Infection after aspiration biopsy can be a problem and indeed the technique tends to be restricted lo atypical cystic lesions where neoplasia is suspected. Fine needle aspiration biopsy (FNAB) can be used to obtain a sample of cells from a solid tumour and is a hospital procedure.
Incisional / excisional biopsy
Mucosal biopsy is one of the more common investigations used by dentists in primary and secondary care. Tissue is removed under local or general anaesthesia using sharp dissection to avoid crushing the specimen. It is fixed in at least 10 times its volume of 10 % neutral buffered formalin or similar fixative. It is then forwarded to the histopathology or specialist oral and maxillofacial pathology laboratory.
Excisional biopsy. The entire lesion is removed and submitted for diagnosis. It is suitable for benign polyps, papillomas, mucocoeles, epulides and other small reactive lesions.
Incisional biopsy. A representative sample of a larger lesion is taken for diagnosis prior to treatment. This is a specialist procedure requiring some expertise and experience. It is used for generalised mucosal disorders such as lichen planus or for the diagnosis of other red and white patches. An important consideration is obtaining a sample from an appropriate area. Nonhealing ulcers are often investigated by incisional biopsy; here it is important to include the margin of the ulcer with some normal tissue and to obtain a sufficiently large sample, (normally 10 mm × 10 mm) to identify or exclude cancer. Sometimes fresh tissue is required for diagnosis, for instance in the vesiculo-bullous diseases where immunofluorescence is needed. Special arrangements must be made with the laboratory when such tests art-planned.
Haematology
Patients presenting with oral manifestations of haematological disease are normally referred for specialist opinion. Full blood count and assay of haematinics is an important investigation for patients presenting with lingual papillary atrophy or recurrent oral ulceration, for example. Coagulation studies and platelet counts may be required when excessive bleeding is encountered. Patients on anticoagulant therapy should have their INR (international normalised ratio) checked before any surgical procedure is undertaken.
The Sickledex test may be used to screen for sickle cell anaemia prior to giving general anaesthesia in situations of urgency. The blood sample should be subjected to haemoglobin electrophoresis.
Biochemistry
Biochemical investigations are used principally in specialist clinics to investigate patients presenting with oral manifestations of systemic disease, for example estimation of alkaline phosphatase in Paget’s disease of bone, and serum calcium to exciude hyperparathyroidism when a giant cell granuloma is diagnosed. Biochemical estimation of cyst fluid for protein content is sometimes undertaken as part of diagnosis of odontogenickeratocyst.
Immunology
Advances in knowledge and methods in immunology have resulted in a large number of laboratory immunological investigations, available in specialist laboratories. Sometimes diagnostic arrays of tests are offered by the laboratory. Examples of tests in dentistry include detection of antibodies against extractable nuclear antigens, including SS-A and SS-B, for the diagnosis of Sjogren’s syndrome and autoantibodies in vesiculobullous diseases.
HIV testing should only be undertaken by specialists and does not fall directly into the remit of dentistry. It requires informed patient consent and counselling. Dentists must be able to recognise the oral manifestations of immunodeficiency states and arrange proper referral.
Imaging
Imaging is an important special test in dentistry and oral and maxillofacial surgery, because X-ray exposure carries a quantifiable risk, X-ray examinations should be selected according to specific selection (referral) criteria. Other imaging investigations not using ionising radiations (ultrasound and magnetic resonance imaging) have their place and should be used in preference to X-ray techniques (radiography and computed tomography) when they can provide the same or better diagnostic information. Selection criteria should be based upon the diagnostic efficacy of the technique for the disease process being examined. For example, approximal caries diagnosis is best aided by bite wing rather than other radiographs. There are a large number of imaging techniques available and these are summarised below. Details of the specific uses of these techniques are given where appropriate in subsequent chapters.
Plain films with or without arthrography are occasionally used (film placed by Parma, Schuller). Transpharyngeal projection is also called as intracranial view, Parma projection, or McQueen projection (Fig. 9>.4).

Fig. 9.4. Transpharyngeal projection (Parma)
This projection demonstrates the condylar process from the midmandibular ramus to the condyle. This technique helps in the diagnosis of fractures of the condyle and the condylar neck and in detecting alterations in the condylar morphology.
I. Diagram and photograph of positioning of the skull for the TMJ film as modified according to Schuller (Fig. 9.5).

Fig. 9.5. Diagram and photograph of positioning of the skull for the TMJ film
To portray the condyles as closely as possible along their long axes. The vertical median sagittal plane should be approximately parallel to the film cassette, with a horizontal angle of no more than 10° to the cassette and a vertical angle of no more than 25°.
II. Detail of the positioning for the Schuller projection with mouth closed, and mouth open. Note that during the second exposure with the mouth open (right) only the mandible has been moved to the open position, otherwise variation in the depiction of structures will occur between the dims taken with mouth closed and open, and this could hamper interpretation.
Conventional radiography
This is familiar to every dentist and student in the forms of bitewing, periapical, occlusal and panoramic radiography.
Other maxillofacial radiographs should be used in addition to the traditional “dental” techniques when appropriate. While detailed prescription of radiographs depends on the particular needs of each patient, some general guidelines are useful and are given in Table 9.1.
Table 9.1. Guidelines of radiographic projections
| Anatomical site to be examined |
Radiographic projections |
Anterior mandible
Body of mandible
Third molar area, angle and ramus of mandible
Condyle temporomandibular joint |
Periapical, oblique and true occlusal views.
Periapical, true occlusal, panoramic {or lateral oblique) views Periapical and true occlusal [third molar area only).
Panoramic (or lateral oblique) view Poster-anterior (PA) view. |
| Panoramic (or lateral oblique) view Transpharyngeal view Transcranialviews (open/closed) Reverse Towne’s view (modified PA projection). |
– |
Anterior maxilla Posterior maxilla Maxillary sinus
Parotid gland (for calculi) Submandibular gland (for calculi) |
Periapical and oblique occlusal views. Periapical, oblique occlusal, panoramic (or lateral oblique) views Periapical, oblique occlusal, panoramic (or lateral oblique) views Occipitomental view Intra-oral soft tissue view ot parotid papilla area
Localised PA/antero-posterior of face
with cheek blown out
True occlusal of floor of mouth
Modified oblique occlusal for
submandibular gland
(Dental film placed by V. S. Kovalenko) |
Contrast investigations
Some radiological techniques use radio-opaque contrast media injected into parts of the body. In the maxillofacial area, they can be used to demonstrate fistulae and sinuses and in vascular studies (angiograms). However, they are most commonly used for sialography and arthrography of the TMJ.
Computed tomography
Computed tomography (CT) is also known as CAT scanning (Fig. 9.6). It provides primarily axial cross-sectional images and uses X-rays. The computer calculates the X-ray absorption (and thus indirectly the density) of each unit volume (voxel) of tissue and then assembles the information into an image made up of many pixels (picture elements). Each pixel is given a grey-scale value according to its density (Hounsfield scale). CT is useful for evaluation of bony deformaties (Fig. 9.7). Dense bone is white, most soft tissues are mid-grey, fat is dark grey and air is black. Metals are beyond the comprehension of the computer software, so dental fillings cause artefacts.

Fig. 9.6. A typical computed tomographic scan

Fig. 9.7. Computed tomography (erosion of the condyle)
Clinical maxillofacial applications include:
- large maxillary cysts /benign tumours;
- malignancy arising in the antrum;
- soft tissue masses;
- oral carcinoma.
Images can be reconstructed in two or three dimensions (Fig. 9.8). In maxillofacial work, reconstructions are invaluable for implantology and useful in major facial trauma and orthognathic surgical treatment planning.

Fig. 9.8. Computed tomography, 3D-reconstruction
CT is associated with a relatively high dose of radiation. Generally, the thinner sections (and the better the fine detail) require the higher the dose.
Diagnostic ultrasound
Ultrasound uses the principle that high frequency (3.5–10 MHz) sound waves can pass through soft tissue but will be reflected back from tissue interfaces. The echoes can be detected to produce an image. The sound is transmitted and detected by the same hand-held transducer. Imaging is “real-time”.
Clinical maxillofacial applications include: soft tissue lumps in the neck and the salivary glands Fig. 9.9).

Fig. 9.9. Ultrasound image
Radioisotope imaging
Radioisotope imaging is also known as nuclear medicine. The technique uses radioisotopes (usually gamma ray emitters) tagged on to pharmaceuticals, which are usually injected into the bloodstream. By choosing the radiopharmaceutical appropriately, particular organs or types of tissues will become radioactive. The patient is placed in front of a gamma camera, which detects the emitted radiation to give an image of physiological activity. It is not an anatomical imaging modality.
Clinical maxillofacial applications include:
- salivary scanning (particularly in Sjogren’s syndrome): uses sodium pertechnetate-99m (Fig. 9.10);
- bone scanning (for bone tumours, metastatic disease, Paget’s disease, arthritis and condylar hyperplasia): uses technetium-99m-labelled methylene bisphosphonate.

Fig. 9.10. Radioisotope scans of the salivary glands (frontal view). Foci of activity are visible in the two major salivary glands, in the mouth and at the bottom of the image, the thyroid gland
Magnetic resonance imaging
Magnetic resonance imaging is also known as MR, MRI or NMR. In this technique, patients are placed into an intense magnetic field, forcing their hydrogen nuclei (principally in water molecules) to align in the field. Radiofrequency waves are pulsed into the patient, the hydrogen nuclei “wobble”, producing an alteration in the magnetic field. This induces an electric current in coils placed around the patient. The computer is capable of reading this and, because different tissues contain different amounts of hydrogen (in water), of producing an image that, superficially, is like a CT scan. However, imaging can be in any plane (axial, sagittal or coronal).
Clinical maxillofacial applications include:
- anything CT can do (but no ionising radiation);
- imaging of the TMJ.
MRI is noninvasive and is the best technique for evaluating disc morphology and position (Fig. 9.11). In general, fibromyalgia requires no imaging study. Type I and II internal derangements require MRI, whereas ankylosis and other bony disorders are best examined by computed tomography. Of note arthroscopy is often employed as well.

Fig. 9.11. MRI (Magnetic Resonance Imaging), disk injury
Chapter 10. Anaesthesia in oral surgery
Painlessness of operations in oral and maxillofacial surgery is the same basic demand, as well as painlessness of surgical interventions in other areas. Development of surgery of this area is obliged much more to successes of a local anaesthesia. Nevertheless, it is not always possible to do without the general anaesthesia at operations in the oral cavity. The necessity of carrying out long and volumetric interventions demands carrying out general anaesthesia and thorough preoperative preparation. Therefore the dentist should know well the basic properties of narcotics, indications and contraindications to their application, to study technique of narcosis and treatment of known complications.
Analgesia is the elimination of painful sensations in the course of surgical or diagnostic manipulations.
Anaesthesia is the eliminations of all sensations (including pain) in the course of surgical or diagnostic manipulations.
Anaesthesia may be:
- General (narcosis), which is divided into inhalation with mask or endotracheal (through the nose) and non-inhalation (intramuscular, intravenous, rectal, epidural).
- Local.
Patients with maxillofacial pathologies constitute a particular category with a peculiar neurotic status. This feature is combined with full-blown pain due to topographical and function peculiarities of the maxillofacial area (a lot of receptors, cranial nerves, speech, breathing and masticate functions). The knowledge of the methods and agents of local anaesthesia can make it easier to carry out surgical operations in the maxillofacial area painlessly.
The general anaesthesia
The general anaesthesia (narcosis) means the condition of the convertible inhibition of the central nervous system (cns) is achieved by pharmacological agents, influence of physical or mental factors. It assumes suppression of perception of pain stimulations, achievement of neurovegetative blockade and muscular relaxation, deenergizing of consciousness, maintenance of an adequate gas exchange and circulation, regulation of metabolic processes.
General anaesthesia includes narcosis, nla, ataralgesia, central analgesia, audioanaesthesia and hypnosis, electronarcosis and acupuncture, electrical puncture. Neuroleptanalgesia (nla) is the loss of pain sensitivity, which is achieved due to rational cooperation of deep analgesia and neurolepsia by the introduction of analgesic and neuroleptic drugs.
Narcosis (general anaesthetizing) is temporary, reversible, artificially caused, (for example, by medicines) change of functions of organism (mainly is braking of cns functions), that is accompanied by narcosis triad: 1) loss of consciousness (sleep, fainting fit) – is achieved by introduction of anesthetic; 2) loss of sensitiveness of different types, among them – pain (analgesia), suppression of reflex activity (areflexia) – the response to external irritants (for example, to operative interference) – is achieved by introduction of analgesics (opioids more frequent); 3) myorelaxation, or skeletal muscle relax (deep or shallow) is achieved by introduction of muscle relaxants.
Ataralgesia – sort of nla, when ataraxia and analgesia are achieved by the administration of tranquilizers and analgesics. Central analgesia is the elimination of pain sensations due to introduction of great doses of analgetics. Audioanestesia is based on stimulation of the auditory analyzer by the certain frequency signal, which causes inhibition in other parts of the brain cortex.
Indications for narcosis
In the maxillofacial area it’s indicated for carrying out long-term and traumatic surgical interventions which are combined with the risk of the airways obstruction. The indications and containdications are distinguished in Table 10.1.
Potentiation is the strengthening of pharmacological action of anesthetic by other medicines, which totally has a greater effect, than the action of these preparations solely.
Premedication
Premedication is the application of medicines during the preparation of the patient. The anesthetist select 3 variants of premedication application:
Absence of premedication – more frequent in small and exigent surgical interferences.
Table 10.1. The indications and containdications for narcosis
| Narcosis on an outpatient basis |
| Indications |
Contraindications |
| general allergic reactions on local anaesthetics |
acute disease of parenchymatous organs |
| Indications |
Contraindications |
low effect or impossibility of local anaesthesia
the patient is mentally unbalanced mental deficiency traumatic interventions surgical interventions at children
Specific
premorbid background anesthetic |
cardiovascular collapse acute cardiac infarction and postinfarction period (up to 6 month) severe bronchial asthma alcoholic or drug inebriation epinephron disease long-term intake of hormones anemia
acute respiratory disease pneumonia
clinically apparent thyrotoxicosis pancreatic diabetes epilepsy full stomach |
Sedation without depression – more frequent in common use.
Basal anaesthesia (preinduction) – when it is impossible to make a mark between premedication and induction to narcosis.
But, in any case, the benevolent conversation with a patient is desirable before the interference.
The primary objective of carrying out preoperative medication and sedation for the patients is to provide the most favorable conditions for a patient and a doctor during the operation. Therefore premedication provides the following effects: 1) it intensifies an effect, and 2) it prolongs the action of thelocal anaesthetics, 3) it reduces the side reactions of the cns and vital systems, 4) it provides possibility to reduce the concentration and dosage of local anaesthetics, 5) it prepares the main organs and systems of the patient for the operation by increasing their compensatory mechanism, keeping their activity at the level necessary to stabilize the vital functions. 6) It prevents the possibility of complications, related to the surgical interference.
The components of preoperative medication for the patients are conditioned by the basic mechanism of stress development, before, during and after the surgery, origin of the pain feeling and its action on vital systems, especially if the patient has concomitant diseases, for example the subcompensated forms or reacting to external irritants, which can provoke the parafunction.
Basic components of most charts of preoperative medication of patients are cholinolitic, central analgesic, sedative drugs, antihistaminic, atonics. And also adaptogens are useful. Atropin is administrated for the prophylaxis of hypersalivation, diminishing the bronchial secretion, prevention the reflexes of vagus (bradyarythmia and heart arrest) during the intubation of trachea. Analgesics (opioids or narcotics) block passing of pain impulse and removes feeling of pain at the level of opioid receptors in cns. Commonly morphine, fortral, tramalare used. They intensify analgesia without narcosis, have a strong action, but they don’t have anti-inflammatory activity and can provoke respiratory standstill and addiction. Antipyretics or nonsteroidresolvents (aspirin, meloxicame) mostly act on the injured tissues by inhibition of prostaglandin synthesis. Prostaglandins stimulate pain receptors and take part in inflammation development. Antipyretics also reduce the body temperature by influence on the temperature control centre in cns. Their action is insufficient (the pain less but does not disappear). Due to long-time administration it can cause clotting disorders, stomach ulcer, gastritis etc. Sedatives (ataractics) and tranquilizers have the purpose to calm down the patient, and prevent agitation, keep compensatory abilities of vital systems before surgery.
At the dental office, short-time acting agents in small doses are used because the patient should go outdoors or drive a car, and it is desirable for his relatives to escort him. At hospital more active and long-term tranquilizers are used. Antihistaminic preparations must decrease the negative influence
Of antigens from the area of operation, which have absorbed into the bloodstream and can entail postoperative allergic reactions. They also have moderate sedative action and partly strengthen the action of tranquilizers. Normally the preparations with sedative and h1 antagonistic action are used.
Before the urgent operation premedication is carried out by intravenous or hypodermal injections of preparations 10-40 min. Prior.
Before the scheduled operation in somatically healthy and compensated patients premedication is conducted 1 day prior the interference (first dose – at 10 pm in the eve of operation, second – 2 hours prior, third – 30-40 minutes prior the interference). In somatically sub- and decompensated patients symptomatic preparation has to begin 5-10 days prior the interference with the participation of contiguous specialists (for example, internists, haematologists). It is conducted until the improvement of the patient’s state and possibility of leadthrough of operation. And after the surgery the postmedication is carried out for the sake of reducing the risk of complications and cutting down the acute postoperative period.
At out-patient’s clinic preparations of short-time activity are usually applied, taking into account the type and short time of duration of operation and necessity to dismiss the patient home, but at hospital they are more long active.
Among the complications of the known charts of premedication there are such as: orthostatic collapses, allergic reactions to the applied medicines insufficient effect or remedy overdose. Orthostatic collapse is a serious
Complication, and it arises up when a patient suddenly zooms (from the operating table, bed, transport) from the horizontal position into vertical. The cardiovascular system is being in the state of slow speed of compensatory reactions, does not have time to change (to promote) tone of the myocardium and blood vessels, promote a pulse and arterial pressure, as a result, a sudden increase of loading on these structures leads to diminishing of their function: circulation effectiveness, hypovolemia of cerebral vessels, cerebral hypoxia and as a result the loss of consciousness and severe malfunction of the nervous regulation of all organs and systems. The first aid in such a case is to put the patient into the horizontal position and carry out the intensive care, or even resuscitation.
The allergic reactions to the applied medicines can develop on any of them, within different periods after their application. In case when the several medicines are applied stage-by-stage, it is more difficult to diagnost and find out, which of them caused the allergic reaction. Treatment of such a state with the known methods requires additional attention to the clinical features and subsequent searching of causal allergen.
If the allergic reaction happened before the planned interference, then the operation will be cancelled in the condition of slow normalization of the state of the patient, if during interference – help will be given to the patient and operation will be finished as quick as possible, and if before urgent interference – the operation will be conducted after normalization of vital systems activity and removal of risk for life.
The insufficient effect of premedication can show up variously, depending on that, whatever component of the pain feeling was not diminished by the medicinal influencing. As a rule, clinically it shows up by feeling of pain, presence of psychic excitation, fear, rejection of interference, active counteraction to the doctor. In such a case it is necessary to apply proper medicines, however, it is needed to remember, that during psychic excitation action of these medications in classic doses will be disfigured, and it is easy to get undesirable clinical effects, which can be dangerous for patient’s life. Taking it into account, it is expedient to decrease a volume or to halt interference (if there is such a possibility), whether to call an anaesthetist and with his participation conduct the operation. After the surgery a patient needs careful supervision during all the period of convalescence, especially at the presence of dangerous concomitant diseases, which can become acute as a result of the psychical and physical trauma.
Overdose of the used preparation (preparations) – clinically shows up depending on pharmacological action of this preparation manifested with unconsciousness, circulation and breathing disorders and so on. Diagnostics and treatment of such disorders need prompt assistance of anaesthetists, toxicologists, internists at the appropriate units at hospitals under the control of activity of vital systems, application of antagonists to medicines, which have been used.
A neuroleptanalgesia (nla) is the variety of general anaesthesia, when for achievement of medical effect neuroleptic (aminazine or haloperidol) and analgesic (strong opioid of short action – for example, phentanyl) are used together. Consciousness is remained, but neuroleptic considerably increases anaesthetizing, which is caused by analgesic. Therefore, a neuroleptanalgesia (nla) is the state of neurolepsy and analgesia, which is achieved by application of two main preparations of neuroleptic droperidol and narcotic phentanyl. For the phenomenon of their combined action a new term “autonomous block” or “neurovisceraldefence” has been invented. Nla is used as an addition to the local anaesthesia, as a preoperative anesthetizing, and more frequently it is combined with an inhalation seminarcosis (nitrous oxide + oxygen) and myorelaxants. Then an anaesthesia triad (tetrade) provides: 1) sleep, 2) analgesia (or other opioid), 3) autonomous block, 4) myorelaxation. Such anaesthesia runs smoothly, hemodynamics is stable, the patient quickly awakes after the stopping of gas supply, a wound does not hurt (due to an opioid), there is no nausea and vomits (due to neuroleptic). Droperidol and phentanyl are more frequent used in correlation 2:1, and the combined preparation with these components has the name of thalamonal (in America – innovar). Preparations should be entered intravenously and slowly.
Combined anaesthesia is supposed for the use of a few preparations, not one (monoanaesthesia).
Ataralgesia is supposed for the use of ataractics (valium, sibazonum), which in large doses remove fear and put the patient into sleep. This two-component anaesthetizing (sedation with ataractic, anaesthetizing with opioid) is used, when myorelaxation is not needed. Combination of Diazepamum+phentanylum in large doses causes the protracted sleep (well after the protracted operations). For short-time operations at a dental office short action ataractic is used. Flumazenil is used for desedation.
Audioanaesthesia is used as an additional method of anaesthetizing by influence on an auditory analyzer by the sounds of music, “white” noise and other. It activates the auditory focus in the brain, diminishing the level of reception of painful irritant. It diverts patient’s attention to another more pleasant irritant and, as a result, reduces the pain. The influence on a visual analyzer by a television set, special glasses for creation of “virtual reality” pictures is used lately to demonstrate emotionally positive films for patients.
Anaesthesia with acupuncture is mainly the additional method of anaesthetizing. It is used for pricking classic points and points on face, auricle.
Electro-anaesthesia is conducted with facility, which generates the weak currents of sinewave, rectangular or three-cornered form, which influences the brain of the patient through electrodes on his head. The most anaesthetic effect is had by rectangular impulses at frequency 100–200 Hz. Action of electric current causes: 1) phenomena of parabiosis (according to the studies of n. E. Vvedensky), 2) general activating of the limbic system, that causes analgesia due to diminishing of ascending nociceptive influence on the brain, 3) activating of the endogenous opioid system of the cns. Since 1952 electro-anaesthesia is applied together with the medicinal influencing. Electro-anaesthesia foresees the use of the special equipment which provides flowing of electric current through cerebral structures by skilled-up medical personnel.
Transcutaneous electric neurostimulation is carried out by the electric neurostimulation facility and electrodes which impose on a skin and skip through them the managed electric current with necessary parameters, as a result local anaesthesia is achieved.
Hypnotic influencing with the purpose of anaesthetizing – must be conducted only by doctors who have necessary qualification. It can be possible for some patients who are inclined to the hypnosis.
Indications for general anaesthesia (narcosis) in dentistry and maxillofacial surgery:
- Individual intolerance to the local anaesthetics.
- Psychoemotional agitation, unwillingness of “presence” in the operation.
- Necessity of monitoring of vital functions.
- Carrying out of complex, traumatic and durative interventions.
There are such contraindications as: uncompensated heart disease, acute.
Infectious diseases, acute and uncompensated diseases of parenchymatous organs, uncompensated diabetes mellitus.
Preparation of the patient includes realization of some principles: thorough examination of the patient, premedication the day before anaesthesia, the patient should not eat for 2–4 hours before narcosis (to avoid regurgitation), the bladder must be empty, dentures, glasses and jewelry should be removed. All equipment and medications for carrying out narcosis and removing possible complications should be in enough quantity and function properly.
During the examination the possibility of typical intubation and its difficulties should be evaluated. For carrying out the typical intubation the head of the patient should throw back easily, neck should be flexible, mandible must move forward easily, tongue must be mobile, mouth opening and fauces should be wide.
Signs of the complex intubation are short and thick neck, “bird face” (brachygnathia) insufficient opening of the mouth, infiltration and low mobility of the root of tongue, cmall throat, narrowing of upper airways by a pathological process, dislocation of the tongue into gullet, side dislocation of the tissues of the mouth floor and throat and glottis, chronical inflammatory processes at nasopharynx and fauces, dislocation of the nasal septum (at nasal intubation), present chronical hypoxia, intoxication, severe condition of the patient, concomitant diseases accompanied by the reducing of compensatory abilities of the organism.
Local anaesthesia
Measures that can assist to achieve the elimination of painful sensations in the certain area without inhibition of patient’s conscience are called the local anaesthesia. It can be achieved by different ways: application to the skin or mucosa (10 % lidocaine spray, 20 % benzocaine, 1–2 % dicaine, 4 % tetracaine, etc.), Intratissue administration of anaesthetizing agents.
There are the following types of the local anaesthesia in clinical dental practice, such as:
- Physical (freeze).
- Topical (applicative).
- Infiltrative.
- Nerve block.
- Intrapulp.
- Intraligament.
- Intraosseous.
The topical method is carried out to anaesthetize the nasal mucosa in the maxillary sinus puncture and the site of injection. The majority of operations in the maxillofacial area and an oral cavity are carried out under injective anaesthesia. In oral surgery infiltrative anaesthesia and nerve block are used.
During infiltrative anaesthesia layered impregnation of the tissues with anesthetic occurs.
Nerve block or so called regional block is the method of local anaesthesia, when anaesthetizing agent blocks the nerve conduction at a distance from the operative area. Conductive anaesthesia is carried out at durational operations at the facial bones and soft tissues, in the operations on the mandible, when infiltration does not have effect (Table 10.2).
Table 10.2. The methods of nerve block in maxillofacial region
| Methods of nerve block (conduction anaesthesia) |
| At maxilla |
At mandible |
Central anaesthesia |
| еuberalinfraorbitalnasopalatine – palatine |
mandibular
torusal
mental |
at the round foramen;
subzygomaticopterigoid;
suprazygomaticopterygoid; tuberal;
orbital;
pterygopalatinal at the oval foramen subzygomaticopterigoidsuprazygomaticopterigoid submandibular |
Block (regional) anaesthesia is performed to prevent pain during tooth, root and neoplasm extraction, during major alveolar process operations, when treating for diffuse pyoinflammatory processes, jaw fractures, when, in the course of applying infiltration anaesthesia, there is a risk of infection spreading to the surrounding tissues and when infiltration anaesthesia proves ineffective. Applying of this kind of anaesthesia means blocking the nerve, supply to a part of the body, outlying the part being operated. Today, such method of anaesthesia is performed by specific instruments and solutions (Fig. 10.1).

Fig. 10.1. Syringe, one-shot needle and carpule with anaesthetic solution
Applying block anaesthesia involves using certain anatomic landmarks to deposit anaesthetics in order to block the nerve trunk. During maxillofacial operations anesthetic is deposited to the nerve where it passes or exits a bone canal. It can be done either from the mouth cavity (oral anaesthesia) or through the skin (extra oral anaesthesia).
Anaesthetization effect depends both on concentration of medication and the size of the contacting area. The target of anaesthetic action in nerve fibres is ranvier’s nodes. For the full blockage, it is necessary to form contact of at least three nodes with anaesthetic.
In the presence of enough convicted hypotheses, the phenomenon of the local anaesthesia is not quite studied. It is a difficult dynamic process, which is expressed by the reverse morphologic and functional changes of the nervous fibre under the action of pharmacological preparations which repress their conductivity and excitability.
Quite often anaesthetizing is conducted without taking into account the neurotic state of the patient and concomitant somatic pathology. From statistical data 84 % of the patients feel insuperable fear, fear of pain during the surgical intervention. A considerable part of parallel instances is made by persons with concomitant diseases. Thus the advantages of the combined methods of anaesthetizing are obvious.
By the acting duration local anaesthetics are divided to the long-time acting and the short time acting
By the chemical structure it is divided in two main groups:
- Etheric (cocaine, novocaine).
- Amid (lidocaine, articaine).
For the topical anaesthesia we use:
Cocaine is the anesthetic, which started the era of modern local anesthetization. But it’s very toxic and now is not used in dental practice.
Dicaine – white crystal powder, well soluble in water or alcohol. The solution is sterilized by boiling. It is a very active agent, which is used for the topical anaesthesia. There is applied 0.25–2 % Solution. The maximum dosage for the adults is 0.09 g (3 % 3 ml).
In dental surgery clinic novocaine, trimecaine, lidocaine, mepivacaine, articaine are mostly used for the injection anaesthesia.
Novocaine
For the local infiltration of the soft tissues 0.5 % Solution is used. On the alveolar process of the jaw 1–2 % solution is used. There are maximum dosages: 150 ml 0.5 %, 75–100 ml 1 % and 25–30 ml 2 %. Novocain is ineffective in inflammation processes.
Trimecaine
The anaesthetizing activity of trimecaine is 2.5–3 times less than novocain, and toxicity is 1.2–1.4 times less. In comparison with novocain, the acting duration of trimecaine is longer, and it is more efficient at the inflammation sites, keloid scars and granulation tissues. Unlike novocain, trimecaine is more tolerable by the patients. The anaphylactoid reactions occur rarely, but isotonic saline solution must be used for preparing the anaesthetizing solution.
Lidocaine hydrochloride (xilocaine, xicaine) is a strong anesthetizing agent. Its anesthetic activity is 2–3 times more than novocaine and toxicity is 1–2 times more as well.
Mepivacaine belongs to amid anaesthetics. It absorbs slowly but blood vessels dilatation does not occur. In overdose, there is the possibility of toxic reactions progression. The remedy is used in 2 % or 3 % solution for the in.
Filtration or nerve blockage. The maximum dose is 4.4 mg/kg. In overdose some patients develop euphoria, depression, bradycardia, arterial hypotension or speech, swallow and vision disorders.
Articaine (ultracaine d-s, ultracaine d-s forte) – local anesthetic, that belongs to amid group and is produced in 1.7 ml cartridges and 20 ml flasks as 4 % solution. It is less toxic than lidocaine and only 1.5 Times more toxic than novocaine. Anesthetizing activity of articaine is 5 times more than novocaine. Anesthetic has a high level of protein bindning and low level of fat solubility. That is basic for the choice to administer it for pregnant patients (less toxic for the fetus).
To increase the anesthetizing activity and acting duration of the local anaesthetics, it is recommended to add 0.1 % Solution of epinephrine hydrochloride (1 drop for 5 ml).
It is necessary to remember, that all anaesthetics with vasoconstrictive action are contraindicated in case of:
- Hypertension.
- Heart disease.
- Decompensated diabetes.
Local and general complications
Medical emergencies require prompt assessment and action. There may not be time for a detailed assessment but it is possible to buy time by using a basic protocol that simultaneously assesses and supports vital functions. Fortunately, serious medical emergencies in dental practice are not common, but that means that they are all the more likely to be alarming when they do occur. The ability to stay calm and manage the situation successfully depends on prior planning and rehearsal for such an event.
There are essential drugs and items of equipment that every dental practitioner should have available for use in an emergency. Some of these are based on providing simple and uncomplicated treatments while others necessitate providing early definitive treatment. Acute asthma and anaphylaxis are two examples of emergencies where simple first aid measures are inadequate and definitive treatment should be started by the dentist while waiting for the ambulance service to transfer the patient to an accident and emergency (A&E) department. This essential treatment is described as first-line treatment in the following protocols. Some drugs are available in preloaded syringes for fast preparation.
Syncope
Signs and symptoms: may be preceded by nausea and closing in of visual fields; pallor and sweating; heart rate below60 beats/min (bradycardia) during attack.
First line treatment including:
- Lay flat.
- Give oxygen.
- Expect prompt recovery.
The main causes of faint could be pain or anxiety.
Principles of treatment:
- Need to encourage oxygenated blood flow to brain as rapidly as possible.
- May need to block vagal activity with atropine and allow heart rate to increase.
Hyperventilation
Signs and symptoms: light-headed; tingling in the extremities; muscle spasm may lead to characteristic finger position (carpo-pedal spasm).
First line: reassure; ask patient to rebreathe from cupped hands or reservoir bag of inhalational sedation or general anesthetic apparatus.
Causes – anxiety
Principles of treatment: reduce anxiety; over-breathing has blown off carbon dioxide, resulting in brain blood vessel vasoconstriction. Return carbon dioxide levels in blood to normal.
Postural hypotension
Signs and symptoms: light-headed; dizzy; loss of consciousness on returning to upright or standing position from supine position.
Treatment:
- Lay the patient flat and give oxygen.
- Sit the patient up very slowly.
More likely to occur if the patient is taking beta-blockers which reduce the capacity to compensate for normal cardiovascular postural changes.
Principles of treatment: encourage oxygenated blood flow to brain.
Diabetic emergencies: hypoglycaemia
Signs and symptoms: shaking and trembling; sweating; hunger; headache and confusion.
- If the patient is conscious, give three sugar lumps or glucose and a little water or glucose oral gel; repeated if necessary in 10 minutes.
Cause: usually known diabetic; the patient may have taken medication as normal but not eaten before a dental visit.
The main principles of treatment is to return blood glucose level to normal by giving glucose or by converting the patient’s own glycogen to glucose by giving glucagon.
Further management:
- Transfer the patient to A&E.
- Give up to 50 ml 20 % glucose i.v. infusion followed by 0.9 % saline flush as the glucose damages the vein.
- Expect prompt recovery.
Grand mal epileptic seizure
Signs and symptoms: a sudden loss of consciousness associated with tonic phase in which there is sustained muscular contraction affecting all muscles, including respiratory and mastication; breathing may cease and the patient becomes cyanosed; the tongue may be bitten and incontinence occur; after about 30 seconds, a clonic phase supervenes, with violent jerking movements of the limbs and trunk.
First-line:
- Ensure the patient is not at risk of injury during the convulsions but do not attempt to restrain convulsive movements.
- Make no attempt to put anything in the mouth or between the teeth.
- After movements have subsided, place the patient in the recovery position and check the airway.
- The patient may be confused after: reassure and offer sympathy.
- After full recovery, send the patient home unless the seizure was atypical or prolonged or injury occurred.
Cause:
- Usually the patient is a known epileptic.
- Epilepsy may not be well controlled.
- Seizure may be initialed by anxiety or by flickering light tube.
Principles of treatment:
- Maintain oxygenated blood to brain.
- Protect from physical harm.
- Administer anticonvulsant.
- Further management.
Risk of brain damage is increased with length of attack; therefore, treatment should aim to terminate seizure as soon as possible.
If convulsive seizures continue for 15 minutes or longer or are repeated rapidly (status epileptics):
- transfer to A&E;
- remove dentures, insert nasopharyngeal airway;
- give oxygen;
- give 10–20 mg i.v. diazepam (2.5 mg/30 s) as Seduxen but beware of respiratory depression, or diazepam solution for rectal administration in hospital.
Acute asthma
Signs and symptoms: persistent shortness of breath poorly relieved by bronchodilators; restlessness and exhaustion; tachycardia greater than 110 beats/min and low peak expiratory flow; respirations may be so shallow in severe cases that wheezing is absent.
First-line:
- Excluded respiratory obstruction.
- Sit the patient up.
- Give oxygen.
- Salbutamol (Ventolin) via a nebuliser (2.5–5 mg of 1 mg/ml nebuliser solution) or via a large-volume spacer (two puffs of a metered dose inhaler 10–20 times: one put every 30 seconds up to 10 puffs for a child).
- Reassure and allow home if recovered.
Cause: exposure to antigen but precipitated by many factors including anxiety.
Principles of treatment: oxygenation; bronchodilatation.
Further management:
- If little response, transfer to A&E.
- Dexamethazonei.v.: adults 200 mg; child 100 mg.
- Add ipratropium 0.5 mg to nebulised salbutamol.
- Euphylline slow i.v. injection of 250 mg in 10 ml over at least 20 minutes: monitor or keep finger on pulse during injection.
Anaphylactic shock
Signs and symptoms:
- Paresthesia, flushing and swelling of face, especially eyelids and lips.
- Generalized urticaria, especially the hands and feet.
- Wheezing and difficulty in breathing.
- Rapid weak pulse.
These may develop over 15 to 30 minutes following the oral administration of a drug or rapidly over a few minutes or seconds following i.v. drug administration.
- Lay the patient flat and raise his feet.
- Give oxygen.
- Give 0.5 ml epinephrine (adrenaline) 1 mg/ml (1 in 1000) intramuscular – 0.25 ml for 6–12 years; – 0.12 ml (or 6 months to 6 years).
- Repeated every 10 min until improvement.
Principles of treatment
Requires prompt energetic treatment of:
- laryngealoedema;
- bronchospa cm;
- hypotension.
Further management:
- Transfer to A&V.
- Chlorphenamine (chlorpheniramine) 10 mg in 1 ml intramuscular or slow i.v. injection.
- Hydrocortisone sodium succinate 200 mg by slow i.v. injection: valuable as action persists after that of adrenaline has worn off.
- Fluids i.v. (colloids) infused rapidly if shock not responding quickly to adrenaline.
Stroke
Stroke results from either cerebral haemorrhage or cerebral ischacmia. Signs and symptoms:
- Confusion followed by signs and symptoms of focal brain damage.
- Hemiplegia or quadriplegia.
- Sensory loss.
- Dysphasia.
- Locked-in syndrome (aware, but unable to respond).
First line: reassure; transfer to A&E.
Principles of treatment:
Maintain and transfer for further investigation.
Angina pectoris and myocardial infarction
Angina results from a reduced coronary artery lumen diameter because of atheromatous plaques.
Myocardial infarction is usually the result of thrombosis in the coronary artery.
Signs and symptoms:
- Sudden onset of severe crushing pain across the front of the chest, which may radiate towards the shoulder and down the left arm or into the neck and jaw; pain from angina usually radiates down the left arm.
- Skin pale and clammy.
- Shallow respirations.
- Nausea.
- Weak pulse and hypotension.
- If the pain is not relieved by glyceryltrinitrate (GTN), then the cause is myocardial infarction rather than angina.
First-line:
Allow the patient to rest in a position that he feels most comfortable:
- In the presence of breathlessness this is likely to do the sitting position, whereas syncopal patients will want to lie flat.
- Often an intermediate position will be most appropriate.
Angina:
- Angina is relieved by rest and nitrates: glyceryltrinitrate spray 400 mg metered dose (sprayed on the oral mucosa or under the tongue and mouth, then closed).
- Give oxygen.
Allow home if attack is mild and the patient recovers rapidly Myocardial infarction if myocardial infarction is suspected:
- give oxygen;
- aspirin tablet 300 mg chewed Principles of treatment;
- pain control;
- vasodilatation of blood vessels to reduce load on the heart.
Further management for severe angina or myocardial infarction:
- Transfer to A&E.
- Diamorphine 5 mg (2.5 mg in older people) by slow i.v. injection (1 mg/min).
- Early thrombolytic therapy reduces mortality.
Cardiac arrest
Most cardiac arrests result from arrhythmias associated with acute myocardial infarction or chronic ischaemic heart disease.
The heart arrests in one of three rhythms:
- VF (ventricular fibrillation) or pulseless VT (ventricular tachycardia);
- asystole;
- PEA (pulseless electrical activity) or EMU (declromechanical dissociation);
- signs and symptoms: unconscious; no breathing; absent carotid pulse. Principles of treatment;
- circulation failure for 4 minutes, or less if the patient is already hypoxaemic, will lead to irreversible brain damage;
- institute early basic life support as holding procedure until early advanced life support is available.
Early basic life support for cardiac arrest
The following instructions are based on the UK Resuscitation Council guidelines for basic life support. The essential features are remembered by ABC: airway, breathing and circulation.
Risks to the rescuer:
- Before starting a resuscitation attempt, the rescuer must rapidly assess the risks: traffic, falling masonry, toxic fumes and other potential hazards relevant to the environment.
- Mucous membrane exposure to hepatitis B virus (HBVJ and human immunodeficiency virus (HIV) is less of a risk than needle stick exposure, strongly suggesting that the chance of infection from mouth-to-mouth ventilation is negligible. However, the US Centers for Disease Control and Prevention advises universal precautions.
Basic life support:
- Initial patient asses cment, airway maintenance, expired air ventilation and chest compression constitute basic life support (BLS) or cardiopulmonary resuscitation.
- BLS is a “holding operation” maintaining ventilation and circulation until treatment of the underlying cause can be instigated.
- BLS implies that no equipment is used. Where a simple airway or face mask is used, this is described as “basic life support with airway adjunct”.
Theory of chest compression:
- The “thoracic pump” theory proposes that chest compression, an increasing intrathoracic pressure, propels blood out of the thorax, forward flow occurring because veins at the thoracic inlet collapse while the arteries remain patent.
- Even when performed optimally, chest compressions do not achieve more than 30 % of the normal cerebral perfusion.
Basic airway management:
- Jaw thrust rather than chin lift is method of choice for the trauma victim (Fig. 10.2).

Fig. 10.2. The jaw thrust airway maneuver. Further management
- An oropharyngeal airway such as a Guedel or nasopharyngeal airway, may be used (Fig. 10.3).

Fig. 10.3. The oropharyngeal (Guedal) and nasopharyngeal airway. Insertion via the mouth (A) and nose (B)
- A face mask used for ventilation allows oxygen enrichment (Fig. 10.4). Sequence of actions:

Fig. 10.4. Pocket face mask
- Ensure safety of rescuer and victim (referred to below as he, for simplicity).
- Check whether casualty is responsive.
- If he responds by answering or moving:
- leave him in the position in which you find him (providing he is not in further danger), check his condition and get help if needed;
- reassess him regularly. If he does not respond;
- shout for help;
- open the airway by tilting the head and lifting the chin (Fig. 10.5).
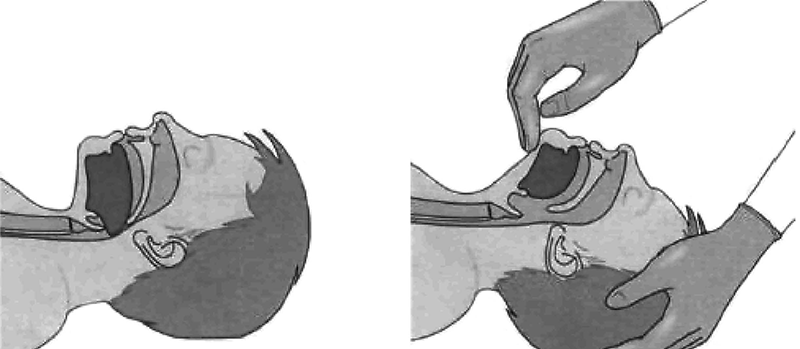
Fig. 10.5. Head tilt and chin lift airway manoeuvre
- Keeping the airway open; look, listen and feel for breathing.
- If he is breathing:
- turn him into the recovery position;
- check for continued breathing;
- send someone for help.
If he is not breathing:
- send someone for help or, if you are on your own, leave the victim and go for help;
- turn victim unto his back;
- remove visible obstruction from the victim’s mouth;
- give 2 breaths.
- Assess the victim for signs of a circulation:
- check the carotid pulse;
- take no more than 10 seconds to do this.
- If you are confident that you can detect signs of a circulation:
- continue rescue breathing;
- check circulation about every minute;
- if the victim starts to breathe on his own but remains unconscious, turn him into the recovery position.
If (there are no signs of a circulation or you are at all unsure:
- start chest compression (Fig. 10.6);
- combine rescue breathing and compression in the ratio of 2:15.
Continue until successful, help arrives, you become exhausted.
Fig. 10.6. Chest compressions: shown from above (A) and in cross-section (B)
Going for assistance:
- A lone rescuer will have to decide whether to start resuscitation or go for help first. If the cause of unconsciousness is likely to be trauma, drowning, or if the victim is an infant or a child, the rescuer should perform resuscitation for about 1 minute before going for help.
- If the victim is an adult and the cause of unconsciousness is not trauma or drowning, the rescuer should assume that the victim has a heart problem and go for help immediately it has been established that the victim is not breathing.
- Transfer to A&E.
- Advanced life support.
Advanced life support for cardiac arrest, advanced airway management techniques and specific treatment of the underlying cause of cardiac arrest constitute advanced life support (ALS).
Advanced airway management:
- A self-inflating bag and mask with attached oxygen permits ventilation with around 45 % oxygen. However, it is preferable also to use a reservoir as oxygen can then be provided at around 90 % (Fig. 10.7).
- The laryngeal mask airways (LMA), which seals around the larynx, is becoming popular as it provides more effective ventilation with a bag – valve system than with a face mask.
- The “gold standard” of airway management is endotracheal intubation as it protects against contamination by regurgitated gastric contents and blood, allows suctioning of the respiratory tract and drugs can be administered by this route. However, its use requires considerable training.
- A surgical airway intervention such as a needle cricothyroidotomy may be necessary if it is not possible to ventilate with bag-valve-mask or to intubate. This may be because of maxillofacial trauma or laryngeal obstruction.

Fig. 10.7. Self-inflating bag and mask with reservoir
High-pressure oxygen is given via a cannula inserted into the trachea, although this is only a temporary measure lasting about 40 minutes until a theatre is prepared for formal tracheostomy.
Specific treatment. Specific treatment algorithms (guidelines) are followed according to the electrocardiogram rhythm assessment and the clinical context. These are based on best scientific evidence.
Treatment is directed toward correcting underlying causes, use of specific drugs and defibrillation.
Defibrillation
Defibrillation is indicated in ventricular fibrillation and pulseless ventricular tachycardia, which arc the commonest arrhythmias causing cardiac arrest and the most treatable. However, the chances of successful defibrillation decline by about 5 % with each minute; therefore early management is vital (Fig.10.8):
- Defibrillation depolarizes most or all of the cardiac muscle simultaneously, allowing the natural pacemaking tissues to resume control of the heart.
- All defibrillators have two features in common: a power source capable of providing direct current, and a capacitor, which can be charged to a predetermined level and subsequently discharged through two electrodes placed on the casualty’s chest.
- Defibrillators may be manual (the operator interprets the rhythm and decides if a shock is necessary), semi-automatic (when the tasks of recognizing the arrhythmia and preparing for defibrillation are automated) or fully automatic.

Fig. 10.8. Defibrillation technique
Chapter 11. Exodontia
Indications and contraindications for teeth extraction
While the great majority of extractions can be safely done in the dental office, some patients require hospitalization for this surgery because of systemic conditions which make them poor surgical risks. Teeth may require removal for many reasons including the following:
I. General indications (morbid conditions caused by decayed teeth as a source of infection): odontogenouschroniosepsis and chronic odontogenous intoxication, odontogenousdisease of any organ (in the background of chroniosepsis).
II. Local indications is divided into 6 groups:
Sanation; Functional; Prosthetic; Orthodontic; Esthetic; Combination of above mentioned.
- Sanation:
- Chronic granulating or granulomatous periodontitis in case of curved or obstructed root canals.
- Acute purulent periodontitis, if there is no possibility to evacuate pus through root canal.
- Acute odontogenous osteomyelitis.
- Presence of pathological process around semi-impacted tooth (retromolar periostitis).
- Decidui teeth, in presence of inflammatory process.
- Decidui teeth, which cause acute septic conditions.
- Functional – indications which concerns cases of injury of soft tissues by impacted or semi-impacted tooth (buccal mucosa, pterygomandibular fossa); supernumerary teeth; in case of birth with erupted teeth, and there is no possibility to cover it with a protective plate.
- Prosthetic including the following:
Single teeth, which compromises denture stability; “gangrenous” roots, which cannot be filled and used as support for denture; teeth extended from dentition (Godon – Popov phenomena), which interferes with forming of occlusal arch significantly decayed permanent 1st molars in children (making room for correct eruption of 7 and 8 teeth).
- Orthodontic: 4th permanent teeth, which interferes orthodontic moving of anterior teeth; teeth extraction in case of space deficiency in orthodontic treatment.
- Esthetic: supernumerary teeth, malposed and teratic teeth; teeth, that spoil appearance, especially while smiling
- Combination of local indications
Complications associated with treatment of teeth (perforation of the tooth cavity floor, root); impacted teeth in uneffective orthodontic treatment; diseases or conditions when it is impossible to perform tooth treatment; the patient insists on tooth extraction.
Contraindications for teeth extraction
There are no absolute contraindications for tooth extraction but there are some diseases and conditions which require operation suspending or, if possible, preoperative medication.
Relative contraindications:
- Heart disease (Angina, arythmia, reumatism, endocarditis in acute course, heart failure).
- Kidney disease (acute glomerulonephritis, renal failure).
- Infectious diseases (diphtheria, hepatitis)
- Blood disease (haemophilia, leukosis, trombocytopenia).
- CNS diseases (meningitis, encephalitis).
- Mental diseases in acute condition (epilepsy, schizophrenia).
- Teeth placed in malignant tumor or hemangioma.
- Acute diseases of the respiratory tract (ARD, flu, bronchitis)
- Pregnancy.
Treatment planning
The information from the history and examination is used to formulate the best plan for the patient. This will include measures for adequate preparation for the procedure and also the selection of anaesthesia: whether local anaesthesia, conscious sedation with local anaesthesia or general anaesthesia. Anticipated difficulties are better discussed with the patient before treatment rather than during treatment, when they may be perceived as excuses for inadequate planning or experience.
Presurgical assessment of the patient includes evaluation of the level of anxiety, determination of health status and any necessary modifications of routine procedures, evaluation of the clinical presentation of the tooth to be removed, and radiographic evaluation of the tooth root and bone. All four of these major factors must be weighed when estimating the difficulty of the extraction. If any factor or combination of factors presents a level of difficulty that seems too great, the dentist should refer the patient to an oral and maxillofacial surgeon.
Instruments for teeth extraction, preparation of patient patient and surgeon preparation
Surgeons must prevent inadvertent injury or transmission of infection to their patients or to themselves. The concept of universal precautions states that all patients must be viewed as having blood-borne diseases that can be transmitted to the surgical team. To prevent this transmission, surgical gloves, surgical mask, and eyewear with side shields are required.
Additionally most authorities recommend that the surgical team wear longsleeved gowns that can be changed when they become visibly soiled.
Surgeon has to use protective eyeglasses, mask, and gloves. Surgeons should have short or pinned-back hair and should wear long-sleeved smocks that are changed daily or sooner if they become soiled. The patient should have full, waterproof drape. If the surgeon has long hair, it is essential that the hair be held in position with barrettes or other holding devices or be covered with a surgical cap. It is a major breach in aseptic technique to allow the surgeon’s hair to hang over the patient’s face and mouth. Before the patient undergoes the surgical procedure, a minimal amount of draping is necessary. A sterile drape should be put across the patient’s chest to decrease the risk of contamination.
Before the extraction, patients should vigorously rinse their mouths with an antiseptic mouth rinse, such as chlorhexidine 0.5 mg. This reduces the gross bacterial contamination in the patient’s mouth, which helps to reduce the incidence of postoperative infection.
To prevent teeth or fragments of teeth from falling into the mouth and potentially being swallowed or aspirated into the lungs, many surgeons prefer to place the 5 × 5 cm gauze loosely into the back of the mouth. This oral partition serves as a barrier so that, should a tooth slip from the forceps or shatter under the pressure of the forceps, it will be caught in the gauze rather than be swallowed or aspirated. The surgeon must take care that the gauze is not positioned so far posterior that it makes the patient gag. The surgeon should explain the purpose of the partition to gain the patient’s acceptance and cooperation for allowing the gauze to be placed.
Tooth extraction technique
To extract a tooth from the alveolus, periodontal attachment must be disrupted and the bony dental socket enlarged to allow withdrawal of the tooth. To achieve this, various instruments have been developed, extraction techniques described and some basic principles and guidance required when learning:
- Proper position of the patient in a chair.
- Elevation of circular ligament.
- Applying the forceps on a tooth.
- Advancing the forceps to enamel-cement line (in normal conditions it is marked by alveolar ridge).
- Closing up (fixing) the forceps with whole hand.
- Loosening of a tooth.
- Pulling a tooth out from socket.
Principles of tooth extraction:
- Beaks should be applied only on vestibular and oral surfaces of a tooth.
- Long axis of beaks should match with axis of a tooth.
- Avoid applying beak tips on an alveolar ridge and therefore subperiostal socket ridge resection.
Instrumental extraction
To extract a tooth from the alveolus, the periodontal attachment must be disrupted and the bony dental socket enlarged to allow withdrawal of the tooth.
To achieve this, various instruments have been developed:
- elevators: curved chisel-shaped instruments that fit the curvature of tooth roots; an elevator has a single blade;
- luxators: similar to elevators but finer blade;
- forceps: have paired blades that are hinged to permit the root to be grasped;
- peritome: has a finer blade with which to sever the periodontal attachment and is preferred where it is important not to damage the bony support of the tooth, for example when immediately replacing a tooth with a dental implant.
The design of forceps has remained remarkably constant over many years: it is difficult to improve on the basic shapes. All forceps consist of two blades and handles joined at a hinge. The inner aspects of the blades are concave to fit the root accurately; they should not touch the crown of the tooth. The blades have sharp edges to cut periodontal ligament fibres and are wedge-shaped to dilate the socket. The blades are applied to the buccal and lingual aspects of the root. There are many designs, but for the purpose of this guide we will restrict discussion to those most commonly used.
Forceps for upper teeth
Forceps for extracting upper anterior teeth are of a simple design (Fig. 11.1). The handles are straight and 12–14 cm long, joined at a hinge to the beaks, which are 2–3 cm long. The handles are contoured on their outer surface to allow a good grip. The beaks are both concave on their inner aspect, shaped to fit around the root of the tooth as closely as possible (Fig. 11.2) when the forceps are applied in the long axis of the tooth. The beaks are applied labially and palatally. All extraction forceps can be seen as modifications of this basic design.
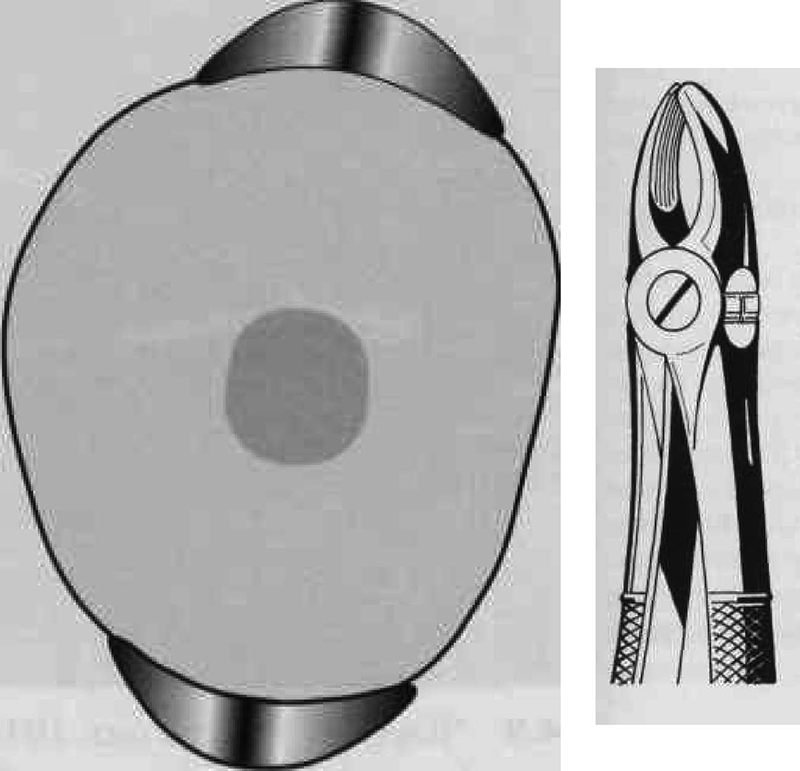
Fig. 11.1. Forceps for extracting upper anterior teeth
Fig. 11.2. Poorly fitting Forcep blades concentrate force at the point of contact
Fit of the beaks of upper straights around a tooth root. If the blades fit closely around the root, the load will be evenly distributed (left). If there is a poor fit, the load will be concentrated at the points of contact (right).
These forceps can be applied to the long axis of anterior teeth, gaining access by the patient opening their mouth fairly widely (Fig. 11.3). However, if one were to attempt to use these forceps on an upper first premolar, there is a risk of traumatizing the lower lip. Forceps for use in the upper jaw further back than the canine have a curve in the beak (Fig. 11.4), which keeps them above the lip when they are in the long axis of the tooth. The beaks of these forceps are also concave on their inner aspect to fit the root of upper premolars.

Fig. 11.3. Application of upper straight forceps to an incisor

Fig. 11.4. Application of upper premolar forceps. Note the curve in the beak
These forceps could be used to extract posterior teeth, but for teeth with multiple roots, forceps are available with beaks specifically designed to fit complex root forms (Fig. 11.5). In principle, the more closely the beaks are adapted to the roots, the more widely the forces of extraction are distributed and the lower the likelihood of tooth fracture.

Fig. 11.5. Beaks of upper left molar forceps (left and right)
The buccal beak has a point to fit into the bifurcation, with concavities on either side to fit around the buccal roots and a broader concave palatal beak. Because of this distinction between buccal and palatal beaks, there must be separate designs for left and
For alI upper extractions it is necessary to push firmly in the long axis of the tooth during extraction. For this reason many forceps for upper posterior teeth have a curve at the end of the handle so that they fit in the palm of the hand (Fig. 11.6).
Access for extraction of teeth far back in the mouth can be difficult. A further variation involves a step in the beaks of the forceps (Fig. 11.7), which enables us to put the beaks on the upper third molar whilst avoiding the lower lip.

Fig. 11.6. Upper premolar forceps. Note the curve in the “Read pattern” handles

Fig. 11.7. “Bayonet” forceps for upper third molars
Forceps for lower teeth
If you were to attempt to apply upper anterior forceps to the lower anterior teeth you would have difficulty in getting past the nose and upper alveolus. It is usual to overcome the problem by using forceps with a right-angled bend in them; this permits the handles to come straight out of the mouth when the beaks are in the long axis of the tooth (Fig. 11.8). The beaks of these simple forceps are similar to those used on upper anterior teeth. Such forceps can be used effectively on all lower teeth, from second premolar to second premolar.

Fig. 11.8. Forceps for lower canine, premolars and incisors
Just as with the forceps for upper teeth, beak design has been modified for multiple-rooted teeth. Full molar forceps have a point and two adjacent concave facets on both buccal and lingual beaks (Fig. 11.9).

Fig. 11.9. Beaks of the lower molar forceps
There are special forceps for removal of lower wisdom teeth or third molars (Fig. 11.10). These forceps also have points on both beaks, but they bent on a plane, as against other lower forceps bent on an edge. In case of need we can use these tools for exodontia of all lower molars when patient has a trismus or insufficient opening of a mouth.

Fig. 11.10. Forceps for wisdom lower molar bent on a plane
Smaller versions of forceps are available for use on deciduous teeth, which some operators like to use to access lower third molars where vertical space is at a premium. There were several different forceps extraction techniques described and so some basic principles and guidance are required when learning. Forceps are used to disrupt the periodontal attachment and dilate the bony socket either directly, by forcing the blades between tooth and bone, or by moving the tooth root within the socket, or both. Once this has been done, the tooth may be lifted from its socket. The movements that are required to complete the extraction may be described as a preliminary movement to sever the periodontal membrane and generally dilate the socket, followed by a second movement to complete the dilation and withdraw the tooth. The first movement requires that force is directed along the long axis of the tooth, pushing the blades of the forceps towards the oot apex. This force is then maintained during the second movement, which is dependent on the tooth root and bone morphology. If a tooth has a single round root, then it may be rotated. Where the buccal bone plate is relatively thin, it may be possible to distort it significantly by moving the forceps applied to the tooth root in a buccal direction.
The second movement depends on the tooth and may be described as:
- upper incisors and canines: rotational;
- upper premolars: limited buccal and palatal;
- upper molars: buccal;
- lower incisors and canines: buccal;
- lower premolars: rotational;
- lower molars: buccal.
Elevators may be used to carry out the first movement prior to completion of the extraction with forceps. Elevators are used to sever the periodontal membrane and dilate the socket; the tooth is then removed. Sometimes teeth and roots may be removed with elevators alone. There are many different designs of elevator (Fig. 11.11).

Fig. 11.11. Dental elevators
It is important that elevators are used appropriately, with their blades between root and bone rather than between adjacent teeth, or else both teeth will be loosened.
There are many designs of forceps. The blades vary in size and shape according to the root morphology of the tooth/teeth for which they
For example, lower molar forceps incorporate a right angle between blades and handles, while the blades each have a central projection to accommodate the bifurcation. Upper “root” forceps have narrower blades than the equivalent upper premolar forceps. It may be difficult to apply forceps to teeth that are outside of a crowded dental arch and elevators may be more appropriate for initiating the extraction or for the whole procedure. The applied force should be controlled and limited when using both elevators and forceps so that the soft tissues are not accidentally injured or the jaws fractured. Only with experience it is possible to know that the usual force is not producing the expected result, when further investigation is required with a radiograph (if not already available) or a transalveolar approach required.
The non-dominant hand is used to support the mandible against the force of the first movement when extracting lower teeth. It is also used to retract the intraoral soft tissues and, by supporting the adjacent alveolus, provide feedback of movement as a measure of control. The patient should have eye protection; if the treatment is carried out under local anaesthesia, then the patient may be placed in a position between sitting up and supine or treated supine. Treatment under conscious sedation or general anaesthesia will dictate the supine position. Lower right quadrant extractions are best performed with the operator standing behind the patient; for all other extractions, the operator should stand in front of the patient.
Atypical (surgical) extraction
Atypical (surgical) tooth extraction – method of exodontias, which is performed with chisel and bur (Fig. 11.12). It’s indicated when tooth or root extraction cannot be performed with dental forceps or elevators only. This method most frequently is used to extract third lower molar. The surgical approach and direction of the incision depends on tooth or root position. Access to the tooth is achieved by forming and raising a mucoperiosteal flap. Then using bur and chisel remove portions of the bone that covers the tooth. Exposed tooth can be removed. Sharp bone edges should be smoothed, the flap is returned on place.

Fig. 11.12. Impacted wisdom tooth
The surgical (atypical) teeth extraction including next stages: raising a flap (Fig. 11.13), removal of bone, tooth division, removal of tooth / tooth fragments (Fig. 11.14), primary closure.

Fig. 11.13. Raising a flap

Fig. 11.14. Removal of bone, tooth division, removal of tooth / tooth fragments
A typical instruction leaflet given to patients after an extraction
On the day of treatment:
- Do not rinse your mouth for at least 24 hours.
- Avoid hot fluids, alcohol, hard or chewy foods.
- Choose cool drinks and soft foods.
- Avoid vigorous exercise.
- Smokers should avoid smoking.
- Should the wound start to bleed, apply a small compress.
This can be made of some cotton wool in a clean handkerchief. Place this on the bleeding point and bite firmly on it for 5–10 minutes or longer if necessary:
- If you cannot stop the bleeding yourself, please seek professional advice.
- Any pain or soreness can be relieved by taking the prescribed medication. If none was prescribed, take tablets such as paracetamol (Panadol) 2 tablets every 4 hours as required. Do not take more than the recommended number per day.
Starting 24 hours later
A typical instruction leaflet given to patients after an extraction:
- gently rinse the wound with hot saltwater mouth rinses (or other rinse as recommended) for a few days. This should be carried out three times a day after each meal.
Complications of tooth extraction
A complication is any event that would not normally occur and which might increase the patient’s suffering. The range of potential complications is vast. It includes adverse events occurring locally, nearby or at distant sites, some things that occur immediately and others that occur a little later or are greatly delayed, some are rare and some frequent, some are serious and some inconsequential. There is considerable variation in the degree to which complications are predictable or preventable. The implications of adverse events are also determined in part by the patient’s expectations, the reason for surgery and the manner in which the event is managed once it is recognized.
In Table 11.1 there is an illustrative list of some typical complications of tooth extraction, divided according to the time and site of occurrence.
Table 11.1. Complications of tooth extraction
| |
Local |
Regional / distant |
| Immediate |
Fractured crown, root, alveolus, tuberosity, mandible, adjacent tooth |
Crushed or burnt lip; injury to inferior dental or lingual nerves; lacerated tongue or palate |
| Tear of gingiva, alveolar mucosa |
Swallowed or inhaled instrument or tooth |
| Oroantral communication |
Injury to Temporomandibular Joint |
| Fractured instrument |
|
| Injury of regional nerves |
|
| Delayed |
Dry socket; local infection |
Spreading infection |
| Delayed or secondary hemorrhage |
Myofascial pain |
| Osteonecrosis |
Hematoma |
| Late |
Alveolar atrophy |
Osteomyelitis; actinomycosis |
Some complications are sufficiently common and amenable to treatment to justify further description.
It is axiomatic that the best and easiest way to manage a complication is to prevent it from happening. Prevention (of surgical complications is best accomplished by a thorough preoperative assessment and comprehensive treatment plan. Only when these are routinely performed can the surgeon expect to have minimal complications. It is important to realize that even with such planning, complications occasionally occur. In situations in which the dentist has planned carefully, the complication is often expected and can be managed in a routine manner.
For example, when extracting a maxillary first premolar, which has long thin roots, it is far easier to remove the buccal root than the palatal root. Therefore the surgeon uses more force toward the buccal root than toward the palatal root. If a root does fracture, it is then the buccal root rather than the palatal root, and the subsequent retrieval is easier.
Surgeons must perform surgery that is within their own ability. Surgeons must therefore carefully evaluate their training and ability before deciding to perform a specific surgical task. It is inappropriate for a dentist with limited experience in the management of impacted third molars to undertake the surgical extraction of a deeply embedded tooth.
The incidence of operative and postoperative complications is unacceptably high in this situation. Surgeons must be cautious of unwarranted optimism, which clouds their judgment and prevents them from delivering the best possible care to the patient. The dentist must keep in mind that referral to a specialist is an option that should always be exercised if the planned surgery is beyond the dentist’s own skill level. In some situations this is not only a moral obligation but also a medicolegal responsibility.
In planning a surgical procedure, the first step is always a thorough review of the patient’s medical history. Several of the complications are caused by inadequate attention to medical histories that would have revealed the presence of a complicating factor. Patients with compromised physical status will have local surgical complications that could have been prevented had the surgeon taken a more thorough medical history.
One of the primary ways to prevent complications is by taking adequate radiographs and reviewing them carefully. The radiograph must include the entire area of surgery, including the apices of the roots of the teeth to be extracted and the local and regional anatomic structures, such as the maxillary sinus and the inferior alveolar canal. The surgeon must look for the presence of abnormal tooth root morphology. After careful examination of the radiographs, the surgeon must occasionally alter the treatment plan to prevent the complications that might be anticipated with a routine forceps (closed) extraction. Instead, the surgeon should consider surgical approaches to removing teeth in such cases.
After an adequate medical history has been taken and the radiographs have been analyzed, the surgeon must do the preoperative planning. This is not simply a preparation of a detailed surgical plan but is also a plan for managing patient anxiety and pain and postoperative recovery (instructions and modifications of normal activity for the patient). Thorough preoperative instructions and explanations for the patient are essential in preventing the majority of complications that occur in the postoperative period. If the instructions are not thoroughly explained or their importance made clear, the patient is less likely to follow them.
Finally, to keep complications at a minimum, the surgeon must always follow the basic surgical principles. There should always be clear visualization and access to the operative field, which requires adequate light, adequate soft tissue reflection (including lips, cheeks, tongue, and soft tissue flaps), and adequate suction. The teeth to be removed must have an unimpeded pathway for removal. Occasionally, bone must be removed and teeth must be sectioned to achieve this goal. Controlled force is of paramount importance; this means “finesse,” not “force.” The surgeon must follow the principles of asepsis, atraumatic handling of tissues, hemostasis, and thorough debridement of the wound after the surgical procedure.
Violation of these principles leads to an increased incidence and severity of surgical complications.
Injuries to the soft tissue of the oral cavity are almost always the result of the surgeon’s lack of adequate attention to the delicate nature of the mucosa and the use of excessive and uncontrolled force. The surgeon must pay careful attention to the soft tissue while working primarily on the bone and tooth structure, develop adequate-sized flaps and use minimal force for retraction of the soft tissue.
The second soft tissue injury that occurs with some frequency is inadvertent puncturing of the soft tissue. Instruments, such as a straight elevator or periosteal elevator, may slip from the surgical field and puncture or tear into the adjacent soft tissue.
Once again, this injury is the result of using uncontrolled force instead of finesse and is best prevented by the use of controlled force, with special attention given to the supporting fingers or support from the opposite hand in anticipation of slippage. If the instrument slips from the tooth or bone, the fingers thus catch the hand before injury occurs. When a puncture wound does occur, the treatment is aimed primarily at preventing infection and allowing healing to occur, usually by secondary intention. If the wound bleeds excessively, it should be controlled by direct pressure on the soft tissue. Once hemostasis is achieved, the wound is usually left open and not sutured, so that if a small infection were to occur, there would be an adequate pathway for drainage.
Abrasions or burns of the lips and corners of the mouth are usually the result of the rotating shank of the bur rubbing on the soft tissue. When the surgeon is focused on the cutting end of the bur, the assistant should be aware of the location of the shank of the bur in relation to the cheeks and lips. If such an abrasion does develop, the dentist should advise the patient to keep it covered with Vaseline or an antibiotic ointment. It is important that the patient keeps the ointment only on the abraded area and not spread onto intact skin, because it is quite likely to result in a rash. These abrasions usually take 5 to 10 days to heal. The patient should keep the area moist with the ointment during the entire healing period to prevent eschar formation, scarring, and delayed healing, as well as to keep the area reasonably comfortable.
The most common complication associated with the tooth being extracted is fracture of its roots. Long, curved, divergent roots that lie in dense bone are most likely to be fractured. The main method of preventing fracture of roots is to perform an open extraction technique and to remove bone to decrease the amount of force necessary to remove the tooth.
Extraction of wrong teeth
A complication that every dentist believes can never happen – but happens surprisingly often is extraction of the wrong tooth. This should never occur if appropriate attention is given to the planning and execution of the surgical procedure.
This problem may be the result of inadequate attention to the preoperative assessment. If the tooth to be extracted is grossly carious, it is less likely that the wrong tooth will be removed. The wrong tooth is most commonly extracted when the dentist is asked to remove teeth for orthodontic purposes, especially from patients who are in mixed dentition stages and whose orthodontists have asked for unusual extractions. Careful preoperative planning and clinical assessment of which tooth is to be removed before the forceps is applied is the main method of preventing this complication.
Fractured alveolus
Most extractions result in delivery of the tooth, intact, with no other tissue apart from some periodontal ligament. However, bone can fracture in a number of circumstances. A small piece of buccal plate of bone is sometimes removed with the tooth. Provided that it is small, and that the mucosa is not torn in removing it, this is of little consequence. Sharp edges of bone beneath mucosa may need to be smoothed.
A maxillary molar standing alone, or associated with a large maxillary antrum, is particularly prone to fracture of the tuberosity. The tuberosity is also vulnerable to a fully erupted maxillary third molar being elevated backwards (see comments about effects of large elevators). In such circumstances, if the bone fragment is small and the antrum will not be left exposed, it may be best to dissect the bone out with the tooth then close the wound. For large fragments, however, the extraction should be abandoned and the fractured piece should be splinted (other temporary means of pain control may be required) and the tooth surgically removed about 4 weeks later, once the bone has healed.
Fractures may also occur if an instrument is forced between teeth or between roots that do not displace out of their sockets, or if undue force is used in any extraction. It is difficult to measure exactly what constitutes excessive force other than by its adverse effects. However, it is very difficult for most dentists extracting most teeth to apply sufficient force in the correct direction to actually do damage. The human body is remarkably resistant to steadily applied force. It is important to be prepared to stop if it appears that reasonable force is not achieving the goal.
Fracture of maxillary tuberosity
Fracture of a large section of bone in the maxillary tuberosity area is a situation of special concern. The maxillary tuberosity is especially important for the construction of a stable retentive maxillary denture. If a large portion of this tuberosity is removed along with the maxillary tooth, denture stability may be compromised. The fracture of the maxillary tuberosity most commonly results from extraction of an erupted maxillary third molar or from a second molar if it happens to be the last tooth in the arch.
Injury to regional nerves
The branches of the fifth cranial nerve, which provide innervation to the mucosa and skin, are the structures most likely to be injured during extraction. The most frequently involved specific branches are the mental nerve, the lingual nerve, the buccal nerve, and the nasopalatine nerve. The nasopalatine and buccal nerves are frequently sectioned during the creation of flaps for removal of impacted teeth. The area of sensory innervation of these two nerves is relatively small, and reinnervation of the affected area usually occurs rapidly. Therefore the nasopalatine and long buccal nerves can be surgically sectioned without sequelae or complications.
Surgical removal of mandibular premolar roots or impacted mandibular premolars and periapical surgery in the area of the mental nerve and mental foramen must be performed with great care. If the mental nerve is injured, the patient will have an anesthesia or paresthesia of the lip and chin. If the injury is the result of flap reflection or simple manipulation, the altered sensation usually disappears in a few weeks to a few months. If the mental nerve is sectioned at its exit from the mental foramen or torn along its course, it is likely that mental nerve function will not return, and the patient will have a permanent state of anesthesia. If surgery is to be performed in the area of the mental nerve or the mental foramen, it is imperative that surgeons have a keen awareness of the potential morbidity from injury to this nerve. If surgeons have any question concerning their ability to perform the indicated surgical procedure, they should refer the patient to an oral and maxillofacial surgeon. If a three-corner flap is to be used in the area of the mental nerve, the vertical releasing incision must be placed far enough anterior to avoid severing any portion of the mental nerve. Rarely is it advisable to make the vertical releasing incision at the interdental papilla between the canine and first premolar.
The lingual nerve is anatomically located directly against the lingual aspect of the mandible in the retromolar pad region. The lingual nerve rarely regenerates if it is severely traumatized. Incisions made in the retromolar pad region of the mandible should be placed to avoid severing this nerve. Therefore incisions made for surgical exposure of impacted third molars or of bony areas in the posterior molar region should be made well to the buccal aspect of the mandible. Prevention of injury to the lingual nerve is of paramount importance for controlling this difficult complication.
Finally, the inferior alveolar nerve may be traumatized along the course of its intrabony canal. The most common place of injury is the area of the mandibular third molar. Removal of impacted third molars may crash or sharply injure the nerve in its canal. This complication is common enough during the extraction of third molars that it is important to inform patients on a routine basis that it is a possibility. The surgeon must then take every precaution possible to avoid injuring the nerve during the extraction.
Injury to temporomandibular joint
Another major structure that can be traumatized during an extraction procedure in the mandible is the temporomandibular joint (TMJ). Removal of mandibular molar teeth frequently requires the application of a substantial amount of force. If the jaw is inadequately supported during the extraction, the patient may experience pain in this region. Controlled force and adequate support of the jaw prevents this. The use of a bite block on the contralateral side may provide adequate balance of forces so that injury and pain do not occur. The surgeon must also support the jaw. If the patient complains of pain in the TMJ immediately after the extraction procedure, the surgeon should recommend the use of dry heat, rest for the jaw, a soft diet, and 1000 mg of aspirin every 4 hours for several days. Patients who cannot tolerate aspirin should be given an aspirin substitute, such as acetaminophen.
Oroantral communications
Removal of maxillary molars occasionally results in communication between the oral cavity and the maxillary sinus. If the maxillary sinus is large, if no bone exists between the roots of the teeth and the maxillary sinus, and if the roots of the tooth are widely divergent, then it is increasingly probable that a portion of the bony floor of the sinus will be removed with the tooth. If this complication occurs, appropriate measures are necessary to prevent a variety of sequelae. The two sequelae of most concern are postoperative maxillary sinusitis and formation of a chronic oroantral fistula. The probability that either of these two sequelae will occur is related to the size of the oroantral communication and the management of the exposure.
Diagnosis of the oroantral communication can be made in several ways. The first is to examine the tooth once it is removed. If a section of bone is adhered to the root ends of the tooth, the surgeon can be relatively certain that a communication between the sinus and mouth exists. If a small amount of bone or no bone adheres to the molars, a communication may exist anyway. To confirm the presence of a communication, the best technique is to use the nose-blowing test. Pinching the nostrils together occludes the patient’s nose, and the patient is asked to blow gently through the nose while the surgeon observes the area of the tooth extraction. If a communication exists, there will be passage of air through the tooth socket and bubbling of blood in the socket area.
After the diagnosis of oroantral communication has been established, the surgeon must determine the approximate size of the communication, be cause the treatment will depend on the size of the opening. If the communication is small (2 mm in diameter or less), no additional surgical treatment is necessary. The surgeon should take measures to ensure the formation of a high-quality blood clot in the socket and then advise the patient to take sinus precautions to prevent dislocation of the blood clot.
Sinus precautions are aimed at preventing increases or decreases in the maxillary sinus air pressure that would dislodge the clot. Patients should be advised to avoid blowing the nose, violent sneezing, sucking on straws, and smoking. Patients who smoke and who cannot stop (even temporarily) should be advised to smoke in small puffs, not in deep drags, to avoid pressure changes.
The surgeon must not probe through the socket into the sinus with a periapical curette or a root tip pick. It is possible that the bone of the sinus has been removed without perforation of the sinus lining. To probe the socket with an instrument might unnecessarily lacerate the membrane. Probing of the communication may also introduce foreign material, including bacteria, into the sinus and thereby further complicate the situation. Probing of the communication is therefore absolutely contraindicated.
If the opening between the mouth and sinus is of moderate size (2 to 6 mm), additional measures should be taken. To help ensure the maintenance of the blood clot in the area, a Figure-of-eight suture should be placed over the tooth socket. The patient should also be told to follow sinus precautions. Finally, the patient should be prescribed several medications to help lessen the possibility that maxillary sinusitis will occur. Antibiotics, usually amoxicillin or clindamycin, should be prescribed for 5 days. In addition, a decongestant nasal spray should be prescribed to shrink the nasal mucosa to keep the ostium of the sinus patent. As long as the ostium is patent and normal sinus drainage can occur, sinusitis and sinus infection are less likely. An oral decongestant is also sometimes recommended.
If the sinus opening is large (7 mm or larger), the dentist should consider closing the sinus communication with a flap procedure. This usually requires that the patient be referred to an oral and maxillofacial surgeon, because flap development and closure of a sinus opening are somewhat complex procedures that require skill and experience.
The most commonly used flap is a buccal flap. This technique mobilizes buccal soft tissue to cover the opening and provide for a primary closure. This technique should be performed as soon as possible, preferably on the same day in which the opening occurred. The same sinus precautions and medications are usually required.
Fractures of the mandible
Fracture of the mandible during extraction is a rare complication; it is associated almost exclusively with the surgical removal of impacted third molars. A mandibular fracture is usually the result of the application of a force exceeding that needed to remove a tooth and often occurs during the use of dental elevators. However, when lower third molars are deeply impacted, even small amounts of force may cause a fracture. Fractures may also occur during removal of impacted teeth from a severely atrophic mandible. Should such a fracture occur, it must be treated by the usual methods used for jaw fractures. The fracture must be adequately reduced and stabilized with intermaxillary fixation. Usually this means that the patient should be referred to an oral and maxillofacial surgeon for definitive care.
Dry socket (alveolar osteitis, alveolitissicca dolorosa, infected socket) occurs after about 3 % of routine extractions. It is recognized by pain at the site of extraction, often aching or throbbing in nature but remarkably constant in severity (including during the night), starting within a day or so of a tooth extraction. The pain is often resistant to common analgesics. Examination reveals a socket partly or totally devoid of blood clot with exposed, rough, painful bone. Grayish remnants of clot may be present. The surrounding mucosa and the whole alveolus may be red, swollen and tender. Inflammation spreads through the alveolus mesiodistally, resulting in tenderness of the adjacent teeth to pressure. Occasionally a patient will believe that the wrong tooth has been extracted because of the pain in the adjacent tooth. Be aware that misdiagnosis can occur. The mouth smells and tastes foul (a smell of anaerobic bacterial activity or rotting meat). There may be a local lymphadenitis, but severe systemic response in the form of fever is rare.
If no treatment were provided the condition would eventually resolve spontaneously, but it may take up to 4 weeks and during that time the pain would persist. Similar pain is experienced whenever an area of bone is left exposed in the mouth and usually settles when the exposed (and non-vital) bone is either eventually covered by granulation tissue or is separated from the underlying bone and sequestrated. A few untreated cases of dry socket may progress to infection that spreads through the bone marrow (osteomyelitis).
There is obviously a bacterial component to this condition. Its incidence may be reduced by the prophylactic administration of metronidazole, or by the irrigation of the gingival crevice with chlorhexidine before extraction. It should be noted, however, that routine prophylactic administration of antibiotics before extraction is not justified. There are similarities to acute ulcerative gingivitis in the high spring and autumn prevalence, frequency in smokers and possible relationship to female sex hormones. However, some aspects of the condition’s behavior are not so obviously infective in nature. The condition is most prevalent in patients in their fourth decade. It is more common after extractions of posterior and difficult teeth and seen more often in the lower jaw than the upper. Dry socket is more likely to occur after extractions under local anaesthesia than under general anaesthesia and is less frequent after multiple extractions. It is probable that the condition represents the outcome of a mixture of disease processes in which trauma, local fibrinolysis and bacterial clot degradation all play a part. Some patients are particularly prone to dry socket, without any other evident medical problem. Investigation need not be extensive; the condition can usually be diagnosed confidently on clinical grounds. A radiograph is valuable, both as a baseline against which to check bone change, should there not be a rapid resolution, and to assure the dentist and patient that no root has been left behind.
Treatment of the condition is primarily symptomatic. The socket should be irrigated with warm saline to remove the debris. A variety of antiseptic dressings is available to cover the exposed bone. A proprietary, eugenol-containing, soft, fibrous paste can be tucked into the coronal part of the socket to cover the bone. It can be left in situ and is usually shed spontaneously from the socket over a few days. Pain relief is usually very effective within hours. If relief is not achieved in a reasonable time, repeat irrigation and dressing of the wound is usually effective. Alternative dressings (each of which must be removed about a week later) include ribbon iodoform gauze and ointment on gauze (which may have lidocaine or tetracaine paste added to it).
Osteonecrosis of the jaw (ONJ)
It has become apparent since about 2002 that patients taking bisphosphonate drugs (such as zoledronate, alendronate and pamidronate), which reduce bone resorption, are at risk of developing osteonecrosis, particularly after tooth extraction (Fig. 11.15). The condition is recognized as failure to heal, exposure of dead bone and, often, associated infection. The condition persists with bone remaining exposed and failing to sequester for many months or years. Stopping use of the drug does not appear to make much difference to the outcome, probably because the half-life of the drugs, in the bone, is of the order of months to years. Tooth extraction should, if possible, be avoided in patients taking these drugs.

Fig. 11.15. Osteonecrosis of the jaw secondary to extraction of lower anterior teeth in a patient taking a bisphosphonate drug
Postextraction haemorrhage
After a routine extraction it is expected that bleeding will cease after no more than 10 minutes. If bleeding continues, the area should be inspected for signs of mucosal tearing or other evident cause for continued hemorrhage. In the absence of any such sign, a further period of 10 minutes with firm pressure on the wound should be tried. Every effort should be made to determine whether the bleeding is arising from mucosa or bone.
If tears in the mucosa are found they should be sutured. They can be remarkably difficult to find if they have occurred posteriorly, especially lingual to a lower third molar or posteriorly to a maxillary third molar. Suturing can be effectively performed with a variety of materials, but black wattled suture permits the knot to be precisely tensioned. If bleeding continues, the next action is to suture the mucosa over the socket, not in an attempt to approximate the mucosal edges but to pull the gingival margin tightly down onto the bone edge of the socket. This restricts the blood supply to the gingiva, from which the bleeding frequently originates. A suture taking bites of tissue from all four corners of the socket, pulled together as a Fig.ure of eight, works well (Fig. 11.16).

Fig. 11.16. A Fig.ure-of-eight stitch is usually performed to help maintain piece of haemostatic agent in tooth socket
If suturing alone is not successful, a resorbable haemostatic agent (e.g. oxidized cellulose, fibrin foam, gelatin foam, collagen granules, alginate fibres) is placed in the socket and the wound resutured. Usually a bleeding socket responds to these measures. However, if bleeding continues, consideration should be given to the possibility of factors other than a purely local minor problem.
Bleeding, of almost any cause, can be arrested by packing the socket with gauze soaked in an antiseptic varnish. This material slowly sets to a firm consistency over hours to days and is well tolerated against bone. It does not become foul for a matter of weeks, so can be left in place for some time if necessary. Because of its consistency, the dressing can be compressed into the socket and secured readily with sutures. However, it should be removed, normally at about one week.
In trans alveolar (surgical) removal of teeth vigorous bleeding can occur from a defined point in the bone. Such bleeds are often best dealt with by pushing a small quantity of bone wax into the bleeding point. This material is not resorbable and tends to become infected if used in large quantities; it should thus be used sparingly. Alternatively, adjacent bone may be crushed into the bleeding point with artery forceps. Significant arterial or venous bleeds from soft tissue are best dealt with by ligation. A pair of artery forceps is clipped over the bleeding point, leaving the tips showing, then a suture (such as polyglycolic acid) is tied around the forceps and slipped over the end and tightened. Smaller bleeding points can be dealt with by diathermy or even by clipping the vessel temporarily without a suture. If bleeding continues despite reasonable attempts to stop it, or if it restarts within 3 days, bleeding and clotting function tests should be performed. These include the international normalized ratio (INR) (for the extrinsic part of the coagulation cascade), activated partial thromboplastin time (APTT) (for the intrinsic part) and a platelet count, which may be done as part of a full blood count that will also include hemoglobin estimation. Any further investigations that might be indicated as a result of these tests may be better performed in a hematology unit.
It is not usual to ask patients about to have extractions to stop taking drugs they are taking to reduce platelet activity such as aspirin. The incidence of abnormal bleeding in such individuals is low. Patients on warfarin therapy, however, require very careful management. It is now recommended that provided the INR is 4.0 or less on the day of extraction, treatment may proceed but the sockets should be dressed with a resorbablehaemostatic agent such as oxidized cellulose and sutured. Clinical trials have shown few serious bleeding complications with this approach.
Patients with a known blood-clotting disorder will be under the care of the regional hemophilia centre. Such units are generally extremely helpful in preparation and after care of the patient for dental purposes, but they must be consulted early in the planning process. Patients may require both factor replacement and antifibrinolytic medication.
Summary
Prevention of complications should be a major goal of the surgeon. Skillful management of complications when they do occur is the sine qua non of the wise and mature surgeon.
The surgeon who anticipates a high probability of an unusual specific complication should inform the patient and explain the anticipated management and sequelae. Notation of this should be made in the informed consent that the patient signs.
General complications, which occur after tooth extraction: miocardial infarction; stroke; subcutaneous emphysema, in cheek, neck or chest; bruise of sclera; hysteria; traumatic delirium; hyperthermia; cavernous sinus thrombosis.
Chapter 12. Inflammatory processes of maxillofacial area and neck
Inflammatory response results from interaction of exogenic (microbs, their toxins, waste and decay products) and endogenic ethiologic factors (factors and mechanisms of non-specific and immune responsiveness).
Up to now it has not been possible to determine the overall spectrum of inflammatory processes agents using microbiological diagnostic methods. Thus, clinicians and microbiologists considered aerobes to be the ethiological factor of these diseases, because only this type of bacteria has been detected in the researched material, provided by patients. With improvement of microbiological research methods it has become possible to obtain evidence that anaerobes can be agents of odontogenic infection. In the course of the researches carried out during the last few years it was ascertained that not only staphylococci, but also different representatives of gram-negative microflora: proteus, colibacillus, klebsiella and others belong to basic agents of acute odontogenic infection.
The great significance in ethiology of inflammatory diseases of the head and the neck has been attached recently to opportunistic microorganisms, asporous obligate anaerobic bacteria. Bacteroides and fusobacteria are the bacteria most frequently found among this type of bacteria. Usually these microorganisms can be found on mucous membranes of the oral cavity. When the immune responsiveness of an organism is decreased and hemodynamic in inflammatory tissue is induced, bacteroids, fusobacteria and other opportunistic anaerobic microorganisms can cause pyoinflammatory diseases.
The role of microflora is undoubtedly great. However, microorganism – macroorganism relations have two-way connection; therefore the peculiarities of the course of the inflammation and development of complications are related not only to the peculiarities of microflora, but also to organism responsiveness, that is the property of an organism to respond to changes in the environment.
In other words, responsiveness of an organism reflects the protective and adaptive properties of an organism and is caused by inherent and acquired factors. To a great extent it depends on sex, age, and environment conditions etc.
Considering the problem of the pathogenesis of acute odontogenic inflammatory diseases, great attention is paid to sensitization of organism, producing of specific antibodies in response to coming of the antigens into tissues. The coming of the antigens first occurs owing to their ability to penetrate deep into tissues through tissue barriers. As a result of forming and continuous existence of the chronic infection nidus the number of penetrating antigens increases and the level of sensitization rises. In response to this organism is constantly producing specific antibodies, which support antibacterial immunity.
The inflammatory process is likely to increase at the disturbance of the dynamic balance between micro- and macroorganism. It may be either the increase in the total effect, which damages from the direction of bacteria, or weakening or increase of reactivity.
One of the major factors which contribute to the beginning of inflammatory process is rise in summary effect, which damages virulence of microflora, as a result of increase in the number of microbes/microorganisms. Another significant factor is injury of the demarcation zone (connective tissue capsula or leukocytic bank), which occurs at the injury or operative treatment.
Development of acute suppurative inflammation against the background of the existing nidus of chronic infection arises as a rule after the physicalor emotional overstrain, supercooling, overheating, and also after certain diseases (especially infectious diseases).
The inflammatory processes of jaw are remarkable for a greater variety of their clinical course, that gives the basis for their various classifications. One of them was suggested by A. G. Shargorodskyi and L. M. Tsepov (1979)
Statistics:
- Per 1 person – 10 of thousand diseases, 100 thousand symptoms and syndromes.
- Per every third patient – with odontogenic inflammatory process:
- 20 % – general numbers of patients which have been sent to a polyclinic;
- 8 % – surgical stomatology of patients,13–39 % of which are hospitalized;
- 60 % – pyoinflammatory.
Signs for classifications of the acute odontogenicin flammatory processes
I. G. Lukomskii (1943) – 3 stages:
- A periodontitis and osteomyelitis.
- Perimaxillary phlegmon.
- Spreading phlegmon and sepsis.
A. I. Evdokimov and G. A. Vassilyev (1964) developed precise differential diagnostics of a acute periodontitis, periostitis, osteophlegmon, adenophlegmon and acute lymphadenitis.
Arguments:
- A. B. Izachik – lymphatic vessels (research – communication, anastomose between the bone, periosteum, periodontium, soft tissues).
- Lanuk – investigated a venous grid (research – communication, anastamoses between a bone, periosteum, a periodontium, soft tissues).
- Inflammatory process is distributed not only per continutatem, but also on venous and lymphatic vessels, not always is osteomyelitis.
- Current: hypoergic, hyperergic, anergic, normergic.
It is possible to separate a periodontitis as a standing alone disease (G. A Vassilyev., A. I. Evdokimov):
- Characteristic symptoms.
- Clinical course of disease at conservative surgical treatment.
- Modern morphological and paraclinical researches (blood from epicenter inflammatory process, infra-red radiation – thermo diagnostics) allow establishing the exact diagnosis of inflammatory process (O. M. Solntsev, A. M. Lihota).
- Patients are not hospitalized.
Another classification of the odontogenic inflammatory processes was proposed by A.G. shargorodskiy and L. M. Tsepov:
A. Periodontitis:
- Acute periodontitis (serous and purulent periodontitis).
- Chronic periodontitis in the stage of exacerbation.
- Chronic (granulating, granulomatous and fibrous periodontitis).
B. Jaw periostitis:
- Acute periostitis (serous and purulent).
- Chronic periostitis.
C. Jaw osteomyelitis:
- By clinical course: a) acute; b) subacute; c) chronic; d) aggravated chronic.
- By the character of the spread: a) limited; b) diffusion.
D. abscesses and phlegmons:
1) face; 2) perimaxillary; 3) floor of the oral cavity; 4) peripharyngeal; 5) tongue; 6) neck.
E. lymphadenitis of the face and neck.
Periodontitis
Periodontitis – inflammatory process which affects the tissue of the periodontium and bones that support the teeth. The main cause of periodontitis is complicated caries.
Distinct types of periodontitis:
- Acute periodontitis:
a) serous periodontitis (limited and generalised);
b) purulent periodontitis (limited and generalised).
- Chronic periodontitis:
a) granulating periodontitis;
b) granulomatous periodontitis;
c) fibrous periodontitis.
- Chronic periodontitis at the stage of exacerbation.
Clinical features of acute periodontitis. The initial symptom of acute serous periodontitis is toothache, which becomes stronger when biting. This pain doesn’t usually irradiate, so it’s easy for the patient to determine the affected tooth. Another characteristic of periodontitis is soft-tissue swelling, minor regional lymphadenopathy, slightly painful lymph nodes.
The affected tooth is a little loose and vertical percussion of the tooth is positive. At the same time there dental X-ray film shows no change. With the progression of the serous inflammatory process into purulent form of periodontitis the intensity of pain is growing. The pain becomes acute, throbbing and irradiates along the trigeminal nerve. There is acute pain every time one touches the tooth, which becomes loose. The patient notes that the tooth seems to be growing. The mouth of the patient is half-open, the mucous membrane of the alveolar process is hyperemic, edematous and painful within the borders of the injured tooth. Regional lymph nodes are enlarged and painful. Edema of the soft tissue is characteristic at this stage as well. There is deterioration of the general condition of the patient. The treatment of the acute periodontitis consists of creating an exudate outflow from the periapical region. The symptomatic and physical therapy is also used.
Chronic periodontitis
Chronic periodontitis (apical) is a chronic inflammation of periodontum, characterized by transition from acute phase into chronic one or by course. Chronic periodontitis is reported to be more frequent than acute one. The morphological and clinical pattern of chronic peridontitis is variable. It can be granulating, granulematous and fibrotic.
Granulating periodontitis is marked by painful sensation, which occasionally appears in the region of the affected tooth. There may be also no pain. It is clear from the anamnesis that tooth disturbs the patient for a long time.
Examining the tooth, it is easy to determine whether there is any filling or cavity, which can be sounded indolently. Percussion of the tooth is usually painless.
X-ray examination (Fig. 12.1) is of considerable importance in differential diagnostics of chronic periodontitis: fibrous periodontitis (Fig. 12.2) is marked by irregular enlargement of periodontal fissure; the characteristic feature of the granulomatous periodontitis (Fig. 12.3) is sharply delineated destruction zone of different shapes and size in periapical region; the granulating periodontitis (Fig. 12.4) is characterized by destruction of the alveolar socket and destructive changes in spongy substance without any distinguished boundary between pathologic zone and unaffected tissues.

Fig. 12.1. X-ray examination

Differential diagnostics. Acute periodontitis should be differentiated from pulpitis, periostitis, osteomyelitis, suppuration of apical cyst, odontogenic sinusitis. In acute periodontitis a person has a pain in bite or percussion, whereas in diffuse pulpitis it is permanent without any disturbance. In acute periodontitis there are inflammatory changes of the gingiva around the tooth, percussion is painful. Electroodontometric data may be useful for diagnosis.
In acute periodontitis a pain is located mainly in the tooth whereas in periostitis it lessens and the soft tissues edema increases. During the evaluation, a fever, collateral inflammatory edema of soft tissues and diffusive infiltration of transitional fold, with forming of an abscess are observed. Percussion of the casuative tooth in periostitis is negative or slight positive unlike acute peridontitis. Acute osteomyelitis of jaw is differentieted from periostitis at the same pattern as acute purulent periostitis. For the last it is peculiar to have bilateral infiltration of an alveolar process and body of a jaw. In acute periodontitis, percussion of causative tooth only is positive, whereas in acute osteomyelitis positive percussion and loosening of adjacent teeth are observed. And percussion of causative tooth is less painful than adjacent. Data of laboratory examination (blood test) can help in differentiating the diseases. It is necessary to differentiate acute periodontitis from suppuration of radicular cyst. For the last displacement of teeth and extrusion of the bone in the middle is peculiar. A bone lesion with robust edge is observed on X-ray.
The same clinical features are reported in acute periodontitis and odontogenous genyantritis. However in acute periodontitis, there is no stuffiness of a nose and no changes in maxillary sinus, which may be revealed with radiograph.
Odontogenic granuloma (subperiosteal, submucous, subcutaneous) can arise from spreading of granulations into submucous and subcutaneous soft tissues.
Clinical course of the process complicated with odontogenic granuloma is also quiet. There are no pain in the tooth. Inflammatory changes are accumulating in soft tissues.
In subperiostal odontogenic granuloma, bone extrusion in the middle of decayed tooth appears. The mucosa over the lesion is not changed, sometimes a few inflammatory signs can be observed.
Submucosal odontogenic granuloma is determined as local, solid formation, which is situated in submucosa of vestibular fold or cheek adjacent to the causative tooth and connected through the fistulous tract. Suppuration of submucosal granuloma is observed often. Discharging of pus through the fistula ensuing declination of process and scarring of the fistulous tract.
Round infiltration in subcutaneous fatty tissue is peculiar for hypodermic granuloma. It is solid, painless or slightly painful. A fistulous tract goes through the soft tissues from responsible tooth to granuloma. Hypodermic granuloma can suppurate. Skin adheses with underlying tissues, becomes reddish, fluctuation appears. Abscess discharges outside, breaking thinned skin. Diagnosis is based upon X-ray data. In periapical granulating periodontitis, it demonstrates changes spreading of periodontal fissure around root tip as a result of bone lesion. Bone lesion has irregular edge. Contours of root tip can be irregular due to resorbtion of the cement and dentine. In the presence of odontogenous granuloma in soft tissues, lesion around apex is of a small size.
Granulematous periodontitis is charachtarized by limited growth of granulation around the root tip. As a result of compaction of the tissues adjacent to granulation fibrous capsule formed.
Depending on the structure we distinguish:
1) simple granuloma, consisting of the elements of connecting (granulation) tissue;
2) epithelial, in which epithelium remnants are located between the areas of granulation tissue;
3) cyst-like granuloma, containing cavities, covered with epithelium.
Clinical features. A flow of granulematous peridontitis may be different. Quite often granuloma does not increase or grows slowly. Thus, patients do not complain. Only by chance in roentgenologic research a granulomatous lesion can be revealed. In some patients granuloma is gradually increased. Usually it is connected with intensifying of inflammatory process and proper changes in tissue of granuloma: by hyperemia, edema, neutrophilia, suppuration. In intensifying of chronic process, capsule of granuloma gets broken, and inflammatory and distrophic processes occur in adjacent tissues, with prevalence of destruction. It can be manifested differently. In some cases, sensitivity and pain of the tooth in percussion are present, in others signs of an acute periodontitis appear. Then, after declination of inflammation, barrage capsule forms around lesion again. Diagnosis is also based upon X-ray data. The radiogram reveales round lesion with robust edges. In inactive flow of granulomatous periodontitis, sclerotic bone around lesion can be observed.
Differential diagnostics. It is necessary to differentiate chronic granulomatous periodontitis from an apical cyst. On X-ray in granulomatous periodontitis the area of resorbtion of bone has a diameter of 0.5–0.7 cm, in a cyst – more considerable resorbtion of bone is visible with robust clear contours.
Fibrous periodontitis. In the end of acute process in periodontium or under the influence of medical measures, scarring can happen spontaneously both in granulating or granulomatous lesion resulted in bone recovery. The local inflammatory process formes around root tip due to growth of connective tissue. However, it is reported that fibrous periodontitis can occur spontaneously.
Clinical picture. In fibrous periodontitis, there are no complaints. Some acute signs can arise in recurrence. In the oral cavity decayed tooth with disintegrated pulp can be revealed. The tooth can slightly react to percussion. Diagnostics is based upon radiographic data. There are spreading of periodontium and compaction of bone around root tip.
Treatment. Surgical treatment of chronic peridontitis consists in extraction of the tooth, replantation, allotransplantation, dental implantation, apicoectomy, rootectomy, hemisection.
Hypodermic granuloma of the face
Hypodermic granuloma of the face is an uncommon disease and has a subacute flow. It manifests by nidal inflammation in hypoderma. More frequent hypodermic granuloma has odontogenic origin as a complication of chronic peridontitis. Similar features are observed in presence of a foreing body in hypoderma. Development of non-odontogenic hypodermic granuloma is caused by insertion of organic foreing bodies, though metal or glass particles do not lead to it.
This form of odontogenous inflammatory process can be also named as: migrating granuloma, hypodermic migrating granuloma, creeping migrating granuloma, migrating abscess and most often – hypodermic granuloma of the face.
In etiology of inflammatory process a leading role belongs to microorganisms which penetrate from the nidus of chronic granulating periodontitis into the hypoderma, where granulation tissue develops as separate malformation – granulomata. Odontogenic hypodermic granuloma is connected with the causative tooth. But not all of the authors uphold such view on the mechanism of development of odontogenic hypodermic granuloma. Some of them have not seen distinctions between it and superficial chronic lymphadenitis, because of similar clinical manifestations. Development of odontogenic hypodermic granuloma is closely related to the causal tooth, and its localization depends on the location of the last one.
Hypodermic granuloma can be single or multiple. Size of granuloma can vary (from 1 to 2–4 cm), borders are regular, there can be mild pain in palpation. The affected skin is thin, cyanotic, glossy, rough, folded. Fluctuation is determined but there is no pus after incision. Fluctuation is explained by formation of granulating tissues under the skin. The tract goes from granuloma to a responsible tooth.
Hypodermic granuloma of the face can have an odontogenic and nonodontogenic origin. In first case we always find a causative tooth and tract, which is going from tooth to granuloma, in the second – these signs are absent. In hypodermic granuloma the size of affection of the skin is equal to affection of underlying tissues, which is a peculiar feature of the disease.
In the development of odontogenic hypodermic granuloma, two stages are marked out: hidden, when changes of a skin are absent, and period of skin manifestations, when changes of skin are visible.
There are four clinical forms of hypodermic granuloma: initial, stationary, creeping, suppurating. In the initial form of disease changes of skin are absent, and in the area of causal tooth painless infiltration is determined, size of which does not exceed peas. In the oral cavity in this stage it is possible to reveal dense tract, which is going from the tooth to infiltration. The stationary form is characterized with the development of process on the limited area. For creeping form, involution in one area and intensificaton in another one is a peculiar feature. In the suppurative form hypodermic granuloma turns into an abscess.
The course of hypodermic granuloma is chronic and dull. Self recovery is not observed.
Treatment consists in tooth extraction, thorough curettage of the socket. The affected skin and fistulous tract must be excised. The defect of the skin, which has been formed due to excision, should be closed. Prevention of the disease consists in timely treatment of caries and its complications.
Tooth-preserving treatment is presented by several types of operations:
- Apical resection (Fig. 12.5).
- Radectomy (Fig. 12.6).
- Premolarization or coronary and radicular separation (Fig. 12.7).
- Hemisection of the tooth (Fig. 12.8).
- Ablation (amputation).
- Apical resection with retrograde filling.
- Dental reimplantation.

Periostitis of the jaw
Acute odontogenic periostitis is acute infection inflammation of the periosteum of the alveolar process or, that is more rarely, body of jaws. Periostitis is localized on the one side of the jaw, frequently affecting vestibular side, rarely – palatal or lingual surface. This disease is treated mainly at out-patient’s clinic.
Etiology and pathogenesis
Periostitis of the jaw develops as a complication of the acute or chronic periodontitis. It can be the result of the root or follicle cyst suppuration, or alveolitis. Periostitis sometimes develops in connection with a suppurative form of the periodontal disease. It can develop in complicated eruption of the wisdom tooth and, finally, accompanies an acute form of odontogenic osteomyelitis. Cooling, stress and inadequate nutrition are factors predisposing to the development of acute periostitis.
Clinical features
At the initial stage odontogenic periostitis can develop slowly, gradually, causing only the insignificant pain feelings. As far as expansion of inflammation area and accumulation of exudates under periostium take place subjective and objective signs of inflammation increase. However in the majority of patients periostitis develops quickly. The certain information in anamnesis is peculiar to the acute periostitis: increasing pain in a gangrenous tooth during previous days; in the beginning pain irradiates to ear, temple, eyes, but in the last days it diminished to some extend, but the facial swelling appeares or rapidly progresses. Touch to the tooth (by the tangle, tooth-antagonist, food, spoon) is painful, however not as much, as earlier, in the stage of acute suppurative periodontitis. Application of heat (rinse, hot-water bottles) does not help, and only facilitates the state to some extent (diminishes pain). Some phenomena associated with intoxication are present (languor, apathy, sometimes headache, increased temperature).
Within a few days from the beginning of the disease, the facial edema increased and pain became considerable (due to intensive tension and chemical irritation of the jaw periostium).
Objective signs depend on localization and extension of the inflammated area as well as on the microorganisms virulence and state of the immune system.
Considerable facial asymmetry is visible, if the process is localized on the vestibular side of the affected jaw. If maxilla is affected one can see the edema expanding to the lower eyelid, upper part of the cheek, parotid and masticatory area, upper lip, bottom of the nose, etc. If the mandible is affected the edema is present at the lower part of the cheek, corner of jaw, neck.
Facial asymmetry is absent, if suppuration spread on a palatal or lingual surface; in this case a subperiostal abscess will not influence the contours of the face. If the disease arises from the central incisor of the maxilla, an abscess can appear between the bottom of the nasal cavity and mucous membrane of the nose.
Examination of the oral cavity reveals edema, hyperemia and infiltration, smoothed vestibular fold, and then in 3–5 days fluctuation appears within the limits of 3–4 teeth.
If pus spreads to the corner and on the branch of the jaw, it results in trismus – inflammatory contraction of the jaws, as the refectory spasm of the inflamed masticatory and medial pterygoid muscles develops.
Especially severe clinical flow is typical to suppurative periostitis, localized on the hard palate. Formation of an abscess under palatal periostium is associated with appearance of semispherical or oval swelling with marked hyperemia. Pus accumulation under the periostium and mucous membrane, which is dense and thick in this region, causes slight aching in the beginning, and then sharp pulsating pain. The permanent contact of palatal abscess with a tangle causes increase in pain sensations.
X-ray examination of the bone in the affected area reveals only those changes, which were caused earlier by chronic inflammation around a gangrenous tooth. Usually there are typical signs of chronic periodontitis.
In accordance with clinical signs and localization of the inflammated area the following forms of acute odontogenic periostitis are distinguished: (1) serous and (2) suppurative.
It is necessary to perform differential diagnostics of acute periostitis with acute suppurative periodontitis, acute osteomielitis, facial abscesses and phlegmons.
Periodontitis (acute suppurative) differs by localization of the inflammation zone within the limits of one tooth, by the absence of edema on the face, by sharp pain in percussion of the affected tooth.
Acute osteomyelytis differs by the presence of the subperiostal reaction not from one, but from two sides of the alveolar process, and also more expressed general signs of intoxication – higher body temperature (up to 39–40 °C), pain, which arise in a few teeth during percussion, by the presence of severe bone injury resulting in necrosis and sequestration of certain areas of bone, more expressed changes in blood and urine.
A phlegmon is characterized not only by the edema of the skin but also by dense infiltration. The skin above it has signs of severe hyperemia, is glossy, the fold could not be formed during palpation. In periostitis the color of the skin is not usually changed, the infiltration of subcutaneous fat is absent. The general state is strongly affected in quickly increasing phlegmon: the body temperature is high, there are vivid changes in haemogram, reflecting the signs of festering process in an organism.
Treatment of acute periostitis is performed in a different way depending on the phase of illness development and objective status. In an initial period, when there are no signs of suppuration and fluctuation, and there is only a small infiltrate on the transitional fold (or on the palate), it is possible (if is necessary to preserve a tooth) to make an effort to attain reverse development of process by means of endodontic treatment and application warm (physiotherapeutic procedures) in combination with antibiotics and anti-inflammatory medicines.
In those cases, when a tooth is strongly destroyed, and its preservation does not represent any value, it is essential to extract the casual tooth and prescribe common treatment without thermal procedures (bleeding from an alveola is possible).
Usually patient applies for medical help to the dental clinics when inflammation is on its marked clinical stage, infiltrate is already clear outlined and subperiostal abscess is formed. The urgent wide cut of the mucous membrane and periostium (up to the bone) in the area of the most pronounced zone of abscess or infiltrate is indicated in this period. It is necessary to perform the periostotomy within the limits of 2–3 teeth (not less) for providing good outflow of the pus. Direction of the cut in a vestibulum is along the transitional fold, and on the palate – parallel to the gum. On the palate it is better to perform not a simple linear cut, but excising the three-cornered area of the mucousa and periosteum over the abscess. Simultaneously with a cut it is necessary to extract a “causal” tooth, if it is mostly destroyed and conservative treatment is impossible. In the case, when such tooth can be preserved for cosmetic or functional reasons, it is treated.
Chronic odontogenic periostitis
Chronic periostitis could be simple and ossificated. Patients complain of the deformation of the jaw and slight pain in it. Anamnesis is distinguished by pain in the affected tooth and its treatment.
Clinical features are marked by deformation of the face owing to the enlarged alveolar process of the maxilla or mandible, which is slightly painful when doctor touches it. Other distinctive characteristics are a little smoothed out transition fold and cyanotic mucous tunic. No intoxication is observed and the general condition is almost not affected.
Treatment including extraction or treatment of the affected tooth;
Periosteotomy in the region of the infiltration with the following draining of the wound, removing of the bone structure deformity; 3. Physical treatment modes appropriate for drained wound (phonophoresis of hydrocortisone, helium-neon exposure, electrophoresis of dimethylsulfonoxidum and iodide potassium).
Pericoronitis
Pericoronitis is the inflammation of the soft tissues surrounding the tooth crown in case of maleruption.
Eruption of wisdom teeth on a mandible, more rarely on maxilla, can be accompanied with different complications.
After emerging of cuspids, its distal surface remains closed with periosteum and gingiva. Debris and infection are accumulating under operculum. During mastication the operculum is injured resulting in erosion and ulcering. The infection spreading to the operculum tissues provokes inflammation.
In some cases it is possible to discover semilunar pocket behind the tooth in addition to expansion of periodontal fissure on an X-ray. It is considered that spreading of pericoronal space distal to the tooth crown up to 2 mm is a normal feature. In case of its enlargement, pathologic process can arise. Semilunar resobtion of the bone occurs behind wisdom tooth (Vassmund’s demilune). Bone resorbtion behind wisdom tooth is caused by chronic inflammation. In that case bony pocket is a reservoir for microorganisms. Later it gets closed and periodontal cyst can appear.
Classification of complications related with impacted wisdoms (according to Magid and Steinberg, 1970):
I. Inflammatory processes, spreading into soft tissues, covering and surrounding a tooth:
- Acute pericoronitis:
a) catarrhal (serous); b) mattery; c) ulcerous.
- Chronic pericoronitis.
II. Pathological processes, which are effecting soft tissues, surrounding a lower jaw:
- Acute purulent periostitis.
- Abscesses and phlegmons.
- Ulcerous stomatitis.
III. Pathological processes of the mandible:
- Odontogenous osteomyelitis:
a) acute; b) chronic.
- Periodontal cysts.
IV. Other complications (lesions of adjacent teeth, neuralgias, neuritis etc.).
In most authors opinion (A. T. Rudenko, 1961, 1971; E. A. Magid, V. M. Shteinberg. 1970, 1981, and other), wisdom teeth erupt at the age from 18 to 33. In this age, pericoronitis (acute and recurrent), lymphadenitis, abscesses and phlegmons are mostly reported. At the age of 26–30 periostitis and osteomyelitis are mainly observed.
Classification of complications related with impacted wisdoms (I. P. Gorzov, 1975)
A. Subsequent complications related to impacted teeth
I. Pericoronitis:
- Acute:
a) acute; b) purulent; c) ulcerous.
- Recurrent chronic.
II. Other complications:
- Complications related to adjacent teeth: a) caries; b) pulpitis; c) periodontitis.
- Periodontal cyst.
- Neuralgias of the III division of trigeminal nerve – symptomatic.
B. Complications of pericoronitis
- Acute purulent periostitis of the mandible.
- Abscesses, phlegmons in surrounding soft tissues.
- Osteomyelitis of the mandible: a) acute; b) chronic.
- Ulcerous stomatitis.
Concerning the late (50–60 year eruption of wisdom teeth, in most cases it is related to their passive baring as a result of atrophy of toothless alveolar process.
Pericoronitis is an inflammation of soft tissues, surrounding the crown of the wisdom tooth, at its incomplete eruption or maleruption. This complication is the most frequent. Depending on a clinical course, pericoronitis can be acute or chronic, early or late recurrent.
Pericoronitis arises because of trauma of mucosa above wisdom tooth. Soft tissues above a crown during mastication are easily injured. Microorganisms and debris can get into pocket having formed and cause inflammatory process.
A disease begins with the unpleasant feelings at the site of unerupted wisdom tooth. Soon pain in swallowing, difficulty of the opening the mouth, nausea, headache, anorexia, sleep disturbance, arising of body temperature occur. There are catarrh, festering and ulcerous pericoronitis depending on the clinical form. In catarrh inflammation operculum is hyperemic, swollen and infiltrated. In general there is no exertions from operculum, but in some cases serous exudate can be. In the purulent edema, hyperemia and infiltration of soft tissues increase, a pus from operculum is reported. Pain becomes more intensive, it can irradiate through adjacent trigeminal branches, jaw stiffness appears. In ulcerous form, the ulceration of flap can be observed. This process occurs due to constant injury of the gum with occlusion of antagonists. Ulcerous pericoronitis can be complicated with ulcerous stomatitis. The general condition of the patient gets worse, the temperature of body rises, pain increases, a bad odor appears from the mouth. The main feature of ulcerous stomatitis associated with pericoronitis is a lesion of soft tissues adjacent mandible on the similar side. Ulceration spreads on cheek mucosa, which is not typical for ordinary ulcerous gingivitis.
Clinical signs of chronic pericoronitis are scanty. Local symptoms are less expressed in comparing with acute forms. Opening of the mouth is free. There are serous or mattery discharges from operculum. In acute condition, symptoms of inflammation may appear.
Maleruption is often associated with acute lymphadenitis. Lymphadenitis quite often has chronic course.
Inflammatory infiltration of soft tissues adjacent lymphatic nodes is called periadenitis, and suppuration of lyphatic node is adenoabscess. Spreading of the infection and festering of surrounding soft tissues is called adenophlegmon.
The hidden nidus of infection, which is disposed under the operculum can cause cellulitis.
In recurrent pericoronitis small portions of infection infiltrate into adjacent soft tissues causing subcutaneous odontogenous granuloma.
Spreading of inflammatory process from a bony pocket and soft tissues to the periosteum leads to acute periostitis of jaw. Pain becomes more intensive, radiates through trigeminal branches, jaw stiffness appears. As a result of localization of inflammatory process on the internal surface of body or branch of a mandible there is a pain during swallowing. There is hyperemia, swelling and infiltration of gingiva. Quite often an inflammatory process spreads to pterygomandibular fold and palatine arch provoking parapharingeal abscess.
Odontogenous osteomyelitis of the mandible has severe course as a result of wisdom impaction, and localized in the ramus, rarely in the body of the mandible.
Treatment of inflammatory complications related to the impacted teeth.
It is indicated to remove the impacted tooth, when pericoronitis arises. Decision about tooth preservation depends on tooth position and lesion in bone adjacent to the impacted tooth. Complications manifested with abscesses and cellulitis require surgery treatment to provide adequate drainage.
Osteomyelitis of the jaws
Osteomyelitis is an inflammation of bone. The inflammatory process may spread through the bone to involve the marrow, cortex, cancellous portion, and periosteum. In the jaws osteomyelitis usually is caused by pyogenic organisms that reach the bone marrow from abscessed teeth or postsurgical infection. However, in some instances no source of infection can be identified, and hematogenous spread is presumed to be the origin. In some patients no infectious organisms can be identified, possibly because of previous antibiotic therapy or inadequate methods of bacterial isolation. Bacterial colonies also may be present in small, isolated pockets of bone that may be missed during sampling.
In patients with osteomyelitis, the bacteria and their products stimulate an inflammatory reaction in bone, causing destruction of the endosteal surface of the cortical bone. This destruction may progress through the cortical bone to the outer periosteum. In young patients, in whom the periosteum is more loosely attached to the outer cortex of bone than it is in adults, the periosteum is lifted up by inflammatory exudate, and new bone is laid down. This periostal reaction is a characteristic but not pathognomonic feature of osteomyelitis. The infection becomes established in the calcified portion of bone when pus in the medullary cavity and beneath the periosteum compromises or obstructs the blood supply. Following ischemia the infected bone becomes necrotic.
Classification of the jaw ostheomyelitis by etiology:
- Odontogenous – 12 % of patients in maxillofacial clinics.
- Hematogenous – mostly in infants, sepsis of the newborns.
- Traumatic – after jaw fractures.
- Specific (certain etiologic microbial factor!).
- Contact (present not in all classifications).
By the phase of the disease: acute (serous and purulent); subacute (identified not by all authors); chronic (destroyed and profilirative forms).
By the localization and spread of the process:
- Localized – around 2–3 teeth.
- Regional – alveolar process, body or ramus.
- Diffuse – total affection of the whole or half of the jaws.
Theories of pathogenesis:
- Infection and embolic theory (Bobrov, Lexner).
- Infection and allergenic theory (S. Derizhanov).
- Neuro-trofic theory (G. Semenchenko).
- Neuro-humoral theory (M. Solovjov).
- Microcirculation theory.
- Theory of infection with immune suppression (J. Jusubov).
- Multifactorial theory.
Acute phase osteomyelitis
The acute phase of osteomyelitis is caused by infection that has spread to the bone marrow. With this condition, the medullary spaces of the bone contain an inflammatory infiltrate consisting predominantly of neutrophils and, to a lesser extent, mononuclear cells. In the jaws the most common source of infection is a periapical lesion from a nonvital tooth. Infection also can occur as a result of trauma or hematogenous spread.
Predisposing factors:
The low incidence of osteomyelitis of the jaws is remarkable considering the high frequency and severity of odontogenic infections. This low incidence is a result of fine balance between the host resistance and the virulence of the microorganism.
The virulence of the microorganisms in addition to any conditions altering the host defense mechanism and alteration ofjaw vascularity are important in the onset and severity of osteomyelitis
Systemic conditions that alter the host’s resistance and influence profoundly the course of the disease include:
Diabetes mellitus, autoimmune disorders, agranulocytosis, anemia, especially sickle cell, leukemia, AIDS, syphilis, malnutrition, chemotherapy for cancer, steroid drug use.
The importance of controlling these conditions in order to achieve proper response from the treatment of osteomyelitis cannot be emphasized enough.
Alchohol and tobacco use are frequently associated with osteomyelitis.
Conditions that alter the vascularity of bone predispose patients to develop osteomyelitis; those include: radiation, osteoporosis, osteopetrosis, Paget’s disease, fibrous dysplasia, bone malignancy and bone necrosis caused by mercury, bismuth and arsenic.
Etiology and pathogenesis:
In infants and children osteomyelitis occurs most commonly in long bones primarily form hematogenous spread. While long bone osteomyelitis in adults and the majority of cases of jaw osteomyelitis is initiated by a contiguous focus.
In the jaws contiguous spread of odontogenic infections that originate from pulpal or periapical tissues is the primary cause of the disease.
Trauma, especially not treated compound fractures, is the second leading cause.
Infection from periostitis after gingival ulcerations, lymph nodes, infected furuncles or lacerations and hematogenous origin account for an additional small number in jaw osteomyelitis.
The extensive blood supply of the maxilla makes it less prone to osteomyelitis when compared to the mandible. The thin cortical plates and the porosity of the medullary portion preclude infections from becoming contained in the bone and facilitate spread of edema and purulent discharge into adjacent tissues.
The mandible in this aspect resembles long bones with a medullary cavity, dense cortical plates and well defined periosteum. The bone marrow is composed of sinusoids rich is reticuloendothelial cells, erythrocytes, granulocytes, platelets, osteblastic precursors as well as cancellous bone, fat tissue and blood vessels.
The bone marrow is lined by the endosteum a membrane of cells containing large numbers of osteoblasts. Bone spicules radiate centrally from the cortical bone to produce a scaffold of interconnecting trabeculae.
The cortical bone has a distinctive architecture that includes longitudinally oriented haversian systems (osteons). Each osteon has a central canal and blood vessel that provide nutrients by means of canaliculi to osteocytes contained within lacunae.
Volkmann’s canals create a complex interconnecting vascular and neural network that nourishes bone and allows for repair, regeneration and function demands. These canals connect the central canals among them and with the periosteum and the marrow spaces.
An outer fibrous layer and an inner layer of osteogenic cells that constitutes the periosteum, envelopes the cortical bone.
Compromise of blood supply is critical factor in establishment of osteomyelitis.
The primary blood supply to the mandible is from the inferior alveolar artery, while the periosteal supply is a secondary source.
The venous drainage from the mandible is directed to the pharyngeal plexus and to the external jugular vein.
Acute inflammation that causes hyperemia increased capillary permeability and infiltration of granulocytes is the process that leads to osteomyelitis.
Proteolytic enzymes are released and along with destruction by bacteria and vascular thrombosis ensue cause tissue necrosis.
If this pus is not walled off by the host and an abscess is not created or if the pus does not escape to surrounding soft tissue from the medullary bone then the process of osteomyelitis is initiated.
Necrotic tissue, dead bacteria within WBCs (pus) accumulate increasing intramedullary pressure resulting in vascular collapse, venous stasis and ischemia.
Pus travels through the Haversian system and the nutrient canals and accumulates beneath the periosteum which gets elevated from the cortex and further decreases the blood supply. The inferior alveolar neurovascular bundle is compressed further accelerating thrombosis and ischemia and results in osteomyelitis induced inferior alveolar nerve dysfunction. If the pus continues to accumulate then the periosteum is penetrated and mucosal and cutaneous abscess and fistulas may develop.
The periosteum in children is less well bound to the cortical bone thus allowing for more extensive elevation. As host defences are more effective and the therapy becomes more effective the process may become chronic. After the acute Inflammation regress, necrotized bone gets separated from the vital one forming sequestra. Small sections of bone may become completely lysed while larger ones may become isolated by a bed of granulation tissue encased in a sheath of new bone (involucrum). Sequestra may follow any of the following routes: may be revascularized, remain quiescent, resorb, or become chronically infected requiring surgical removal for complete resolution of the infection. When the involocrum is penetrated by channels, called cloacae, the pus escapes to the epithelial surface creating fistulas.
Microbiology
Appropriate collection and transportation of cultures are essential in accurate diagnosis and initiation of appropriate therapy. Repeated cultures, especially in cases of chronic osteomyelitis and chronic antibiotic therapy, are paramount for identification and isolation of the involved pathogen.
Appropriate collection and handling of specimen along with culture of all sequestra cannot be emphasized enough. Staphylococcus Aureus and epidermis were, until recently, estimated to be involved in jaw osteomyelitis 80–90 % of the times. With more sophisticated methods of collection and appropriate handling of cultures a hemolytic streptococcus is recognized as the primary organism along with oral anaerobes e.g. Peptostreptococcus, Fusobacterium and Provotela species.
Eikenella corrodens is isolated in high percentages form cultures along with Klesbsiella, Pseudomonas and Proteus species. Antibiotic treatment should therefore be directed towards Streptococcus spp and anaerobes and not towards staph. Staphylococcus spp are the most common organisms recovered from long bones in adults and are the most prominent in children and infants osteomyelitis.
Clinical Features
The acute phase of osteomyelitis can affect people of all ages, and it has a strong male predilection. It is much more common in the mandible than in the maxilla, possibly because of the poorer vascular supply to the mandible. The typical signs and symptoms of acute osteomyelitis are rapid onset, pain, swelling of the adjacent soft tissues, fever, lymphadenopathy, and leukocytosis. The associated teeth may be mobile and sensitive to percussion. Purulent drainage also may be present. Paresthesia of the lower lip in the third division of the fifth cranial nerve distribution is not uncommon. Peculiarities and differences if clinical flow of the mandible and maxillary osteomyelitis are presented in Table 12.1.
Table 12.1. Peculiarities and differences of clinical flow of the mandible and maxillary osteomyelitis
| In mandible |
In maxilla |
1. More prolonged and severe process, determined by mandible architectonics.
2. More often transformation into chronic phase.
3. Severe complications with infection spread into the neck spaces and mediastinum.
4. Disorders in bone microcirculation determined by block of the alveolaris inferior artery. |
1. Process is less severe (bone is more porotic and thin. It promotes the evacuation of suppurative exudates).
2. Always accompanied by sinusitis.
3. Transformation into the chronic phase is rare.
4. Sequestration of the bone is more frequent and less pronounced than in mandible. |
Radiographic features
Very early in the disease, no radiographic changes may be identifiable. The bone may be filled with inflammatory exudate and inflammatory cells and may show no radiographic change. The most common location is the posterior body of the mandible. The maxilla is a rare site. Acute osteomyelitis most often presents an ill-defined periphery with a gradual transition to normal trabeculae.
The first radiographic evidence of the acute form of osteomyelitis is a slight decrease in the density of the involved bone, with a loss of sharpness of the existing trabeculae. In lime the bone destruction becomes more profound, resulting in an area of radiolucency, in one focal area or in scattered regions throughout the involved bone. Later, the appearance of sclerotic regions becomes apparent. Sequestra may be formed which means the transformation to the chronic stage. In this stage they become more apparent and numerous. Acute osteomyelitis can stimulate either bone resorption or bone formation.
Portions of cortical bone may be resorbed. An inflammatory exudate can lift the periosteum and stimulate bone formation. Radiographically, this appears as a thin, faint, radiopaque line adjacent to and almost parallel or slightly convex to the surface of the bone. A radiolucent band separates this periosteal new bone from the bone surface. As the lesion develops into a more chronic phase, cyclic and periodic acute exacerbations may produce more inflammatory exudate, which again lifts the periosteum from the bone surface and stimulates the periosteum to form a second layer of bone. This is detected radiographically as a second radiopaque line almost parallel to the first and separated from it by a radiolucent band. This process may continue and may result in several lines (an onion-skin appearance), and eventually a massive amount of new bone may be formed. This is referred to as proliferative periostitis and is seen more often in children. The effects on the teeth and lamina dura may be the same as those described for periapical inflammatory lesions.
A two-phase nuclear medicine study composed of a technetium bone scan followed by a gallium citrate scan may help to confirm the diagnosis. With inflammatory lesions, a positive result on the technetium scan indicates increased bone metabolic activity, and a positive result on the gallium scan in the same location indicates an inflammatory cell infiltrate.
The differential diagnosis of the acute phase of osteomyelitis may include fibrous dysplasia, especially in children. Aside from the clinical signs of acute infection, the most useful radiographic characteristic to distinguish osteomyelitis from fibrous dysplasia is the way the enlargement of the bone occurs. The new bone that enlarges the jaws in osteomyelitis is laid down by the periosteum and therefore is on the outside of the outer cortical plate. In fibrous dysplasia the new bone is manufactured on the inside of the mandible; thus the outer cortex, which may be thinned, is on the outside and contains the lesion. This point of differentiation is important because the histologic appearance of a biopsy of new periosteal bone in osteomyelitis may be similar to that of fibrous dysplasia, and the condition may be reported as such.
Malignant neoplasia (e.g., osteosarcoma, squamous cell carcinoma) that invades the mandible at times may be difficult to differentiate from the acute phase of osteomyelitis, especially if the malignancy has been secondarily infected via an oral ulcer; this may result in a mixture of inflammatory and malignant radiographic characteristics. If part of the inflammatory periosteal bone has been destroyed, the possibility of a malignant neoplasm should be considered. The differential diagnosis may include other lesions that can cause bone destruction and may stimulate a periosteal reaction that is similar to that seen in inflammatory lesions. Langerhans’ cell histiocytosis causes lylic ill-defined bone destruction and often results in the formation of periosteal reactive new bone. This lesion rarely stimulates a sclerotic bone reaction such as that seen in osteomyelitis. Leukemia and lymphoma may stimulate a similar periosteal reaction.
Management
As with all inflammatory lesions of the jaws, removal of the source of inflammation is the primary goal of therapy. Antimicrobial treatment is the mainstay of treatment of acute osteomyelitis, along with establishing drainage. This may entail removal of a tooth, root canal therapy, or surgical incision and drainage.
Acute Suppurative osteomyelitis
The initial management usually is aided by hospitalization to administer high doses of antibiotic therapy, identify and correct host compromise factors and eliminate the cause (removal of a tooth), surgical incision and drainage, osteoperforation of the cortical plates, irrigation by antiseptics, antibiotics, enzymes, drainage and irrigation of the maxillary sinus and systemic: antibiotics, non steroid analgetics, desintoxication; immune correction, hyposensibilization, symptomatic.
Since many organisms are responsible for osteomyelitis and are resistant to penicillin, a drug effective against those should be added to the regiment.
Examples are: Penicillin + Metronidazole, Amoxicillin + Metronidazole, Amoxicillin + Clavulanate potassium and Ampicillin + Sulbactam sodium. Other effective regiments are Clindamycin, Clindamycin + metronidazole and Cephalosporines.
There are complications of the jaw osteomyelitis which could be divided into local: bone defects, resorbtive fractures, teeth and foliculi loss, affection of the jaw growth and general: sepsis, generalized infection, toxic shock.
The main factors of the chronic osteomyelitis development include: delay in medical care; inadequate treatment; insufficiency of the compensatory mechanisms.
Это содержимое тега макета H5
The chronic phase of osteomyelitis may be a sequela of inadequately treated acute osteomyelitis, or it may arise de novo. The hallmark of osteomyelitis is the development of sequestra. A sequestrum is a segment of bone that has become necrotic because of ischemic injury caused by the inflammatory process. Numerous forms of osteomyelitis have been described. For the sake of simplicity, we group them into two major phases, acute and chronic, recognizing that these represent two ends of a continuum without a definite separating boundary in the process of bone inflammation. If not controlled within 10–14 days after onset, then subacute suppurative ostemyelitis is established. Pus travels through haversian canals and accumulates under the periosteum which penetrates to spread through to soft tissues. Deep pain, malaise fever and anorexia are present. Teeth are sensitive to percussion and become loose. Pus may be seen around the sulcus of the teeth or through skin fistulas and is associated with fetid odor. The skin overlying the effected bone is warm, erythematous, tender to touch; firm cellulites with expansion of bone from periosteal activity and paresthesia of mental nerve, regional lumphadenopathy are usually present. Mild leukocytosis with a left shift and mildly elevated ESR are present but are not valid indicators of the course or the extent of the disease. If inadequately treated the progression to subacute or chronic form is warranted. Findings are limited to fistulas, induration of soft tissues with a thickened or wooden character to the affected area with pain and tenderness.
Primary chronic form is not preceded by an episode of acute symptoms, is insidious in onset with onset of mild pain, slow increase of jaw size and gradual development of sequestra, often without fistulas. Other forms of osteomyelitis have been described as separate and distinct clinicopathologic entities with unique radiographic features. These are Garre’s osteomyelitis and diffuse sclerosing osteomyelitis. They are considered to be the part of the same continuum. Garre’s osteomyelitis is an exuberant periosteal response to inflammation. Diffuse sclerosing osteomyelitis is a chronic form of osteomyelitis with a pronounced sclerotic response. It is important to understand that all these variations of osteomyelitis have the same underlying process of bone’s response to inflammation. The features expressed by each subtype represent only variations in the type and degree of bone reaction. Osteomyelitis may resolve spontaneously or with appropriate antibiotic intervention. However, if the condition is not treated or is treated inadequately, the infection may persist and become chronic in about 20 % of patients. Some chronic systemic diseases, immunosuppressive states, and disorders of decreased vascularily may predispose an individual to the development of osteomyelitis. For example, osteopetrosis, sickle cell anemia, and acquired immunodeficiency syndrome (AIDS) have been documented as underlying factors in the development of osteomyelitis.
Radiographic Features
As in the acute phase of osteomyelitis, the most common site is the posterior mandible. The periphery may be better defined than in the acute phase, but it is still difficult to determine the exact extent of chronic osteomyelitis. Usually a gradual transition is seen between the normal surrounding trabecular pattern and the dense granular pattern characteristic of this disease. When the disease is active and is spreading through bone, the periphery may be more radiolucent and have poorly defined borders. The internal structure comprises regions of greater and lesser radiopacity compared with surrounding normal bone. Most of the lesion usually is composed of the more radiopaque or sclerotic bone pattern. In older, more chronic lesions the internal bone density can be exceedingly radiopaque and equivalent to cortical bone. The rentgenogram shows irregular destruction of the bone tissue and sequestra. Sequestra on the upper jaw are formed during 3–4 weeks, while the sequestra on the lower jaw – during 5–6 weeks since the onset of the disease (Fig. 12.9).

Fig. 12.9. Irregular destruction of the bone tissue and sequestra
In these cases no obvious regions of radiolucency may be seen. In other cases, small regions of radiolucency may be scattered throughout the radiopaque bone. A close inspection of the radiolucent regions may reveal an island of bone or sequestrum within the center. Often the sequestrum appears more radiopaque than the surrounding bone (Fig. 12.10). Detection may require illumination of the radiolucent regions of the film with an intense light source.

Fig. 12.10. Sequester formation at different areas of mandible
CT is superior for revealing the internal structure and sequestra, especially in cases with very dense sclerotic bone. The bone pattern usually is very granular, obscuring individual bone trabeculae. Sequestra can be identified by closely inspecting a region of bone destruction (radiolucency) for an island of bone. This island of nonvital bone may vary from a small dot (smaller sequestra usually arc seen in young patients) to larger segments of radiopaque bone.
Computed tomography (CT) is the imaging method of choice. CT reveals more bone surface for detecting periosteal, new bone and is the best imaging method for detecting sequestra.
Chronic osteomyelitis often stimulates the formation of periosteal new bone, which is seen radiographically as a single radiopaque line or a series of radiopaque lines (similar to onion skin) parallel to the surface of the cortical bone. Over time the radiolucent strip that separates this new bone from the outer cortical bone surface may be filled in with granular sclerotic bone. When this occurs, it may not be possible to identify the original cortex, which makes it difficult to determine whether the new bone is derived from the periosteum. After a considerable amount of time the outer contour of the mandible also may be altered, assuming an abnormal shape, and the girth of the mandible may be much larger than on the unaffected side. The roots of teeth may undergo external resorption, and the lamina dura may become less apparent as it blends with the surrounding granular sclerotic bone. If a tooth is nonvital, the periodontal ligament space usually is enlarged in the apical region. In patients with extensive chronic osteomyelitis, the disease may slowly spread to the mandibular condyle and into the joint, resulting in a septic arthritis. Further spread may involve the inner ear and mastoid air cells. Chronic lesions may develop a draining fistula, which may appear as a well-defined break in the outer cortex or in the periosteal new bone.
Differential diagnosis
Very sclerotic, radiopaque chronic lesions of osteomyelitis may be difficult to differentiate from fibrous dysplasia, Paget’s disease, and osteosarcoma. In children, osteomyelitis with a proliferative periosteal response may be misinterpreted as fibrous dysplasia. Differentiation of the chronic form of osteomyelitis may be even more difficult if considerable remodeling and loss of a distinct original cortex have occurred. In these cases, inspection of the bone surface at the periphery of the lesion may reveal subtle evidence of periosteal new bone formation. The presence of sequestra indicates osteomyelitis. Paget’s disease affects the entire mandible, which is rare in osteomyelitis. Periosteal new bone formation and sequestra are not seen in Pagct’s disease. Dense, granular bone may be seen in some forms of osteosarcoma, but usually evidence of bone destruction is found. A characteristic spiculated (sunray-like) periosteal response also may be seen. As mentioned in the section on acute osteomyelitis, other entities such as Langerhans’ cell histiocytosis, leukemia, and lymphoma may stimulate a similar periosteal response, but these usually produce evidence of bone destruction.
The imaging method of choice for aiding in the differential diagnosis is CT because of its ability to reveal sequestra and periosteal new bone. Also, CT allows accurate staging of the disease, which is important for future assessment of healing. Scintigraphy using bone scans, gallium, or labeled white blood cells is not particularly useful for differential diagnosis. Bone scans indicate increased bone formation, which is nonspecific, and often gallium scans (which highlight inflammatory cells) are not supportive.
Management
Chronic osteomyelitis tends to be more difficult to eradicate than the acute form. In cases involving an extreme osteoblastic response (very sclerotic mandible), the subsequent lack of a good blood supply may work against healing. Hyperbaric oxygen therapy and creative modes of long-term antibiotic delivery have been used with limited success. Surgical intervention, which may include sequestrectomy, decortication, or resection, often is necessary. The probability of successful treatment, especially when using long-term antibiotic therapy with decortication, is greater in the first two decades of life.
Principles of treatment are:
- Evaluation and correction of compromised host defenses.
- Gram staining and culture and sensitivity testing.
- Imaging of the region to determine the extend of the lesion and to rule out the presence of tumors.
- Empirical administration of Gram stain-guided antibiotics.
- Removal of loose teeth and sequestra.
- Prescription of culture-guided antibiotic therapy.
- Possible placement of irrigating drains / polymethylmethacrylate antibiotic beads.
- Sequestrectomy, debridement, decortication, resection or reconstruction as indicated.
Hyperbaric oxygen therapy, it has been used to promote healing in refractory chronic osteomyelitis. In situations in which osteomyelitis is associated with decreased systemic blood flow (e.g., in diabetes, vasculitis) or segmental blood flow (eg, in trauma), hyperbaric oxygen therapy may be used as adjunctive therapy. Reduced oxygen tensions in infected bone have been shown to interfere with normal polymorphonuclear leukocyte activity. Hyperbaric oxygen therapy has been shown to increase the oxygen tensions within infected bone, thereby augmenting polymorphonuclear leukocyte and macrophage activity.
Wound healing is a dynamic process that requires an adequate oxygen tension to proceed. In the ischemic or infected wound, hyperbaric oxygen therapy provides oxygen to promote collagen production, angiogenesis, and ultimately wound healing. Referral for hyperbaric oxygen is made whenever refractory osteomyelitis occurs or a soft tissue infection develops that is not amenable to a local or microvascular flap.
Surgical therapy: Surgical management of contiguous focus osteomyelitis can be very challenging. The principles of treating any infection are equally applicable to the treatment of infection in bone. These include adequate drainage, extensive debridement of all necrotic tissue and obliteration of dead spaces, stabilization, adequate soft tissue coverage and restoration of an effective blood supply.
The number and nature of the required surgical procedures increases with the severity of the infection, which can be divided into 4 categories, as follows:
- Category 1 – Removal of necrotic tissue by extensive debridement.
- Category 2 – Dead space obliteration with flaps, antibiotic beads, and bone grafts.
- Category 3 – Provision of soft tissue coverage of the bone.
- Category 4 – Stabilization of bone by external or open reduction and internal fixation.
Category 1
Debridement surgery is the foundation of osteomyelitis treatment. It is the most commonly performed procedure and may need to be repeated multiple times. The goal of debridement is to reach healthy, viable tissue, but even when all necrotic tissue has been adequately debrided, the remaining bed of tissue must be considered contaminated with the responsible organism. Debridement should be direct, atraumatic and executed with reconstruction in mind. All dead or ischemic hard and soft tissue is excised unless a noncurative procedure has been chosen. Surgical excision of bone is carried down to uniform haversian or cancellous bleeding, known as the paprika sign.
Sequestrectomy: sequestra which can be cortical or cortico-cancelous are usually seen after 2 weeks from the onset of the infection and once fully formed can persist for several months. Sequastra are avascular therefore poorly penetrated by antibiotics. Sequastra can be removed with minimaltrauma, but the risk of subjecting the patient to a chronic infection and prolong antibiotic treatment should be bared in mind.
Sequestectomy and Saucerization: saucerization is the unroofing of the bone to expose the medullary cavity. This is usefull in chronic osteomyelitis, since it permits excision of sequestra either formed or forming ones. It should be performed as soon as the acure stage has resolved, so to decompress the bone allow for extrusion of pus, debris and avascular bone.
Procedure
A full thickness mucoperiosteal flap is reflected usually buccaly, to exposed infected bone. Reflection should not comprise blood supply.
Loose teeth and bony sequestra are removed.
The lateral cortex of the mandible is reduced, until bleeding bone is encountered, producing a saucerlike defect.
All granulation tissue and loose bony fragments are removed, irrigation follows and hemostasis is achieved.
The wound is packed lightly with gauze covered with triple antibiotic ointment and the flap is loosely sutured over. The packing is removed 3–6 days and is replaced several times until the surface of the bone is epithelialized.
There is minimal or no risk of fracture in the jaws with this type of procedure unlike long bones. In long bones primary closure and immediate bone graft may be required.
Saucerization is rarely required for the maxilla.
Decortication
First introduced in 1917 and further described by Mowlem, decortication involves removal of the chronically infected cortex, usually the buccal and the inferior border are removed 1–2 cm beyond the affected area. It can be used as initial treatment of primary or secondary chronic osteomyelitis or more commonly when initial conservative treatment has failed.
Procedure
Full thickness mucoperiosteal flap is reflected buccaly and extends to the inferior border.
Involved teeth are removed.
The buccal cortex and the inferior borders are removed until bleeding bone is encountered.
Primary closure is achieved and pressure dressing is applied to maintain close contact of the bone bed to the vascular soft tissue. Irrigation tubes and or antibiotic beads may be placed.
If extensive debridement is required and the remaining bone is suspected to be prone to fracture, appropriate stabilization and reconstruction should be performed.
Resection and reconstruction
May be required for low-grade persistent or chronic osteomyelitis. It is especially used in cases of persisted infection after decortication, marked disease involving both buccal and lingual cortices and in cases of pathologic fractures.
Category 2
Adequate debridement may leave a large bony defect (dead space). Appropriate management of dead space created by debridement surgery is mandatory in order to arrest the disease and to maintain the integrity of the skeletal part. The goal of dead space management is to replace dead bone and scar tissue with durable vascularized tissue. Local tissue flaps or free flaps may be used to fill dead space. An alternative technique is to place cancellous bone grafts beneath local or transferred tissues where structural augmentation is necessary. Careful preoperative planning is critical for conservation of the patient’s limited cancellous bone reserves. Open cancellous grafts without soft tissue coverage are useful when a free tissue transfer is not a treatment option and local tissue flaps are inadequate.
Complete primary or delayed primary wound closure should be performed whenever possible. Suction irrigation systems are not recommended because of the high incidence of associated nosocomial infections and the unreliability of the apparatus. Healing by secondary intent is also discouraged since the scar tissue that fills the defect may later become avascular. Antibiotic-impregnated acrylic beads can be used to sterilize and temporarily maintain dead space. The beads are usually removed within 2–4 weeks and replaced with a cancellous bone graft. The most commonly used antibiotics in beads are vancomycin, tobramycin and gentamicin. Local delivery of antibiotics (amikacin, clindamycin) into dead space also can be achieved with an implantable pump.
Category 3
Adequate coverage of the bone by soft tissue is necessary to arrest osteomyelitis. Most soft tissue defects are closed primarily, but small soft tissue defects may be covered with a split thickness skin graft. In the presence of a large soft tissue defect or an inadequate soft tissue envelope, local muscle flaps and free vascularized muscle flaps may be placed in a 1- or 2-stage procedure.
Local and free muscle flaps, when combined with antibiotics and surgical debridement of all nonviable osseous and soft tissue for chronic osteomyelitis, have a success rate ranging from 65 % to 100 %. Local muscle flaps and free vascularized muscle transfers improve the local environment by supplying blood vessels, which are critical for host defense, antibiotic delivery, and osseous and soft tissue healing.
Category 4
If movement is present at the site of infection, measures must be taken to achieve permanent stability of the skeletal unit. Stability can be achieved with plates, screws, rods, and/or an external fixator. One type of external fixation allows bone reconstruction of segmental defects and difficult infected nonunions. The Ilizarov external fixation method uses the theory of distraction histogenesis, in which bone is fractured in the metaphyseal region and slowly lengthened. The growth of new bone in the metaphyseal region pushes a segment of healthy bone into the defect left by surgery. The Ilizarov technique is used for difficult cases of osteomyelitis when stabilization and bone lengthening are necessary. It also can be used to compress nonunions and correct malunions, and in a small group of patients for reconstruction of difficult deformities that result from osteomyelitis.
However, this technique is labor intensive and requires an extended period of treatment, averaging 9 months in the device. The Ilizarov pins usually become infected, and the device is painful. Infected pseudoarthrosis with segmental osseous defects can be treated by debridement and microvascular bone transfers. Vascularized bone transfer is also useful for the treatment of infected segmental osseous defects of long bones that are more than 3 cm in length. Vascularized bone transfers can be placed after 1 month without clinical evidence of infection.
Loss of bone stability, bone necrosis, and soft tissue damage frequently occur in contiguous focus osteomyelitis. Surgical debridement of infected bone and soft tissue provides specimens for culture and hastens eradication of the infection. Other steps in the surgical management of contiguous focus osteomyelitis should be tailored to the specific anatomy of the bone infection. When osteomyelitis is characterized by a full thickness, cortical sequestration, patients usually can be treated with removal of the dead infected bone (bone saucerization). Bone grafting may be necessary to augment structural support. These patients may require external fixation for structural support while the bone graft incorporates. Complex reconstruction of both bone and soft tissue is frequently necessary.
In some cases, osteomyelitis progresses to an infection involving the entire diameter of the bone. These patients often require an intercalary resection of the bone in order to arrest the disease process. Since this advanced stage of osteomyelitis involves an entire through-and-through section of bone, a loss of bony stability occurs either before or after debridement surgery. As a result, treatment often must be directed toward establishing structural stability and obliterating debridement gaps by means of cancellous bone grafts or the Ilizarov technique. Vascularized bone grafting is the other possible treatment modality.
Abscesses and phlegmons of the maxillofacial region
Phlegmon – (Greek inflammation) – diffuse purulent inflammation of hypodermal, submocousal, intermuscle and interfascial cellular tissue.
Abscess – localized purulent inflammation which occurs as a result of purulent desintigration of hypodermal, submocousal, intermuscle and interfascial cellular tissue or lymphatic nodes.
Microorganisms are the main etiology factor in beginnings of purulent inflammation, which are distinguished by aerobes (78.8 %), anaerobes – 21.2 %. Monoculture – 67.5 % (aerobes – 56.7 %, anaerobes – 8.8 %). Aerobes – staphylococcus aureus, staphylococcus epidermidis, E. coli, St. haemoliticus, enterococcus, proteus, diplococci. Anaerobes Gr(-) – bacteroides, streptococci – 19 % (floor of the oral cavity) Gr(+) – peptostreptococci, eubacteria – 10 %. In monoculture St. epidermidis, veilonellae, peptostreptococci was inoculated.
Sources of infection include odontognic (84 %), stomatogenic (gingival, mucosal), endosseous, salivary, tonsillar, rhinogenic, otogenic.
For optimal planning of approach to inflammation nidus against anatomic location in soft tissue, there is clinical anatomic classification of abscesses and phlegmons.
I. Abscesses and phlegmons at maxilla:
- Infraorbital region.
- Zygomatic region.
- Orbital area (upper and lower eyelids).
- Temporal region.
- Infratemporal and pterygopalatine fossa.
- Hard and soft palate.
II. Abscesses and phlegmons at the mandible:
- Submental space.
- Buccal area.
- Submandibular area.
- Pterygomandibular space.
- Parapharingeal space.
- Submasseteric (masseteric) space, parotid region.
- Retromandibular fossa.
III. Abscesses and phlegmons of the floor of the mouth:
- Upper division of oral cavity floor;
- Sublingual space;
- Lower division of oral cavity floor.
IV. Abscesses and phlegmons of the tongue:
- The tongue.
- The tongue root.
V. Abscesses and phlegmons of the neck:
- Superficial, deep, space of neurovascular bundle, paratracheal and paraesophageal space, paravertebral space.
Classification of abscesses and phlegmons (M. V. Farbicant, 1935):
- Paramaxillar:
- subcutaneous;
- phlegmons of intercelular space are always diffuse.
- Adenophlegmons.
- Osteophlegmons.
Classification of abscesses and phlegmons (A.i. Evdokimov, 1964):
- Phlegmons and abscesses in anatomic regions (cheeks, orbits, zygomatic and temporal regions).
- Paramaxillar and paramandibular phlegmons.
- Phlegmon of the mouth floor.
- Parapharingeal.
- Phlegmon of the tongue.
- Phlegmon of the neck (lower than upper neck fold).
Spreading of phlegmons realize per continuitatem; through lymphatic vessels; through venous vessels; trough arterial vessels.
Clinical signs
General signs of severe intoxication are marked by nausea, anorexia, general sweating, increasing of pulse and breathing rate. Sometimes – thrombosis of face and neck veins. Significant leucocitosis in periferial blood, leukocyte shift, increasing of neutrophils, decreasing of eosinophils, ESR – up to 70 mm per hour. In more severe conditions of the patient lymphopenia develops (amount of leukocytes decreases to 10 %), against the background of which eosinophiles deplete, and amount of neutrophiles increases up to 80 % and more. It can be sign of toxic nephritis. Necrotic and gas phlegmons have the severest course. Thermoregulation disorders – body temperature arises to 39.5–40 °C. If general intoxication increases dramatically, and local inflammation is low it can evident about infiltration of infection through local reticuloendothelial barrier and regional lymphatic nodes, which indicates to decreasing of resistance and could be the basis for unfavorable prognosis.
Local signs rely on location:
- Superficial phlegmons – presence of diffuse swelling is peculiar, swelling is tight and painful, skin hyperemia; skin cannot be folded, tensed and glossy; the face is asymmetric. There is a clinical case with typical signs of superficial phlegmon (Fig. 12.11).
- Deep phlegmons (in pterygomandibular and parapharingeal space, in the depth of the tongue and so forth) skin changes and face asymmetry are absent or insignificant. Keep in mind the signs of inflammation by Halenus and Celsus: tumor, rubor, color, dolor, functio lease.
More or less significant disorder of mandible movement up to stiffness (trismus).Impairment and severe pain in mastication and swallowing, especially in pterygomandibular and submasseteric phlegmons, and in other cases, when masticatory muscles involved in inflammation.Impairment of articulation, speaking and breathing (as a result of swelling of oral cavity, trachea, vocal cords). Saliva becomes tough, viscous and it spits out with difficulties.
By clinical course phlegmons are divided to:
- 1 group – mild – phlegmons located in 1 anatomic region.
- 2 group – moderate – phlegmons located in 2–3 anatomic regions.
- 3 group – severe – phlegmons of the mouth floor, half of the face, and two different anatomic regions.
Course severity depends on microbiotic virulence and condition of the immune system.
In case of the anaerobic phlegmon of the mouth floor (Ludwig’s angina), the clinical course is of major importance. Anaerobic infection is marked by crepitation symptom (gases are accumulated in the subcutaneous fat and are cracking during palpation, resembling the creak of snow); necrotic mass is determined during draining of the nidus; muscles achieve the colour of the boiled meat; foul, grey substance is exuded, there is no pus.
Treatment consists of such principles: 1. Drain of abscesses and phlegmons via incision (under general anaesthetic) taking into consideration their localization, spreading of the n.facialis bacillus, natural folds of face, neck and creating of the favorable conditions for exudate outflow. 2. Draining of the inflammatory nidus. 3. In case of odontogenic origin of the disease – extraction of the affected tooth. 4. Bacterial examination for determining of the microflora antibiotic susceptibility. 5. General medical treatment (anti-inflammatory, antibiotic, detox, hyposensitive, fibrinolytic, immune therapy, desagregants – aspirin, trental, ticlid).
In case of the Ludwig’s angina:
Drain of the abscesses, phlegmons, infiltrates by means of section in the submaxillary, retromandibular, submental regions, joined by means of the perforated tube drainage.
Creating of the highest possible conditions for aeration of the wound, its dialysis with antiseptic liquid and oxidizing substances.
Prevention of the joining of the commonplace microflora.
Anti-inflammatory, antibiotic, detox, hyposensitive, fibrinolytic, immune therapy, desagregants – aspirin, trental, ticlid.
Antigangrenous serum (preventive dose, or therapeutic dose if necessary).
Wound draining to be carried out with drains, draining sorbents, dialysis.
Sorbents: uvesorb, carbovit, carbolong, enterosgel – per os, sorbilact, rheosorbilact (i/v).
There are some forms of dialysis: fractional, continuous, circulating, aspirating. Detoxication includes hemosorbtion – arteriovenous shunt, plasmasorption, lymphosorbtion. Blood processing by UV, helium – neon laser, infrared rays (for improvement of rheologic properties).
Wound management in postoperative period is distinguished by wound processing with pulsing current, vacuum processing of the wound, laser processing + photosensitive agents based on hematoporphirines – discharged oxigen amplifies antimicrobic effect, ultrasound wound processing, cryoprocessing, hyperbaric oxigenation.
Accelaration of wound healing is reached by preparations, which stimulate wound healing, physiotherapy, diet, primary delayed sutures (2–5 day), secondary delayed – on granulating wound – 7–10–12 days. Contraindications – fever, hematogenous osteomyelitis and immune disorders (diabetes mellitus, rheumatism, poliarthritis, nephritis, chronic radial disease.), hemo-, plasma-, lymphosorbtion.
Complications
Complications of the abcesses and phlegmons could be general: phlegmon of retrobulbal cellulae. Thrombophlebitis of facial veins, sepsis, mediastinitis, thrombosis of cavernous sinus (7.1 %), purulent basal meningitis (2.6 %), arachnoiditis etc.:
- in favorable course – in 13 % of patients;
- in unfavorable course – in 80 % of patients.
Pneumonia, pleuritis (metastatic – 14 %, kidney abscess – 7.1 %). DIC – syndrome of disseminating intravascular clotting.
Furuncle and carbuncle
Furuncle – acute purulo-necrotic inflammation of a hair follicle and surrounding tissues caused by pathogenic microorganisms, more often by staphylococcal infection.
Carbuncle – acute purulo-necrotic inflammation of several hair follicles which are close to each other, and sebaceous glands, and also extend to surrounding tissues (skin, hypoderm).
Predisposing factors to development of furuncles or carbuncles are skin pollution, microtraumas, especially after squeezing out of abscesses on a skin, increased perspire and increased fat production. Very often these processes arise in people suffering from hypovitaminoses, with carbohydrate metabolism disorders (diabetes), with parallel conditions (overheat, supercooling, etc.).
The most dangerous in the prognostic plan are furuncles and carbuncles which are situated in a site of the upper lip, mouth angles and infraorbital site. It is associated with the mesh structure of piogenic membrane, which surrounds furuncles and carbuncles, instead of formation of a solid “bank” as it is in the abscesses. Therefore squeezing of abscesses can lead to development of dangerous to patient’s life complications. There is clinical case of furuncle of the buccal region (Fig. 12.12).

Fig. 12.12. Clinical case of furuncle of the buccal region
Complication of furuncles and carbuncles can be divided on local and general.
Local complications:
- Cheilitis (catarral, glandularis, impetiginous).
- Phlebitis, thrombophlebitis.
- Lymphangitis, serous and purulent lymphadenitis, periadenitis, adenophlegmons.
- Inflammatory infiltrates, abscesses, phlegmons.
- Osteomyelitis.
- Different forms of an erysipelas.
General complications: sinus thrombosis; meningitis; different forms of a sepsis.
The main tasks of a doctor during the treatment of patients with furuncles and carbuncles are reduction of the terms and prevention of the development of local and general complications.
Erysipelas
Erysipelas (Greek spuamsAa – red skin) (also known as “Ignis sacer,” and “St Anthony’s fire” is an acute streptococcus bacterial infection of the dermis, resulting in inflammation and characteristically extending into underlying fat tissue.
Most cases of erysipelas are due to Streptococcus pyogenes (also known as beta-hemolytic group A streptococci), although non-group A streptococci can also be the causative agent. Historically, the face was most affected; today the legs are affected most often.
Erysipelas infections can enter the skin through minor trauma, eczema, surgical incisions and ulcers, and often originate from strep bacteria in the subject’s own nasal passages.
Clinical forms distinguish: erythematous; erythematous bullous; erythematous hemorrhagic; bullous hemorrhagic.
Patients typically develop symptoms including high fevers, shaking, chills, fatigue, headaches, vomiting, and general illness within 48 hours of the initial infection. The erythematous skin lesion enlarges rapidly and has a sharply demarcated raised edge (Fig. 12.13). It appears as a red, swollen, warm, hardened and painful rash, similar in consistency to an orange peel. More severe infections can result in vesicles, bullae, and petechiae, with possible skin necrosis. Lymph nodes may be swollen, and lymphedema may occur. Occasionally, a red streak extending to the lymph node can be seen.

Fig. 12.13. The erythematous skin lesion
The infection may occur on any part of the skin including the face, arms, fingers, legs and toes, but it tends to favor the extremities. Fat tissue is most susceptible to infection, and facial areas typically around the eyes, ears, and cheeks. Repeated infection of the extremities can lead to chronic swelling (lymphangoitis). This disease is mainly diagnosed by the appearance of well-demarcated rash and inflammation. Blood cultures are unreliable for diagnosis of the disease, but may be used to test for sepsis. Erysipelas must be differentiated from herpes zoster, angioedema, contact dermatitis, and diffuse inflammatory carcinoma of the breast. Erysipelas can be distinguished from cellulitis by its raised advancing edges and sharp borders. Elevation of the antistreptolysin O titre occurs after around 10 days of illness.
There are some severe complications: spread of infection to other areas of body through the bloodstream (bacteremia), including septic arthritis and infective endocarditis (heart valves); septic shock; recurrence of infection – Erysipelas can recur in 18–30 % of cases even after antibiotic treatment; lymphatic damage; necrotizing fasciitis; treatment.
Depending on the severity, treatment involves either oral or intravenous antibiotics, using penicillins, clindamycin or erythromycin. While illness symptoms resolve in a day or two, the skin may take weeks to return to normal.
Because of the risk of reinfection, prophylactic antibiotics are sometimes used after resolution of the initial condition.
The maxillary sinusitis
The infectious-inflammatory disease characterized by involving in the inflammatory process of the sinus mucousa.
Distinguish rhinogenic, odontogenic, allergic or an extent maxillary sinusitis.
Odontogenic maxillary sinusitis according to different authors makes from 3 to 4.2 % of number of the admitted patients. Given statistical data concerning patients of the maxillofacial department as patients of the given group also can undergo treatment in ENT-department.
As a result of acute and chronic odontogenic inflammatory processes in the maxillary region there can be inflammation of maxillary sinus.
Comparatively frequent origin of odontogenic antritis is explained by the near location of apexes of the roots of the second premolar, first and second molar, more rarely – the third molar to the sinus (Fig. 12.14).

Fig. 12.14. The location of apexes
1 – saggital position,
2 – horizontal position
Sometimes apexes of the roots of these teeth are dissociated from the sinus by a thin bone plate, and on occasion – only by one mucus membrane (to 40 % cases). These anatomic features facilitate the breach of pus in the sinus cavity at acute purulent processes in the area of the second premolar and molars and explain possibility of connection of sinus with the cavity of the mouth during extraction of tooth with its next infecting by a mouth liquid.
A chronic process near the apexes of teeth, spreading toward the sinus, can entail thinning, up to complete disappearance of bone layer between the apex of tooth and sinus cavity and transition of inflammation to the mucous membrane of the sinus (Fig. 12.15).

Fig. 12.15. Complete disappearance of the teeth roots bone layer between the apex of tooth and sinus cavity
Also inflammatory process can extend to ossteomyelitic process or as a result of a suppuration of new growths of the upper jaw. An immediate cause of development of an inflammation is the microbic microflora. In odontogenic maxillary sinuitis staphylococcus is more often sown – both in a monoculture, and in microbic associations.
Odontogenic maxillary sinusitises divide into the acute, chronic, becoming aggravated chronic one. Among them is subacute, an initially-chronic sinusitis. And also they divide in opened (after perforation) and closed ones. Classification by pathologoanatomic signs: catarrhal; purulent; polypous; purulent-polypous.
Acute odontogenic maxillary sinusitis is difficult enough for differentiating from an aggravated chronic one. This proceeds and can come to an end with the treatment or transition into a chronic process. Often enough unique acknowledgement of the diagnosis is the absence of similar aggravations in the anamnesis. For a clinical picture odontogenic maxillary sinusitis are characterized by tearing pain, sense of weight in the infraorbital area, a pain can simulate that in a pulpitis, the body temperature is raises, depending on a type of reactivity. In the oral cavity causal tooth can be found, painful on percussion, an X-ray examination reveals destructive inflammatory process or cyst. On roentgenograms of the maxillary sinus opacity is observed. The maxillary sinus puncture makes it possible to finalise the diagnosis.
Local treatment consists of the creation of conditions for outflow of exudates from the maxillary sinus that is provided either by vasoconstrictive therapy or maxillary sinus puncture, and also in sanitation of odontogenic source by removal of a tooth or its endodontic treatment. It is also prescribed local and general antibacterial, hyposinsebilizating and anti-inflammatory therapy.
The chronic maxillary sinusitis often enough proceeds as initially-chronic inflammatory process.
The clinical picture of chronic odontogenic maxillary sinusitis is characterized by: a headache, heavy feeling in the maxilla with prevailing localization in the infraorbital area, passage of air or passage of a liquid from the oral cavity into the nasal one (at the closed forms), discharges from the fistula, discharges from the nose, presence of a causal tooth. It is typical to reveal the sinus opacity on the X-ray with primary localisation process in the bottom part of the sinus.
For making diagnosis we could use:
- X-ray examination including panoramic films.
- Electoodontodiagnostics.
- Endoskopic research of sinus.
- Spiral or cone-beam computer tomography.
It is necessary to differentiate odontogenic maxillary sinusitis follows with radix and other cyst, grown into the sinus (presence of a shadow, like a dome on the roentgenogram), malignant tumours. Maxillary sinusitis also can be accompanied with an odontogenic osteomyelitis, acting thus as its symptom. The treatment of chronic odontogenic maxillary sinusitis is similar. In inefficiency of conservative treatment, we have to provide the surgical one.
Surgical treatment is performed by the following operative approaches:
- Caldwell – Luc (Fig. 12.16).
- Wasmund – Neumann – Zaslavsky (a Figured incision with access to an alveolar shoot with possibility of plastic elimination of fistula).
- Evdokimov – apertures in an anterior wall maxillary sinus.
- Parch – bow-shaped.
- Trapezoid Novak – Peteru.

Fig. 12.16. Opening of the maxillary sinus:
a – incision of mucus; b – forming of the trepanation opening; c – scheme of location of the maxillary sinus and trepanation opening (1 – foramen infraorbital; 2 – a lower nasoturbinal; 3 – lower nasal path; 4 – alveolar process of the maxilla; 5 – trepanation opening; 6 – maxillary sinus); d – connection of the sinus with a lower nasal path; e – scheme of this connection (7 – opening which connects a sinus with lower nasal path); f – incision in the area of lower nasal path (8 – incision of mucus of the nose; 9 – the area of nasoturbinal is remote)
Thus formation of following flaps is possible:
- Muco-periostal flaps.
- Muco-periostal-bone flaps (V. O. Malanchuk).
- Muco-periostal-bone-adiposal flaps (V. A. Sukachyov).
- Muco-periostal flaps from the pallet.
- The overturning muco-periostal flaps.
- Bridge flaps.
- Multilayered flaps with use of GTR technique.
In the case of perforation of the maxillary sinus, the area of connection of the sine through the oral cavity passes in development of a stage of the connection, a fistula (at the presence of granulations) and anatomizes (at the presence of epithelium).
Approaches to treatment can be the following:
I. Oneself closing: in the case of absence an artificial body in the maxillary sinus; after ending over of acute inflammatory process; in a case of absence of an aggravation of chronic inflammatory process, without presence of polyps and the pathologically changed mucosa.
II. Plastic elimination of communication without sinusotomia:
In the presence of a punched aperture or fistula in a course without an maxillary sinusitis; in chronic, but not polyp inflammatory process; in presence of fibrous changed mucous membrane that probably can be assessed by endoscopic devices.
III. Plastic closing with sinusotomia, without formation of unnatural communication: after conservative treatment in removal of only changed mucous membrane; in endoscopical revision for estimation of a sinus – in the presence of single polyps
IV. Radical sinusotomia with formation of unnatural communication.
- At polypous changed mucousa in the maxillary sinus.
- Along with punching or presence of an foriegn body in a sinus (a root in maxillary sinus).
Sialadenitis
Sialadenitis means inflammatory processes involving the salivary glands. The process may be acute and may result in an abscess formation particularly as a result of bacterial infection. The involvement can be unilateral or bilateral as in viral infections.
Chronic sialadenitis may be nonspecific resulting from ductal obstruction due to sialolithiasis or external radiation or may be specific, caused by various infectious agents and immunologic disorders. The ductal obstruction or decreased salivary flow, allowing retrograde spread of bacteria throughout the ductal system. Blockage of the duct can be caused by sialolithiasis, congenital strictures, or compression by an adjacent tumor.
Etiology
Inflamation of the salivary glands (sialadenitis) can arise from various infectious and noninfectious causes. One of the more common causes of sialadenitis is recent surgery (especially abdominal surgery), after which an acute parotitis (surgical mumps) may arise because the patient has been kept without food or fluids and has received atropine during the surgical procedure. Other medications that produce xerostomia as a side effect also can predispose patients to such an infection. Most cases of acute bacterial sialadenitis are due to Stapfylococcus aureus, but they also may arise from streptococci or other organisms. Noninfectious causes of salivary inflammation include Sjogren syndrome, sarcoidosis, radiation therapy and various allergens.
The most common viral infection is mumps, although a number of other viruses also can involve the salivary glands, including Coxsackie A. ECHO, choriomeningitis, parainfluenza, and cyiomegalovirus (in neonates).
It may be subdivided temporally into acute, chronic and recurrent forms.
Clinical and radiographic features mumps (epidemic parotitis)
Mumps is a paramyxovirus infection that primarily affects the salivary glands. As with measles and rubella, the epidemiology has been affected dramatically by the MMR vaccine (measles-mumps-rubella vaccine). Before the advent of widespread vaccination, epidemics were seen every 2 to 5 years. Although most authorities assume that natural infection is associated with lifelong immunity, rare cases of recurrent mumps have been well documented in patients with a confirmed history of prior natural infection.
The mumps virus can be transmitted through urine, saliva, or respiratory droplets. The Incubation period usually is 16 to 18 days, with a range of about 2 to 4 weeks. Patients are contagious from 1 day before the clinical appearance of infection to 14 days after its clinical resolution.
Approximately 30 % of mumps infections are subclinical. In symptomatic cases, prodromal symptoms of low-grade fever, headache, malaise, anorexia, and myalgia arrive first. Most frequently, these nonspecific findings are followed within 1 day by significant salivary gland changes. The parotid gland is involved most frequently, but the sublingual and submandibular glands also can be affected. Discomfort and swelling develop in the tissues surrounding the lower half of the external ear and extending down along the posterior inferior border of the adjacent mandible. The enlargement typically peaks within 2 to 3 days, and the pain is most intense during this period of maximal enlargement. Chewing movements of the jaw or eating saliva-stimulating foods tends to increase the pain. Enlargement of the glands usually begins on one side and is followed by contralateral glandular changes within a few days. Unilateral involvement is seen in about 25 % of patients.
The second most common finding is epididymoorchitis, which occurs in about 25 % of postpubertal males, in those affected, the testicle exhibits rapid swelling with significant pain and tenderness. The enlargement can range from a minimal swelling to a fourfold increase In size. Unilateral involvement is most common. On resolution of the swelling, atrophy occurs in the affected testicle. Permanent sterility from testicular changes is rare. Less commonly, oophoritis and mastitis can be seen in postpubertal females. In addition, spontaneous abortion occurs In approximately 25 % of females who contract mumps during the first trimester of pregnancy.
Less commonly, meningoencephalitis, cerebellar ataxia, hearing loss, pancreatitis, arthritis, carditis, and decreased renal function may occur. Isolated changes such as orchllis or meningitis, may occur in the absence of salivary gland involvement, thereby making diagnosis difficult in nonepidemic settings. Mumps-related mortality is exceedingly rare and most frequently associated with mumps encephalitis.
The most frequently reported oral manifestation is redness and enlargement of Wharton’s and Stenson’s salivary gland duct openings. In addition, involvement of the sublingual gland may produce bilateral enlargements of the floor of the mouth.
The diagnosis of mumps can be made easily from the clinical presentation when the infection is occurring in an epidemic fashion; however. Isolated cases must be differentiated from other causes. Saliva, urine, or cerebrospinal fluid specimens can be obtained for culture.
The most frequently used confirmatory measures are demonstration of mumps-specific IgM or a fourfold rise of mumps-specific IgG titers when measured during the acute phase and about 2 weeks later.
Acute bacterial sialadenitis is most common in the parotid gland and is bilateral in 10 % to 25 % of cases. The affected gland is swollen and painful, and the overlying skin may be erythematous (Fig. 12.17). An associated low-grade fever may be present, as well as trismus.

Fig. 12.17. Sialadenitis. Tender swelling of the submandibular gland
A purulent discharge often is observed from the duct orifice when the gland is massaged (Fig. 12.18).

Fig. 12.18. Sialadenitis. A purulent exudate arising from Stensen’s duct
Recurrent or persistent ductal obstruction (most commonly caused by sialoliths) can lead to a chronic sialadenitis. Periodic swelling and pain occur within the affected gland, usually developing at mealtime when salivary flow is stimulated, unilateral, duct orifice is reddened and flow decreases, may or may not have visible/palpable stone. Depends on ethiology and pathogenesis, sialography demonstrates various types of changes either ductal or parenchyma gland’s tissue (Fig. 12.19; 12.20; 12.21).

Fig. 12.19. Chronic sialadenitis

Fig. 12.20. Chronic sialadenitis
(interstitial form)

Fig. 12.21. Chronic sialadenitis (parenchymatous form)
Parotid sialogram demonstrating ductal dilatation proximal to an area of obstruction
In the submandibular gland, persistent enlargement may occur (Kuttner tumor), which is difficult to distinguish from a true neoplasm. Chronic sialadenitis also can occur in the minor glands, possibly as a result of blockage of ductal flow or local trauma. Subacute necrotizing sialadenitis is a recently recognized form of salivary inflammation that occurs most commonly in teenagers and young adults. The lesion usually involves the minor salivary glands of the hard or soil palate, presenting as a painful nodule that is covered by intact, erythematous mucosa. Unlike necrotizing sialometaplasia, the lesion does not ulcerate or slough necrotic tissue. An infectious or allergic cause has been hypothesized.
Histopathologic features in patients with acute sialadenitis, accumulation of neutrophils is observed within the ductal system and acini. Chronic sialadenitis is characterized by scattered or patchy infiltration of the salivary parenchyma by lymphocytes and plasma cells. Atrophy of the acini is common, as is ductal dilatation. If associated fibrosis is present, the term chronic sclerosing sialadenitis is used (Fig. 12.22).

Fig. 12.22. Chronic sclerosing sialadenitis. Chronic inflammatory infiltrate with associated acinar atrophy, ductal dilatation, and fibrosis
Subacute necrotizing sialadenitis is characterized by a heavy mixed inflammatory infiltrate consisting of neutrophils, lymphocytes, histiocytes, and eosinophils. There is loss of most of the acinar cells, and many of the remaining ones exhibit necrosis. The ducts tend to be atrophic and do not show hyperplasia or squamous metaplasia. Chronic sialadenitis has been misinterpreted as other non-neoplastic entities and also overcalled as several different types of neoplasms, both benign and malignant (Table 12.2).
Table 12.2. Differential Diagnosis of Chronic Sialadenitis
| A. Non-neoplastic |
B. Neoplastic |
| Mucocele, mucus retention cyst Benign lymphoepithelial cyst Benign lymphoepithelial lesion Intraparotid lymph node Amylodosis |
Warthin’s tumor Pleomorphic adenoma Low-grade adenocarcinoma, NOS Adenoid cystic carcinoma Mucoepidermoid carcinoma Acinic cell carcinoma |
Treatment and Prognosis
The treatment of acute sialadenitis includes appropriate antibiotic therapy against S. aureus (eg, oxacillin, 250 mg, a 1st-generation cephalosporin, or clindamycin), modified according to culture results. With the increasing prevalence of methicillin-resistant S. aureus, especially among the elderly living in extended-care nursing facilities, vancomycin is often required and hydration, sialagogues (eg, lemon juice, hard candy, or some other substance that triggers saliva flow), warm compresses, compress with 10 % Dimeksid, gland massage, and good oral hygiene are also important. Surgical drainage may be needed if there is abscess formation. Although this regimen is usually sufficient, a 20 % to 50 % mortality rate has been reported in debilitated patients because of the spread of the infection and sepsis.
The management of chronic sialadenitis depends on the severity and duration of the condition. Early cases that develop secondary to ductal blockage may respond to removal of the sialolith or other obstruction. If sialectasia is present, the dilated ducts can lead to stasis of secretions and predispose the gland to further sialolith formation, if sufficient inflammatory destruction of the salivary tissue has occurred, surgical removal of the affected gland may be necessary.
Subacute necrotizing sialadenitis is a self-limiting condition that usually resolves within 2 weeks of diagnosis without treatment.
The treatment of mumps is palliative in nature. Frequently, nonaspirin analgesics and antipyretics are administered. In an attempt to minimize orchitis, bed rest is recommended for males until the fever breaks. Avoidance of sour foods and drinks helps to decrease the salivary gland discomfort. As with measles and rubella, the best results come from prior vaccination, thereby preventing the infection.
Physiotherapeutic procedures for treatment chronic forms of the sialadenitis consists of: magnet-therapy, UHF (ultrahigh frequencies), ultrasound, electrophoresis (hydrocortisone 0.25 %, trypsin 0.01). Gland massage – 2–3 times a day, everyday.
Arthtritis
Arthritis can occur in a chronic, low-grade form or an acute inflammatory form. In addition, it can occur as a degenerative condition, associated with either overuse or aging, or it can occur as an autoimmune disease, such as juvenile rheumatoid arthritis. Most cases are chronic degenerative joint disease and are successfully treated with non-surgical management. The cartilage of the jaw is specifically designed to absorb and cushion the stress associated with movement and chewing. In some patients, the cartilage may lose its elasticity and become stiff. This can occur due to premature aging of the joint or as a result of overuse, such as a patient who grinds their teeth.
Infectious arthritis: Infection of the TMJ may result from direct extension of adjacent infection or hematogenous spread of bloodborne organisms. The area is inflamed, and jaw movement is limited. Local signs of infection associated with evidence of a systemic disease or with an adjacent infection suggest the diagnosis. X-ray results are negative in the early stages but may show bone destruction later. If suppurative arthritis is suspected, the joint is aspirated to confirm the diagnosis and to identify the causative organism. Diagnosis must be made rapidly to prevent permanent joint damage.
Treatment includes antibiotics, proper hydration, pain control, and motion restriction. Parenteral penicillin, ampicillin, ceftriakson are the drugs of choice until a specific bacteriologic diagnosis can be made on the basis of culture and sensitivity testing. Suppurative infections are aspirated or incised. Once the infection is controlled, jaw-opening exercises help prevent scarring and limitation of motion.
Traumatic arthritis. Rarely, acute injury (e.g., due to difficult tooth extraction or endotracheal intubation) may lead to arthritis of the TMJ. Pain, tenderness, and limitation of motion occur. Diagnosis is based primarily on history. X-ray results are negative except when intra-articular edema or hemorrhage widens the joint space. Treatment includes NSAIDs, application of heat, a soft diet, and restriction ofjaw movement.
Osteoarthritis. The TMJ may be affected, usually in people > 50 yr. Occasionally, patients complain of stiffness, grating, or mild pain. Crepitus results from a hole worn through the disk, causing bone to grate on bone. Joint involvement is generally bilateral. X-rays or CT may show flattening and lipping of the condyle, suggestive of dysfunctional change. Treatment is symptomatic.
Rheumatoid arthritis. The TMJ is affected in > 17 % of adults and children with RA, but it is usually among the last joints involved. Pain, swelling, and limited movement are the most common findings. In children, destruction of the condyle results in mandibular growth disturbance and facial deformity. Ankylosis may follow. X-rays of the TMJ are usually negative in early stages but later show bone destruction, which may result in an anterior open-bite deformity. The diagnosis is suggested by TMJ inflammation associated with polyarthritis and is confirmed by other findings typical of the disease.
Treatment is similar to that of RA in other joints. In the acute stage, NSAIDs may be given, and jaw function should be restricted. A night guard or splint is often helpful. When symptoms subside, mild jaw exercises help prevent excessive loss of motion. Surgery is necessary if ankylosis develops but should not be done until the condition is quiescent.
For children who suffer from chronic arthritis, there are challenges of daily living that are associated with decreased range of motion, pain and inflammation. For many children, the complications of arthritis extend well beyond that of the arms, legs, feet, and hands, and even include the joints in the face, including the temporomandibular joint, TMJ. Children who suffer from complications associated with juvenile rheumatoid arthritis often develop complications involving pain when feeding. This pain is associated with arthritic complications in the TMJ. While some TMJ pain can be associated with infection in and around the mouth, most children experience the complication of feeding in direct response to the arthritic and associated arthritic effusions.
If child is complaining of pain in and around the jaw, or TMJ, and complications associated with feeding are becoming apparent, ask your child’s physician to run the diagnostic studies to determine if the complication is related to the development of arthritis in the temporomandibular joint. MRI is often the diagnostic tool used to confirm the development of arthritic conditions in children. With MRI of the head, your child’s complications of pain in the temporomandibular joint can also be confirmed.
Degenerative arthritis
Degenerative arthritis can be either primary or secondary. Primary disease is seen in old people and is a disease of wear and tear. Patients are usually asymptomatic, and when symptomatic, the complaints are usually mild. Secondary degenerative arthritis: This type of arthritis usually develops in people aged 20 to 40 after trauma or in people with persistent myofascial pain syndrome. When degenerative arthritis occurs, the cartilage may then splinter and fracture. Once this occurs, the joint will gradually become stiff and painful. The patient will often hear noise or grinding in the joint and may feel roughness or grating. Joint noise indicates that the cartilage and the disk are beginning to lose their normal smooth contour. Pain in the joint often indicates progression of the disease leading to destruction of the joint components. It is characterized by limited opening of the mouth, unilateral pain during jaw movement, joint tenderness, and crepitus. When it is associated with the myofascial pain syndrome, symptoms wax and wane. Diagnosis is based on X-rays, which generally show condylar flattening, lipping of the joint with osteophyte formation, spurring, or erosion of the articular surface of the condyle. Unilateral joint involvement helps distinguish secondary degenerative arthritis from osteoarthritis.
Treatment of degenerative arthritis is similar to that of myofascial disorders and early internal derangements. NSAIDs, such as ibuprofen, and muscle relaxers with a soft diet are the primary treatment. Bite appliances are added as necessary. When conservative medical management fails to improve symptoms after a 3–6 month trial, surgery is considered. Surgical intervation includes removal of any surgical capsular abnormality, including osteophytes, until the joint space is smooth. A condylar shave is when the entire cortical plate is removed. It should be avoided if possible, as resorption of the condyle is a known complication.
Physical findings which support an initial diagnosis of temporomandibular arthralgia include:
Complete absence of molar teeth in any one quadrant.
Deviation of the jaw to the painful side on wide opening.
Reproducibility of the pain by pressure below the ear forward in the direction of the mandibular condyle.
Reproducibility of the pain by pressure from within the membraneous ear canal forward in the direction of the mandibular condyle, typically by reversing a laryngeal mirror and pressing with the round end of the handle in the ear canal.
Reproducibility of the patient’s complaint of “ear pain” by inserting two tongue blades between the opposite molars and instructing the patient to bite down hard on the tongue blades.
Diagnosis
There are two elements to diagnosis. The first is a comprehensive history and clinical examination. The second is a series of diagnostic studies.
In general, the diagnostic studies available for TM Joint diagnosis and evaluation are:
- X-rays of the TM Joints Skull.
- MRI (Magnetic Resonance Imaging).
- Computed tomography.
- Electromyography (studies of muscle function).
- Motion Performance Studies.
- Joint Vibration Analysis (a form of ultra-sound sonography).
- Diagnostic Study Casts of the Mandible Maxilla.
- X-rays of the Dentition.
Lymphadenites of maxillofacial area and a neck
Lymphadenitis is an inflammation of lymph nodes (Fig. 12.23), often combined with inflammation of lymph vessels.

Fig. 12.23. The lymph nodes of the maxillofacial area and neck
Lympadenites in submaxillary and mental areas as well as in the area of a neck can be characterized as odontogenic or non-odontogenic inflammatory processes. Odontogenic inflammatory processes in a periodontium, bones of a face, maxillary sinus, soft tissue of a face and an oral cavity inevitably result in penetration of infection to respective regional lymph nodes: submaxillary, mental, cheek, parotid, neck. As a result symptomatic lymphadenites develop in the aboved mentioned nodes and both nonspecific and specific lymphadenites can occur.
Acute attack of chronic periodontitis, periostitis and acute pericoronitis were considered to be the most frequent reasons of lymphadenitis. Serous inflammation of a lymph node usually developed on 1–3 day of primary disease while purulent fusion more often was observed on 3–6 day. It is noted that pathological process in primary odontogenic lesion can be curable while the inflammatory occurrences in regional lymph node continue to increase.
Acute odontogenic lymphadenites have been connected with pathological changes in the region of molar teeth and premolar teeth of lower jaw, less often – molar teeth and lateral cutters of the upper jaw. It caused more frequent affect of submandibular ganglion, submental, cheek and parotid lymph nodes, having been major collectors of lymph outflow from mentioned sites of lesion. Usually one lymph node was involved in inflammatory process, the increase in two region nodes areas wasn’t often observed.
Group of non-odontogenic lymphadenites comprises those which have no pathogenetic relation with the dental-maxillary system. They are so-called stomatogenic, rhinogenous, otogenous and other symptomatic lymphadenites, developing due to stomatites, gingivites, glossites, rhinites, inflammatory diseases of an ear. Regional lymphadenites quite often arise in connection with more or less expressed damage of skin or the mucous membrane of the mouth: at a site trauma an entrance gate for an infection are created.
Classification of the lymphadenitis including such forms: acute; serous; purulent; chronic; exudative; productive; traumatic; odontogenic; nonodontogenic; Infectious – Non-specific (acute, chronic); Specific (tuberculous; syphilitic; actinomycotic; viral; vaccinal).
Acute lymphadenitis
Acute inflammation begins with feeling of some awkwardness at head motion, pain in the area of the injured node or groups of nodes.
Both in serous and hyperplastic forms increased lymph nodes are well determined by palpation and under such conditions they are a little bit painful and have dense-elastic consistency. General disorders at the beginning of an inflammation can be absent or be of low-grade. The serous inflammation seldom turns into purulent process; it gradually calms down in compliance with the efficacy of the treatment of the underlying disease which has caused an inflammation of lymphatic vessels and regional nodes. The nodes gradually decrease in sizes, become less painful in some weeks, have usual form and a consistency. At adverse course of serous inflammation it can turn into purulent: in the field of the node infiltration appears (perilymphadenitis), the node becomes not mobile, commissures with other nodes forming with them a package, suppurates. The body temperature raises up to 37.2–37.8 °C. As for blood, there are changes characteristic for abscesses. The general state of health and of the patient is quite often abnormal: indisposition, weakness, loss of appetite, etc. Inflamed lymph node gradually fuses and causes formation of the sinus tract (with transition of disease into the chronic form) or adenophlegmon (see below). In acute purulent lymphadenitis its general parameters (changes in blood, urine, temperature reaction) can be shaded and can be explained as changes due to underlying odontogenic or nonodontogenic inflammation caused lymphadenitis.
Process of purulent fusion of the node can develop quickly – within several days, but sometimes slowly even after elimination of the underlying process on the face, the jaw and in the oral cavity. In the maxillofacial area the most often lymphadenites are those in submandibular nodes as they are the major nodes of the first stage on the way of lymphatic outflow from the given area. The second by frequency of occurrence are inflammatory processes in mental as well as in parotid and supramaxillar (buccal) nodes. Odontogenic lymphadenites developing on the background of acute or chronic leucosis usually have plural character, locating simultaneously on the face, in the submaxillary areas and the neck. In odontogenic source of infection localized on one side, lymphadenitis can be bilateral as in leucosis all protective immunologic mechanisms are significantly lowered.
Chronic lymphadenitis
Chronic nonspecific lymphadenitis develops as a result of attenuation of the acute process or it is caused by poorly virulent microorganisms. It is characterized by enlargement of lymph nodes to various sizes and restriction of their motion. Separate, clearly determined nodes, painless, but dense enough are palpated. The general state of health of a patient usually is not disordered. The purulence of lymph nodes in chronic nonspecific inflammation occurs seldom; it is a feature of transition of chronic process to the acute due to the flare-up of a dormant infection. If odontogenic or other source of infection “bombards” node during a long period of time, it is gradually decaying during a chronic inflammation and is replaced by granulation tissue; from time to time there are aggravations; the latter finally lead to skin perforation and formation of a fistula which is closed and cicatrizes with time. Then beside a fistula appears.
Chronic specific lymphadenitis has, as a rule, tubercular or actinomycotic ethiology and affects mandibular, submandibular, retromandibular and cervical nodes. Sometimes it is combined with injury of other lymph nodes of a body, including bronchial both retroperitoneal. Tubercular and actinomycotic chronic lymphadenites initially have similar courses, creating a picture of so-called hypodermic migrating granuloma of a face or mandibular area. Later actinomycotic lymphadenitis differs by greater tendency to suppuration and formation of fistulas. Course of tubercular lymphadenitis is variable and depends on a stage of disease, amount of injured lymph nodes, reactions of tissues surrounding a node, etc.
It is important to determine first of all, whether lymphadenitis is banal or specific.
In this connection it should be taken into account, that tubercular lymphadenitis is characterized by the absence of the inflammatory features in the oral cavity, jaws, face; rather slow and quite often bilateral increase of inflammatory process in lymph nodes, prolonged mild pyrexia, positive Mantoux test, sterility of pus obtained during a puncture. If chronic lymphadenitis has syphilitic ethiology, thus in the anamnesis or the objective status there are proofs of this disease (Wassermann test, availability of specific destructions of the nose, palate, soft tissue in the area of the pharynx, etc.).
The diagnosis actinomycosis of lymph nodes is determined on the basis of the characteristic anamnesis, infiltrate density, immunoreactions, findings of pathologo-histological or cytological examinations.
Differences between adenophlegmon and lymphadenitis include more extensive area of injury, skin tension and more expressed general disorders (see below).
Sialoadenitis (inflammation of parotid or submandibular salivary gland) is characterized by purulent or serous-purulent discharge from the efferent duct of the gland. If in chronic lymphadenitis there is infiltrate tuberosity, it is necessary to exclude a neoplasm. In such cases biopsy is indicated.
Syphilitic injury of a node is characterized by its significant induration and availability of corresponding findings and the objective status in anamnesis (see above).
Brill-symmers disease or giant follicular lymphoma is one of benign variants of lymphosarcomas. For many years it can represent asymptomatic increase of parotid, submandibular, mental lymph nodes, dense by touch and by that supposing chronic nonspecific lymphadenitis or reactive follicular hyperplasia.
Giant follicular lymphoma (known also as medullar lymphosarcoma by WHO classification 1976) is diagnosed only by histologic study. As in this disease occurs generalization (injury of the nearby and remote lymph nodes with involving of the skin, a hypodermic layer, tonsils, internal organs, bone marrow), it is necessary to not hesitate with radical removal of palpated nodes and their careful histological examination.
Differential diagnostics of LAP (lymphoadenopaties)
Local (regional) LAP:
- Local infections bacterial (pharyngitis, mild otitis, ethmoiditis, frontitis, an antritis, an abscess and caries of teeth).
- Viral (disease of “the cat’s scratch”, a tuberculosis, children’s infections, etc.).
- Fungous (actyinomycaosis, candidiasis) lymphogranulematosis (Hodgkin’s disease).
- Non-Hodgkin’s lymphomas (lymphoma of tonsiles, LN).
- Carcinoma (secondary).
Generalized (systemic) LAP:
- Infections bacterial (sepsis, tuberculosis, brucellosis, tularemia, syphilis, etc.); viral (measles, adenoviral infection, flu, AIDS, infectious mononucleosis etc.) fungoid (histoplasmosis, actinomycosis) protozoan (toxoplasmosis, listeriosis, leishmanioisis).
- Autoimmune diseases (rheumatoid arthritis, systemic red erythematosus, dermatomyositis, sclerodermia, nodular periarteritis, granulematous arterites, etc.).
- Benign tumor diseases (sinus histiocytosis with massive LAP, associated with infections, hemophagocytic syndrome, sarcoidosis).
- Malignant tumor diseases primary: LGM (Hodgkin’s disease). Non-Hodgkin’s disease (lymphoma of peripheral LN, skin lymphoma, malignant histiocytoses; metastatic: leukemia, neuroblastoma, rhabdomyosarcoma. Kaposi’s sarcoma, cancers of the lungs, bronchus and thyroid gland.
- Storage diseases (Gaucher’s disease, Niemann – Pick disease).
- Reactions to medicinal and chemical substances (serum sickness, medicamentous allergy, pollinosis).
- Other diseases.
Treatment
Treatment of acute serous and chronic lymphadenites should be conservative only when it is impossible to define a source (an entrance gate) of infection in the oral cavity, teeth, jaws, face, ENT-organs, etc. In such cases there are applied: dry heat, UHF-therapy, short-term novocaine-antibitics blockade. For the treatment of acute serous lymphadenitis inflammatory infiltrates A. A. Timofeev (1989) recommends daily novocaine nerve-blockade for 5 days of superior cervical and stellate sympathetic ganglions on a side of injury and after dissection of purulent lymphadenites – intramuscular infusion of the Lysozyme (200 mg 2 times a day on first three days, 100 mg 2 times a day the next 3 days) without combination with antibiotics. Blockades are useful because sympathetic fibres of cervical ganglions innervate smooth muscule elements being in a capsule and trabeculas of lymph nodes of the maxillofacial area and the neck that provides contraction of the latter and promotes pushing through of lymph to revehent vessels. In the inflammatory area nervous fibres are in a state of parabiosis the rate of which depends on the severity of the inflammatory process. Novocaine has antiparabiotic property.
It is very useful to apply warming compresses with 30 % solution of dimethylsulfoxide. If the source of infection is not revealed and suppuration of a node (or a package of nodes) occured, it is necessary to dissect the abscess and drain it. In some cases it is possible to manage with aspiration of pus and filling of the cavity of an abscess with a solution of antibiotics. If the source of an infection is revealed, it is necessary to eliminate it with antibacterial preparations or surgical intervention (removal of tooth with periodontitis, husking of festered cyst, removal of hanging inflamed hood above cutting tooth, treatment of antritis, osteomyelitis, periostitis, etc.).
If there is interrelation between suppurated lymph node and odontogenic source of an infection, it is as usually enough to eliminate the latter to stop lymphadenitis or perilymphadenitis. However, in some cases besides intervention on a tooth (its removal, replantation, apical resection etc.) it is necessary to do an incision throughout the mucogingival fold to dissect granular-inflammatory bundle from a tooth to the focus of suppuration in soft tissue. An incision throughout mucogingival fold is drained by rubber strip. As a result, entry of new portions of infection from dental-maxillary systems completely stops. If lymph node suppuration resulted in destruction and cicatricial deformation of the skin, it is necessary to dissect cicatrical changes of tissue, to remove whole granulation tissue both in the depth of the focus of injury and on the internal surface of the dissected skin, to rinse the wound and layer by layer to take it in.
Specific tubercular lymphadenitis should be treated in specialized medical establishments. Sanitation of the oral cavity is obligatory. Immunotherapy is successful for adenoactinomycosis as well as hypodermic form of actinomycotic injuries of the face and the neck; in case of lymph nodal suppuration dissection of the focus, scraping of granulations and administration of antibiotics (locally and intramuscularly) is indicated. However, it is necessary to remember, that a source of a specific infection quite often is gangrenous tooth. Therefore the treatment of specific lymphadenitis should be started with sanitation of the oral cavity.
Prevention of acute sharp and chronic limphadenitis consists of general and local anticarious actions: duly treatment of caries of teeth and its complications, elimination of non-odontogenic sources of infection (treatment of stomatitis, rhinitis, gingivitis, glossitis, otitis, furuncules, carbuncules, etc.), treatment of traumatic injuries of the mucous membrane of a mouth and skin of face, increase of resistance of human organism, etc.
Specific inflammatory processes
Actinomycosis, tuberculosis, syphilis: etiology, classification, clinical course, diagnostics, treatment.
Tuberculosis (tbc.)
Mycobacterium Tbc. (human – 92 %, bovine – 5 %, intermediate – 3 %).
Droplet type of transfer, contact, alimentary factor. Immunity and firmness of an organism to Tbc, premobid background, social conditions of a life of the patient. Tbc. bacilli are partially persist in a place of penetration, the others – are transferred by a current of a lymph to the nearest lymph nodes. Further duplication of microbacilli takes and granuloma is formed – Tbc tubercule. Tubercule (Tbc) decays with formation of the cheesy decay focus 4–8 weeks after an organism sensitizes to tuberculoprotein.
Tbc can affect any human system or organ, remaining thus systemic disease.
Tbc of the maxillofacial area can be primary, when there is no pulmonary focus and secondary – when active Tbc process occurs in lung, bones, etc.
Clinic
Tbc. injury of the maxillofacial area includes injuries of the skin, mucous membranes, hypodermic cellular tissue, jaws, lymph nodes and salivary glands.
Primary Tbc injury is usually formed in the region of lymph nodes amounts up to 60 %.
Classification including:
Hyperplastic (infiltrative) form – Tbc granulomas against the background of lymphoid tissue proliferation. Fibrous-cheesy form – cheesy necrosis numerous combined Tbc granulomas. Fibrous – cicatricial hardenings, development of a connecting fabric.
- Tbc of jaws – secondary, with mucous, in hematogenous spread (lymphogenous) spread, Ro – in a jaw foci of exhaustion take place.
- Tbc of salivary glands are rare, often in parotid, foci of necrosis appear.
- Tbc of skin and hypodermic cellular tissue:
Primary Tbc (Tbc chancre) – erosion and ulcers with harden bottom; Tbc lupus – Tbc tubercule (lipoma) soft; scrofuloderma – intrascutaneous nodes sized 1–3 cm, dense; lupus verucosis Tbc – small, dense, painless node of pinkish-cyanotic color; milliary-ulcer Tbc – small yellowy-red nodes, ulcerating conjugate and superficial very painful ulcers are formed; disseminated milliary Tbc (milliary lupus) – small nodes are painless, they are ulcering, cicatrize or resolve; roseola tuberculitis – pinkish-brown papulae with drying up crusts; papulo-necrotic Tbc – small roundish paulae (2–3 mm).
Treatment
Dissection of the purulent foci,biopsy (incisional, excisional), sequestectomy, etc. Sanitation of the oral cavity. Systemivc treatment: PAS(A), phtivazid, rifampicin.
Syphilis (LuES)
It is caused by pale treponema. A venereal and domestic way of transmission.
It can be congenital, a superinfection – pale treponemas get into an organism (repeated infection of not cured patient) – overlay of syphilitic infection on the already available ones, clinically – erupt during the period when repeated infection occured.
Clinic consist of the primary, secondary and tertiary periods.
The incubatory period is 3 weeks and is completed with formation of primary syphiloma. Primary – a spot of red color or papulae – in the center is necrosis – an ulcer (hard chanre), 5–7 days after enlargement of regional lymph nodes – syphilitic scleradenitis 3–4 weeks after – polyadenitis painless.
Seronegative and seropositive period 6–7 weeks later.
Secondary – occurrence of roseolas, papulae, pustules (syphilides) on the skin and mucous membrane.During this period the greatest contagiosa occures. Sometimes periosteum is injured, more often on the lower jaw, thickening.
The tertiary period occurs 3–6 years later and is characterized by grumous tubercle and gummatous formations. In tubercle syphilide in dermal thickness rounded dense raised formation are detected.
Formation of grumous infiltrate, necrosis, ulcers is possible. Gumma is a painless node densely elastic consistence up to 1.5 mm in diameter, contains viscous substance – a deep ulcer, cicatrizes slowly – deformed scars. They are in the region of hard and soft palates in the thickness of the tongue, the back wall of the throat, the nose, frequently in nasal septum. Foraminous defects in bone are formed.
Dental treatment includes the following stages: antiseptic care of syphilitic elements. Sanitation of teeth.Surgical treatment of deformations after the performed course of treatment.
Actinomicosis
Radiant-fungoid diseases – is ray fungus. In 85 % maxillofacial area is affected. Ray fungus – saprophyte, mainly in stroma of dental calculus.
The entrance gate of an infection – carious teeth, pathological dentalgingival pockets, the mucous membrane of the oral cavity, pharynx, nose, throat, salivary glands. The incubation period – from some days up to 2–3 weeks, but sometimes it can last for months. Ray fungus can develop in friable cellular tissue, in tissue layers of muscles and organs, i.e. in good vascularized environment. Specific granuloma is formed. Robustova distinguishes the following forms of actinomycosis of the face, neck, jaws and oral cavity: cutaneous; hypodermic; submucosal; mucous; odontogenic actinomycosis granuloma; hypodermical-intermuscular; actinomycosis of lymph nodes; actinomycosis of jaw periosteum; actinomycosis of jaws; atinomycosis of the oral cavity, tongue, tonsils, salivary glands, maxillary sinus.
The diagnosis is verified by analysis reaction:
1) - negative reaction – only a site of needle prick is visible;
2) ? doubtful reaction – hardly appreciable pink erythema;
3) +? poorly positive – clear erythema;
4) + positive reaction – brightly-pink erythema up to dark red color;
5) + + strongly positive reaction – brightly-red erythema with skin edema, painful;
6) + + + systemic or local reaction – systemic or focal changes.
Treatment may consist of surgical: removal of teeth – an entrance gate of infection; surgical processing of infection foci, removal of neoplastic bone. Influence on specific immunity; increase of general resistance of organism; influence on accompanying purulent infection; anti-inflammatory, desensibilizing, symptomatic treatment, treatment of concomitant diseases; physical methods and exercise therapy.
Complications of inflammatory processes of the maxillofacial region and neck
Sepsis
Sepsis is a serious medical condition characterized by a whole-body inflammatory state (called a systemic inflammatory response syndrome or SIRS) and the presence of a known or suspected infection. Septicemia is a related but deprecated (formerly sanctioned medical) term referring to the presence of pathogenic organisms in the blood-stream, leading to sepsis. Severe sepsis occurs when natural immune response to an infection goes into overdrive, triggering widespread inflammation and blood clotting in tiny vessels throughout the body. One or more organs may stop working properly or fail. Sepsis can lead to a dangerous drop in blood pressure (septic shock).
Sepsis is usually treated in the intensive care unit with intravenous fluids and antibiotics. If fluid replacement is insufficient to maintain blood pressure, specific vasopressor drugs can be used. Artificial ventilation and dialysis may be needed to support the function of the lungs and kidneys, respectively. To guide therapy, a central venous catheter and an arterial catheter may be placed. Sepsis patients require preventive measures for deep vein thrombosis, stress ulcers and pressure ulcers, unless other conditions prevent this. Some patients might benefit from tight control of blood sugar levels with insulin (targeting stress hyperglycemia), low-dose corticosteroids or activated drotrecogin alfa (recombinant protein C).
Severe sepsis occurs when sepsis leads to organ dysfunction, low blood pressure (hypotension), or insufficient blood flow (hypoperfusion) to one or more organs (causing, for example, lactic acidosis, decreased urine production, or altered mental status). Sepsis can lead to septic shock, multiple organ dysfunction syndrome (formerly known as multiple organ failure), and death. Organ dysfunction results from sepsis-induced hypotension (< 90 mm Hg or a reduction of > 40 mm Hg from baseline) and diffuse intravascular coagulation, among other things.
Bacteremia is the presence of viable bacteria in the bloodstream. These term says nothing about the consequences this has on the body. For example, bacteria can be introduced into the bloodstream during toothbrushing. This form of bacteremia almost never causes problems in normal individuals. However, bacteremia associated with certain dental procedures can cause bacterial infection of the heart valves (known as endocarditis) in high-risk patients. Conversely, a systemic inflammatory response syndrome can occur in patients without the presence of infection, for example in those with burns, polytrauma.
At higher risk for sepsis are:
- Very young people and elderly people.
- Anyone who is taking immunosuppressive medications (such as transplant recipients).
- People who are being treated with chemotherapy drugs or radiation.
- Patients who have no spleen.
- Patients taking steroids (especially over the long-term).
- People with long-standing diabetes, AIDS, or cirrhosis.
- Someone who has very large burns or severe injuries.
In addition to symptoms related to the provoking infection, sepsis is characterized by evidence of acute inflammation present throughout the entire body, and is, therefore, frequently associated with fever and elevated white blood cell count (leukocytosis) or low white blood cell count and lower-than-average temperature. The modern concept of sepsis is that the host’s immune response to the infection causes most of the symptoms of sepsis, resulting in hemodynamic consequences and damage to organs. This host response has been termed systemic inflammatory response syndrome (SIRS) and is characterized by hemodynamic compromise and resultant metabolic derangement. Outward physical symptoms of this response frequently include a high heart rate (above 90 beats per minute), high respiratory rate (above 20 breaths per minute), elevated WBC count (above 12G) and elevated or lowered body temperature (under 36 °C or over 38 °C). Sepsis is differentiated from SIRS by the presence of a known pathogen. For example, SIRS and a positive blood culture for a pathogen indicates the presence of sepsis. Without a known infection you can not classify the above symptoms as sepsis, only SIRS. This immunological response causes widespread activation of acute-phase proteins, affecting the complement system and the coagulation pathways, which then cause damage to the vasculature as well as to the organs. Various neuroendocrine counter-regulatory systems are then activated as well, often compounding the problem. Even with immediate and aggressive treatment, this may progress to multiple organ dysfunction syndrome and eventually death.
Definition of sepsis
Sepsis is considered present if infection is highly suspected or proven and two or more of the following systemic inflammatory response syndrome (SIRS) criteria are met:
- Heart rate > 90 beats per minute (tachycardia).
- Body temperature < 36 °C (97 °F) or > 38 °C (100 °F).
- Respiratory rate > 20 breaths per minute or, on blood gas, a PaCO2 less than 32 mm Hg (4.3 kPa) (tachypnea or hypocapnia due to hyperventilation).
- White blood cell count < 4.000 cells/mm3 or > 12,000 cells/mm3 (< 4 × 109 or > 12 × 109 cells/L), or greater than 10 % band forms (leukopenia, leukocytosis, or bandemia).
Fever and leukocytosis are features of the acute-phase reaction, while tachycardia is often the initial sign of hemodynamic compromise. Tachypnea may be related to the increased metabolic stress due to infection and inflammation, but may also be an ominous sign of inadequate perfusion resulting in the onset of anaerobic cellular metabolism.
To qualify as sepsis, there must be an infection suspected or proven (by culture, stain, or polymerase chain reaction (PCR)), or a clinical syndrome pathognomonic for infection.
The more critical subsets of sepsis are severe sepsis (sepsis with acute organ dysfunction) and septic shock (sepsis with refractory arterial hypotension). Patients are defined as having “severe sepsis” if they have sepsis plus signs of systemic hypoperfusion: either end-organ dysfunction or serum lactate greater than 4 mmol/dL. Other signs include oliguria and altered mental status. Patients are defined as having septic shock if they have sepsis plus hypotension after aggressive fluid resuscitation (typically upwards of 6 liters or 40 ml/kg of crystalloid).
Diagnosis
The medical history and clinical examination can provide important elements regarding the cause and severity of sepsis.
The identification of the causative microbe in sepsis can provide useful information. The exact causative organism is confirmed by microbiological culturing in the laboratory (blood cultures and cultures from suspected sites of infections). However, this is a slow process, as it takes a few days to grow up the cultures and correctly identify the pathogens. New molecular diagnostic tests are now available that use genetic material from the pathogen to quickly (within hours) provide results. However, current practice is to directly prescribe broad spectrum antibiotics to the patient.
The effects of the condition on the function of the organs should be documented to guide therapy. This can involve measurement of blood levels of lactate, blood gas sampling, and other blood tests. Because patients on the intensive-care unit are predisposed to hospital-acquired infections (especially related to the presence of catheters), they may require surveillance cultures.
Treatment
The therapy of sepsis rests on antibiotics, surgical drainage of infected fluid collections, fluid replacement and appropriate support for organ dysfunction. This may include hemodialysis in kidney failure, mechanical ventilation in pulmonary dysfunction, transfusion of blood products, and drug and fluid therapy for circulatory failure. Ensuring adequate nutrition – preferably by enteral feeding, but if necessary by parenteral nutrition – is important during prolonged illness.
During critical illness, a state of adrenal insufficiency and tissue resistance (the word “relative” resistance should be avoided to corticosteroids) may occur. This has been termed critical illness-related corticosteroid insufficiency. Treatment with corticosteroids might be most beneficial in those with septic shock and early severe acute respiratory distress syndrome (ARDS).
A number of different types of medications are used in treating sepsis, such as:
- Antibiotics. Treatment with antibiotics begins immediately – even before the infectious agent is identified. Initially “broad-spectrum” antibiotics are used, which are effective against a variety of bacteria. The antibiotics are administered intravenously (IV).
- Vasopressors. If the blood pressure remains too low even after receiving intravenous fluids, the patient may be given a vasopressor medication, which constricts blood vessels and helps to increase blood pressure.
- Activated protein C. People with severe sepsis whose organs are failing or who are at high risk of dying may receive a newer drug called activated protein C. This drug interferes with some of the body’s responses to severe infection, helping to curb the overactive inflammatory reaction, but it can cause serious bleeding.
- Others. Other medications include low doses of corticosteroids, insulin to help maintain stable blood sugar levels, and painkillers or sedatives.
People with severe sepsis usually receive supportive care. Depending on the condition, the patient may need mechanical ventilation (respirator) in case of breathing problems or dialysis for kidney failure.
Possible complications: death; disseminated intravascular coagulation; impaired blood flow to vital organs (brain, heart, kidneys); septic shock.
Mediastinitis
Mediastinitis is inflammation of the tissues in the midchest, or mediastinum. The mediastinum lies between the right and left pleura in and near the median sagittal plane of the chest. It extends from the sternum in front to the vertebral column behind, and contains all the thoracic viscera excepting the lungs.
Mediastinitis can be either acute or chronic. Acute mediastinitis is usually bacterial and due to rupture of organs in the mediastinum. As the infection can progress rapidly, this is considered a serious condition. Chronic sclerosing (or fibrosing) mediastinitis, while potentially serious, is caused by a long-standing inflammation of the mediastinum, leading to growth of acellular collagen and fibrous tissue within the chest and around the central vessels and airways. It has a different cause, treatment, and prognosis than acute infectious mediastinitis.
Before the development of modern cardiovascular surgery, cases of acute mediastinitis usually arose from either perforation of the esophagus or from contiguous spread of odontogenic or retropharyngeal infections. However, in modern practice, most cases of acute mediastinitis result from complications of cardiovascular or endoscopic surgical procedures.
Treatment usually involves aggressive intravenous antibiotic therapy and hydration. If discrete fluid collections (such as abscesses) have formed, they may have to be surgically drained. Chronic mediastinitis is usually a radiologic diagnosis manifested by diffuse fibrosis of the soft tissues of the mediastinum. This is sometimes the consequence of prior granulomatous disease, most commonly histoplasmosis. Other identifiable causes include tuberculosis and radiation therapy. Fibrosing mediastinitis most frequently causes problems by constricting blood vessels or airways in the mediastinum. This may result in such complications as superior vena cava syndrome or pulmonary edema from compression of pulmonary veins. Treatment for chronic fibrosing mediastinitis is somewhat controversial, and may include steroids or surgical decompression of affected vessels.
Meningitis
Meningitis is inflammation of the protective membranes covering the brain and spinal cord, known collectively as the meninges. The inflammation may be often caused by bacteria of odontogenic origin. Meningitis can be life-threatening because of the inflammation’s proximity to the brain and spinal cord; therefore the condition is classified as a medical emergency.
The most common symptoms of meningitis are headache and neck stiffness associated with fever, confusion or altered consciousness, vomiting, and an inability to tolerate light (photophobia) or loud noises (phonophobia).
A lumbar puncture may be used to diagnose or exclude meningitis. This involves inserting a needle into the spinal canal to extract a sample of cerebrospinal fluid (CSF), the fluid that envelops the brain and spinal cord. The CSF is then examined in a medical laboratory. The usual treatment for meningitis is the prompt application of antibiotics. In some situations, corticosteroid drugs can also be used to prevent complications from overactive inflammation. Meningitis can lead to serious long-term consequences such as deafness, epilepsy, hydrocephalus and cognitive deficits, especially if not treated quickly.
Clinical features
In adults, a severe headache is the most common symptom of meningitis – occurring in almost 90 % of cases of bacterial meningitis, followed by nuchal rigidity (inability to flex the neck forward passively due to increased neck muscle tone and stiffness). The classic triad of diagnostic signs consists of nuchal rigidity, sudden high fever, and altered mental status; however, all three features are present in only 44–46 % of all cases of bacterial meningitis. Other signs commonly associated with meningitis include photophobia (intolerance to bright light) and phonophobia (intolerance to loud noises).
Nuchal rigidity occurs in 70 % of adult cases of bacterial meningitis. Other signs of meningism include the presence of positive Kernig’s sign or Brudzinski’s sign. Kernig’s sign is assessed with the patient lying supine, with the hip and knee flexed to 90 degrees. In a patient with a positive Kernig’s sign, pain limits passive extension of the knee. A positive Brudzinski’s sign occurs when flexion of the neck causes involuntary flexion of the knee and hip. Although Kernig’s and Brudzinski’s signs are both commonly used to screen for meningitis, the sensitivity of these tests is limited. They do, however, have very good specificity for meningitis: the signs rarely occur in other diseases.
People with meningitis may develop additional problems in the early stages of their illness. These may require specific treatment, and sometimes indicate severe illness or worse prognosis. The infection may trigger sepsis, a systemic inflammatory response syndrome of falling blood pressure, fast heart rate, high or abnormally low temperature and rapid breathing. Disseminated intravascular coagulation, the excessive activation of blood clotting, may cause both the obstruction of blood flow to organs and a paradoxical increase of bleeding risk.
The brain tissue may swell, with increasing pressure inside the skull and a risk of swollen brain tissue getting trapped. This may be noticed by a decreasing level of consciousness, loss of the pupillary light reflex, and abnormal positioning. Inflammation of the brain tissue may also obstruct the normal flow of CSF around the brain (hydrocephalus).
The types of bacteria that cause bacterial meningitis vary by age group. In premature babies and newborns up to three months old, common causes are group B streptococci (subtypes III which normally inhabit the vagina and are mainly a cause during the first week of life) and those that normally inhabit the digestive tract such as Escherichia coli (carrying K1 antigen). Listeria monocytogenes (serotype IVb) may affect the newborn and occurs in epidemics. Older children are more commonly affected by Neisseria meningitidis (meningococcus), Streptococcus pneumoniae (serotypes 6, 9, 14, 18 and 23) and those under five by Haemophilus influenzae type B (in countries that do not offer vaccination). In adults, N. meningitidis and S. pneumoniae together cause 80 % of all cases of meningitis, with increased risk of L. monocytogenes in those over 50 years old.
In some proportion of people, an infection in the head and neck area lead to meningitis. Recent trauma to the skull gives bacteria in the nasal cavity the potential to enter the meningeal space. In these cases, infections with staphylococci are more likely, as well as infections by pseudomonas and other Gram-negative bacilli. The same pathogens are also more common in those with an impaired immune system.
Recurrent bacterial meningitis may be caused by persisting anatomical defects, either congenital or acquired, or by disorders of the immune system. Anatomical defects allow continuity between the external environment and the nervous system. The most common cause of recurrent meningitis is skull fracture, particularly fractures that affect the base of the brain or extend towards the sinuses and petrous pyramids.
Diagnosis
In someone suspected of having meningitis, blood tests are performed for markers of inflammation (e.g. C-reactive protein, complete blood count), as well as blood cultures.
The most important test in identifying or ruling out meningitis is analysis of the cerebrospinal fluid through lumbar puncture (LP, spinal tap). However, lumbar puncture is contraindicated if there is a mass in the brain (tumor or abscess) or the intracranial pressure (ICP) is elevated, as it may lead to brain herniation. CT or MRI scans are performed at a later stage to assess for complications of meningitis.
Treatment
Meningitis is potentially life-threatening and has a high mortality rate if untreated; delay in treatment has been associated with a poorer outcome. Thus treatment with wide-spectrum antibiotics should not be delayed while confirmatory tests are being conducted. Intravenous fluids should be administered if hypotension (low blood pressure) or shock is present. Given that meningitis can cause a number of early severe complications, regular medical review is recommended to identify these complications early, as well as admission to an intensive care unit if deemed necessary.
Mechanical ventilation may be needed if the level of consciousness is very low, or if there is evidence of respiratory failure. The structural formula of ceftriaxone, one of the third-generation cefalosporin antibiotics recommended for the initial treatment of bacterial meningitis.
Empiric antibiotics (treatment without exact diagnosis) must be started immediately, even before the results of the lumbar puncture and CSF analysis are known. The choice of initial treatment depends largely on the kind of bacteria that cause meningitis in a particular place.
The results of the CSF culture generally take longer to become available (24–48 hours). Once they do, empiric therapy may be switched to specific antibiotic therapy targeted to the specific causative organism and its sensitivities to antibiotics. For an antibiotic to be effective in meningitis, it must not only be active against the pathogenic bacterium, but also reach the meninges in adequate quantities; some antibiotics have inadequate penetrance and therefore have little use in meningitis.
Adjuvant treatment with corticosteroids (usually dexamethasone) reduces rates of mortality, severe hearing loss and neurological damage. The likely mechanism is suppression of overactive inflammation.
Prognosis
Untreated, bacterial meningitis is almost always fatal. With treatment, mortality (risk of death) from bacterial meningitis depends on the age of the patient and the underlying cause and is about 19–37 % in adults. Risk of death is predicted by various factors apart from age, such as the pathogen and the time it takes for the pathogen to be cleared from the cerebrospinal fluid, the severity of the generalized illness, decreased level of consciousness or abnormally low count of white blood cells in the CSF.
Cavernous sinus Thrombosis
Cavernous sinus thrombosis (CST) was initially described by Bright in 1831 as a complication of epidural and subdural infections. CST is usually a late complication of an infection of the central face or paranasal sinuses. Other causes include bacteremia, trauma, and infections of the ear or maxillary teeth. CST is generally a fulminant process with high rates of morbidity and mortality. Fortunately, the incidence of CST has been decreased greatly with the advent of effective antimicrobial agents.
Pathophysiology
The cavernous sinuses are irregularly shaped, trabeculated cavities located at the base of the skull. The cavernous sinuses are the most centrally located of the dural sinuses and lie on either side of the sella turcica. These sinuses are just lateral and superior to the sphenoid sinus and are immediately posterior to the optic chiasm. Each cavernous sinus is formed between layers of the dura mater, and multiple connections exist between the 2 sinuses.
The cavernous sinuses receive venous blood from the facial veins (via the superior and inferior ophthalmic veins) as well as the sphenoid and middle cerebral veins. They, in turn, empty into the inferior petrosal sinuses, then into the internal jugular veins and the sigmoid sinuses via the superior petrosal sinuses. This complex web of veins contains no valves; blood can flow in any direction depending on the prevailing pressure gradients. Since the cavernous sinuses receive blood via this distribution, infections of the face including the nose, tonsils, and orbits can spread easily by this route.
The internal carotid artery with its surrounding sympathetic plexus passes through the cavernous sinus. The third, fourth, and sixth cranial nerves are attached to the lateral wall of the sinus. The ophthalmic and maxillary divisions of the fifth cranial nerve are embedded in the wall.
This intimate juxtaposition of veins, arteries, nerves, meninges, and paranasal sinuses accounts for the characteristic etiology and presentation of CST. Staphylococcus aureus accounts for approximately 70 % of all infections. Streptococcus pneumoniae, gram-negative bacilli, and anaerobes can also be seen. Fungi are a less common pathogen and may include Aspergillus and Rhizopus species.
Mortality / Morbidity
Prior to the advent of effective antimicrobial agents, the mortality rate from CST was effectively 100 %. Typically, death is due to sepsis or central nervous system (CNS) infection. With aggressive management, the mortality rate is now less than 30 %. Morbidity, however, remains high, and complete recovery is rare. Roughly one sixth of patients are left with some degree of visual impairment, and one half have cranial nerve deficits.
Causes
- Most cases of septic CST are due to an acute infection in an otherwise healthy individual. However, patients with chronic sinusitis or diabetes mellitus may be at a slightly higher risk.
The causative agent is generally Staphylococcus aureus, although streptococci, pneumococci, and Cavernous sinus thrombosis.
Clinical signs
The early signs and symptoms of cavernous sinus thrombosis (CST) may not be specific. A patient who presents with headache and any cranial nerve findings should be potentially evaluated for CST. The most common signs of CST are related to the anatomical structures affected within the cavernous sinus.
- Patients generally have sinusitis or a midface infection (most commonly a furuncle) for 5–10 days. In as many as 25 % of cases in which a furuncle is the precipitant, it will have been manipulated in some fashion (eg, squeezing, surgical incision).
- Headache is the most common presentation symptom and usually precedes fevers, periorbital edema, and cranial nerve signs. The headache is usually sharp, increases progressively, and is usually localized to the regions innervated by the ophthalmic and maxillary branches of the fifth cranial nerve.
- In some patients, periorbital findings do not develop early on, and the clinical picture is subtle.
- As the infection tracts posteriorly, patients complain of orbital pain and fullness accompanied by periorbital edema and visual disturbances.
- Without effective therapy, signs appear in the contralateral eye by spreading through the communicating veins to the contralateral cavernous sinus. Eye swelling begins as a unilateral process and spreads to the other eye within 24–48 hours via the intercavernous sinuses. This is pathognomonic for CST.
- The patient rapidly develops mental status changes including confusion, drowsiness, and coma from CNS involvement and/or sepsis. Death follows shortly thereafter.
Other than the findings associated with the primary infection, the following signs are typical:
- Periorbital edema may be the earliest physical finding:
- Chemosis results from occlusion of the ophthalmic veins.
- Lateral gaze palsy (isolated cranial nerve VI) is usually seen first since CN VI lies freely within the sinus in contrast to CN III and IV, which lie within the lateral walls of the sinus.
- Ptosis, mydriasis, and eye muscle weakness from cranial nerve III dysfunction.
- Manifestations of increased retrobulbar pressure follow:
- Exophthalmos.
- Ophthalmoplegia.
- Signs of increased intraocular pressure (IOP) may be observed:
- Pupillary responses are sluggish.
- Decreased visual acuity is common owing to increased IOP and traction on the optic nerve and central retinal artery.
- Hypoesthesia or hyperesthesia in dermatomes supplied by the V1 and V2 branches of the fifth cranial nerve.
- Appearance of signs and symptoms in the contralateral eye is diagnostic of CST, although the process may remain confined to one eye.
- Meningeal signs, including nuchal rigidity and Kernig and Brudzinski signs, may be noted.
- Systemic signs indicative of sepsis are late findings. They include chills, fever, shock, delirium, and coma.
FBC, ESR, blood cultures, and sinus cultures help establish and identify an infectious primary source. Lumbar puncture is necessary to rule out meningitis.
A MRI using flow parameters and an MR venogram are more sensitive than a CT scan, and are the imaging studies of choice to diagnose cavernous sinus thrombosis. Findings may include deformity of the internal carotid artery within the cavernous sinus, and an obvious signal hyperintensity within thrombosed vascular sinuses on all pulse sequences.
Treatment
Cavernous sinus thrombosis has a mortality rate of less than 20 % in areas with access to antibiotics. Before antibiotics were available, the mortality was 80–100 %. Morbidity rates also dropped from 70 % to 22 % due to earlier diagnosis and treatment.
Recognizing the primary source of infection (i.e., facial cellulitis, middle ear, and sinus infections) and treating the primary source expeditiously is the best way to prevent cavernous sinus thrombosis.
Broad-spectrum intravenous antibiotics are used until a definite pathogen is found.
Vancomycin may be used if significant concern exists for infection by methicillin-resistant Staphylococcus aureus or resistant Streptococcus pneumoniae. Appropriate therapy should take into account the primary source of infection as well as possible associated complications such as brain abscess, meningitis, or subdural empyema. Anticoagulation with Heparin is controversial. Retrospective studies show conflicting data. This decision should be made with subspecialty consultation. Steroid therapy is also controversial and is not recommended by many sources. All patients with CST are usually treated with prolonged courses (3–4 weeks) of IV antibiotics. If there is evidence of complications such as intracranial suppuration, 6–8 weeks of total therapy may be warranted.
All patients should be monitored for signs of complicated infection, continued sepsis, or septic emboli while antibiotic therapy is being administered.
Complications of untreated CST include extension of thrombus to other dural venous sinuses, carotid thrombosis with concomitant strokes, subdural empyema, brain abscess, or meningitis. Septic embolization may also occur to the lungs, resulting in ARDS, pulmonary abscess, empyema, and pneumothorax.
Complications in treated patients include oculomotor weakness, blindness, pituitary insufficiency, and hemiparesis.
In order to treat an acute dentoalveolar infection as well as a fascial space abscess correctly, the following are considered absolutely necessary.
Take a detailed medical history from the patient. There are following indications for hospital admission: temperature > 38.3 °C, dehydration, threat to the airway or vital structures, infection in moderate or high severity anatomic spaces, need for general anesthesia, need for inpatient control of systemic disease and other.
The most frequent cause of death in reported cases of odontogenic infection is airway obstruction. Therefore, the surgeon must assess current or impending airway obstruction within the first few moments of evaluating the patient with a head and neck infection. Complete airway obstruction is, of course, a surgical emergency. In such cases insufficient or absent air movement in spite of inspiratory efforts will be apparent. In highly skilled hands one brief attempt at endotracheal intubation may be made, but a direct surgical approach to the airway by cricothyroidotomy or tracheotomy is more predictably successful. In such extreme circumstances the presence of infection overlying the trachea is less important than the absence of ventilation. Therefore, infection in the region of surgical airway access is not a contraindication to an emergency cricothyroidotomy or tracheotomy
Drainage of pus, when its presence in tissues is established. This is achieved by way of the root canal, with an intraoral incision, with an extraoral incision, and through the alveolus of the extraction. Without evacuation of pus that is with administration of antibiotics alone the infection will not resolve. Drilling of the responsible tooth during the initial phase of inflammation, to drain exudates through the root canal. In this way, spread of inflammation is avoided and the patient is relieved of the pain. Drainage may also be performed with trepanation of the buccal bone, when the root canal is inaccessible. In general, surgery for management of severe odontogenic infections is not difficult. Given a thorough knowledge of the anatomy of the deep fascial spaces of the head and neck, the surgeon should be able, by using appropriate anatomic landmarks, to use small incisions and blunt dissection without direct exposure and visualization of the entire infected anatomic space. Another important principle of surgical incision and drainage is the need to dissect a pathway for the drain that includes the locations where pus is most likely to be found.
On the management of deep fascial space infections of the head and neck there are two approaches to surgical drainage of deep neck infections. First strategy is to use parenteral antibiotic therapy as a means of controlling, localizing, or even eradicating the soft tissue infection. Failure of the medical approach is determined by patient aggravation, impending airway compromise, and the identification of an abscess by CT or clinical examination or both. Only then is surgical drainage undertaken. The expectant approach to management of severe odontogenic infections has not been supported by empiric investigation. The alternative strategy is the immediate establishment of airway security as necessary, and aggressive early surgical intervention. Identification of an abscess is not required before surgical intervention. This approach is predicated on the concept that early incision and drainage aborts the spread of infection into deeper and more critical anatomic spaces, even when it is in the cellulites stage.
Planning of the incision and steps so that:
- Antisepsis of the area with an antiseptic solution before the incision.
- Anesthesia of the area where incision and drainage of the abscess are to be performed, with the block technique together with peripheral infiltration anesthesia at some distance from the inflamed area, in order to avoid the risk of existing microbes spreading into deep tissues.
- Injury of ducts (Wharton, Stenson) and large vessels and nerves is avoided. Incision for drainage of a sublingual abscess is performed parallel to the submandibular duct and the lingual nerve. During cutaneous incisions, the course of the facial artery and vein must be taken into consideration, as well as that of the facial nerve movement of the fluid inside the abscess. If the incision is premature, there is usually a small amount of bleeding, no pain relief for the patient and the edema does not subside.
- Sufficient drainage is allowed. The incision is performed superficially, at the lowest point of the accumulation, to avoid pain and facilitate evacuation of pus under gravity. The incision is not performed in areas that are noticeable, for esthetic reasons; if possible, it is performed intraorally.
- Placement of a rubber drain inside the cavity and stabilization with a suture on one lip of the incision, aiming to keep the incision open for continuous drainage of newly accumulated pus. The advantages of drainage are the provision of two pathways for the egression of pus, placement of the incisions in healthy tissue in cosmetically acceptable areas, and the ability to irrigate the infected wound with unidirectional flow from one incision to the other. Wound irrigation is facilitated especially by the use of tube drain, which is noncollapsible and perforated.
- Removal of the responsible tooth as soon as possible, to ensure immediate drainage of the inflammatory material, and elimination of the site of infection. Extraction is avoided if the tooth can be preserved, or if there is an increased risk of serious complications in cases where removal of the tooth is extremely difficult.
Administration of antibiotics, when swelling is generally diffuse and spreading, and especially if there is fever present, and infection spreads to the fascial spaces, regardless of whether there is an indication of the presence of pus. Antibiotic therapy is usually empiric, given the fact that it takes time to obtain the results from a culture sample. These antibiotic choices are separated by severity of infection. Penicillin group of antibiotic continues to be a highly effective for uncomplicated odontogenic infections, owing to its low cost and low incidence of unwanted side effects. Most resistance to penicillin that occurs among the oral pathogens is due to synthesis of P-lactamase. Therefore, it is reasonable to use penicillin plus a P-lactamase inhibitor such as ampicillin-sulbactam or a penicillin plus metronidazole as alternative antibiotics for serious odontogenic infections. The penicillins and metronidazole have the advantage of crossing the blood-brain barrier when the meninges are inflamed. Clindamycin, on the other hand, does not cross the blood-brain barrier. Therefore, it is appropriate to use penicillin plus metronidazole or ampicillin-sulbactam when there is a risk of an odontogenic infection entering the cranial cavity. Few cephalosporins are able to cross the blood-brain barrier. Some third generation cephalosporins, such as ceftadizime, can do so. In addition, ceftadizime is effective against the oral streptococci and most oral anaerobes.Among the cephalosporins, therefore, ceftadizime is the alternative antibiotic of choice. A new fluoroquinolone antibiotic, moxifloxacin has great promise in the treatment of head and neck infections. Its spectrum against oral streptococci and anaerobes is excellent. Its absorption is virtually complete via either the oral or intravenous routes, and it penetrates bone readily. The tissue level of antibiotics determines their effectiveness. Those tissue levels are of course dependent on the antibiotic’s level in serum, through which the antibiotic must pass in order to achieve therapeutic levels in soft tissues, bone, brain, and abscess cavities. Administration of antibiotics by the oral route requires that the drug successfully navigate the vagaries of the highly acidic stomach, the chemical qualities of ingested foods, and the basic intestinal tract. Some antibiotics, however, are equally well absorbed intravenously and orally. The fluoroquinolones, such as ciprofloxacin and moxifloxacin, are the best examples of this. For this reason the fluoroquinolones are not given intravenously unless use of the oral route is contraindicated. Dosage intervals should not be changed from published guidelines by the surgeon. Nonetheless, the surgeon must be aware of the greater effectiveness of intravenous antibiotics over their oral counterparts.
Criteria for changing antibiotics: allergy, toxic reaction, or intolerance, culture and/or sensitivity test indicating resistance, failure of clinical improvement, given, removal of odontogenic cause, adequate surgical drainage (suggest postoperative imaging), other causes for treatment failure ruled out 48–72 h of the same antibiotic therapy. Medical supportive care for the patient with a severe odontogenic infection is composed of hydration, nutrition, and control of fever in all patients.
Chapter 13. Benign tumors and tumor-like lesions of the maxillofacial area and neck
Tumors and tumor-like lesions of the maxillofacial area are very numerous and have various clinical manifestation and gistogenesis. Some of these tumors may be found in other areas of the human body, but there are also specific neoplasms which occur only in the maxillo-facial area. Maxillofacial tumors originate from different tissues ectodermal, mesodermal, entodermal or mesenchymal. Maxillofacial area is more liable to the action of exogenous carcinogens.
Benign tumors and tumor-like lesions of the soft tissues
Fibroma
A fibroma, also referred to as an irritation fibroma, is by far the most common of the oral fibrous growths. Although the terminology implies a benign neoplasm, most if not all fibromas represent reactive focal fibrous hyperplasia due to trauma or local irritation. Although the term focal fibrous hyperplasia more accurately describes the clinical appearance and pathogenesis of this entity, it is not commonly used.
A fibroma may occur at any oral site, but most often it is seen on the buccal mucosa along the plane of occlusion of the maxillary and mandibular teeth. It appears as a round-to-ovoid, asymptomatic, smooth, firm, and sessile or pedunculated mass. The diameter may vary from 1 mm to several centimeters. The surface may be hyperkeratotic or ulcerated because of continued trauma.
Fibromas most often are observed in adults, but they may occur in individuals of any age. Females are affected twice as frequently as males.
The clinical differential diagnosis of a fibroma includes giant cell fibroma, neurofibroma, peripheral giant cell granuloma, mucocele, and benign and malignant salivary gland tumors.
Histologically, a fibroma is an unencapsulated, solid, nodular mass of dense and sometimes hyalinized fibrous connective tissue that is often arranged in haphazard fascicles. A mild chronic inflammatory infiltrate may be observed. The surface epithelium may be hyperkeratotic, either hyperplastic or atrophic, and it may be ulcerated. Conservative excisional biopsy is curative, and its findings are diagnostic; however, recurrence is possible if the exposure to the offending irritant persists.
A giant cell fibroma has a distinctive histologic appearance that sets it apart from a conventional fibroma. It appears as an asymptomatic sessile or pedunculated nodule that is smaller than 1 cm in diameter. Often, it has a bosselated or somewhat papillary surface. Most cases are diagnosed in persons aged 10–30 years, and no sex predilection exists. The most common site is the mandibular gingiva, followed by the maxillary gingiva, tongue, and palate.
The clinical differential diagnosis includes squamous papilloma, irritation fibroma, pyogenic granuloma, and peripheral giant cell granuloma.
Microscopically, a giant cell fibroma is an unencapsulated mass of loose fibrous connective tissue that contains numerous characteristic large, plump, spindle-shaped and stellate fibroblasts, some of which are multinucleated. These cells are easily observed in the peripheral areas of the lesion, whereas the more central areas contain typical fusiform fibroblasts. The surface epithelium is corrugated and atrophic; in contrast to an irritation fibroma, a giant cell fibroma has thin, elongated rete ridges. Conservative excisional biopsy is curative, and its findings are diagnostic. Recurrence is rare.
A peripheral ossifying fibroma is also known as a calcifying fibrous epulis or a peripheral fibroma with calcification. It is a reactive gingival lesion that is believed to arise from cells of the periodontal ligament or periosteum. Most often, it is located in the gingival papilla between adjacent teeth. A peripheral ossifying fibroma appears as a sessile or pedunculated mass, which is often ulcerated; generally, its diameter is less than 2 cm. Primarily, peripheral ossifying fibromas are seen in persons aged 10–20 years. Females are affected more often than males by a ratio of about 3:2. The maxillary gingiva is involved more often than the mandibular gingiva; usually, the anterior region is affected. Mobility and/or migration of adjacent teeth is occasionally observed. Microscopically, fibrous proliferation is accompanied by increased cellularity with plump, immature fibroblasts and variable amounts of calcified material. This material may be osteoid, cementoid, or dystrophic. In some cases, this characteristic pattern is only part of the pattern of a larger lesion that resembles an irritation fibroma or pyogenic granuloma. Surface ulceration is common. The clinical differential diagnosis of a peripheral ossifying fibroma includes inflammatory gingival hyperplasia, peripheral giant cell granuloma, pyogenic granuloma, peripheral odontogenic fibroma, and fibroma.
Treatment consists of excision down to the periosteum and the elimination of any local irritants. Care must be taken to maintain or reestablish acceptable gingival architecture and periodontal integrity. A recurrence rate of 16 % is reported. Even in cases complicated by recurrence, reexcision is generally successful, with the retention of the associated tooth.
A peripheral odontogenic fibroma is a rather uncommon neoplasm that is believed to arise from odontogenic epithelial rests in the periodontal ligament or the attached gingiva itself. The entity, formerly confused with peripheral ossifying fibroma, is currently considered to be the extraosseous counterpart of the central odontogenic fibroma of the World Health Organization type. A peripheral odontogenic fibroma appears as a firm, slowly growing, sessile, and nodular growth of the gingiva, most often on the mandibular buccal or labial aspect. It occurs in persons of a wide age range and affects both sexes equally.
The clinical differential diagnosis of a peripheral odontogenic fibroma includes inflammatory gingival hyperplasia, peripheral ossifying fibroma, and peripheral giant cell granuloma.
Microscopically, the tumor consists of an unencapsulated mass of interwoven cellular fibrous connective tissue that contains scattered nests or strands of odontogenic epithelium. Myxoid foci; calcifications; or osteoid, cementoid, or dysplastic areas are sometimes seen. The surface generally is not ulcerated.
Treatment consists of conservative excision performed with care to maintain or reestablish the gingival architecture and periodontal integrity. The tendency for recurrence is low.
Desmoplastic fibroma
A desmoplastic fibroma is considered to be the intraosseous counterpart of the soft-tissue fibromatosis. A desmoplastic fibroma appears as a firm,
painless, poorly demarcated mass that is either rapidly or slowly growing. Usually, it involves the tongue or buccal mucosa. The mass is locally aggressive, blends into surrounding structures, and causes resorption of the underlying bone when it is present.
The differential diagnosis of a fibromatosis includes low-grade fibrosarcoma, nodular fasciitis, reactive fibrous hyperplasia, fibrous histiocytoma, and neurofibroma.
Treatment consists of wide excision. The reported recurrence rate of 24 % for intraoral fibromatoses is considerably lower than the 50–70 % rate reported for fibromatoses of the entire head and neck region.
Myofibroma
Myofibroblasts have features of both fibroblasts and smooth muscle cells. Myofibroblasts have been identified in lesions other than myofibromas, but when they are the predominant cell type in a tumor, the terms myofibroma (if solitary) or myofibromatosis (if multicentric) are applied. The tumors are benign, and, although myofibromatosis is similar to fibromatosis in many ways, its behavior is less aggressive. Tumors of the myofibroblasts may occur in either sex and in patients of all ages, with a mean patient age of 26.6 years.
Myofibroblastic tumors are most common in the head and neck region, including oral and perioral sites, than in other areas. Intraoral lesions occur mainly on the tongue, lips, and buccal mucosa. Tumors also have been described in the dermis, soft tissues, viscera, and bone. Jaw lesions, usually mandibular lesions, generally appear as well-defined unilocular or multilocular radiolucencies. Oral lesions appear as firm submucosal nodules or exophytic masses with a diameter of 0.3–5.0 cm. Although lesions are most often asymptomatic, they may be tender or even painful.
The clinical differential diagnosis for oral myofibroma includes irritation fibroma, peripheral giant cell fibroma, neurofibroma, leiomyoma, and benign and malignant neoplasms of the minor salivary glands.
Treatment for oral myofibromas is conservative excision. The recurrence rate is low, and spontaneous regression is reported.
Juvenile nasopharyngeal angiofibroma (angiofibroma, nasopharyngeal fibroma, bleeding fibroma of adolescence, fibroangioma)
Juvenile angiofibroma (JNA) is a benign tumor that tends to bleed and occurs in the nasopharynx of prepubertal and adolescent males. The lesion originates in close proximity to the posterior attachment of the middle turbinate, near the superior border of the sphenopalatine foramen. A hormonal theory has been suggested because of the lesion’s occurrence in adolescent males. Other theories include a desmoplastic response of the nasopharyngeal periosteum or the embryonic fibrocartilage between the basiocciput and the basisphenoid. Etiology from nonchromaffin paraganglionic cells of the terminal branches of the maxillary artery has also been suggested.
Clinical symptoms
Nasal obstruction (80–90 %) – Most frequent symptom, especially in initial stages. Epistaxis (45–60 %) – Mostly unilateral and recurrent; usually severe epistaxis that necessitates medical attention; diagnosis of angiofibroma in adolescent males to be ruled out. Headache (25 %) – especially if paranasal sinuses are blocked; facial swelling (10–18 %); other symptoms – unilateral rhinorrhea, anosmia, hyposmia, rhinolalia, deafness, otalgia, swelling of the palate, deformity of the cheek. There are main signs: nasal mass (80 %); orbital mass (15 %); proptosis (10–15 %). Other signs including serous otitis due to eustachian tube blockage, zygomatic swelling and trismus that denote spread of the tumor to the infratemporal fossa, decreasing vision due to optic nerve tenting (rare).
Treatment include: hormonal therapy (the testosterone receptor blocker flutamide was reported to reduce stage I and II tumors to 44 %. Despite tumor reduction with hormones, this approach is not routinely used).
Radiotherapy (Some centers have reported 80 % cure rates with radiation therapy. However, concerns regarding potential effects of radiation make radiation therapy a nonuseful modality in most cases).
Stereotactic radiotherapy (e.g., Gamma knife) delivers a lower dose of radiation to surrounding tissues. However, most authorities reserve radiotherapy for intracranial disease or recurrent cases.
Surgical therapy include: a lateral rhinotomy, transpalatal, transmaxillary, or sphenoethmoidal route is used for small tumors (Fisch stage I or II). The infratemporal fossa approach is used when the tumour has a large lateral extension.
The midfacial degloving approach, with or without a Le Fort osteotomy, improves posterior access to the tumor. The facial translocation approach is combined with Weber – Ferguson incision and coronal extension for a frontotemporal craniotomy with midface osteotomies for access. An extended anterior subcranial approach facilitates en bloc tumor removal, optic nerve decompression, and exposure of the cavernous sinus. Intranasal endoscopic surgery is reserved for tumors limited to the nasal cavity and paranasal sinuses.
Neurofibroma
A neurofibroma is, like a schwannoma, derived from sheath cells. It actually may represent in many instances a hamartoma or a reactive process rather than a neoplasm. A neurofibroma is asymptomatic and rarely occurs as a single lesion. Most often neurofibromas are part of von Recklinghausen’s disease (Fig. 13.1). Quite often the tongue is involved, in some cases resulting in unilateral macroglossia.

Fig. 13.1. Neurofibromatosis I type (after 9 operations)
Also the possibility of hereditary neuropolyendocrine syndrome – consisting of mucosal neuromas, pheochromocytoma of the adrenal glands, and medullary thyroid carcinoma should be taken into account. In general, the mucosal neuromas in that syndrome are already present at childhood, being the first manifestation of the syndrome (Casino et al, 1981). In contrast to the schwannoma, a neurofibroma is not encapsulated.
Proliferating Schwann’s cells are haphazardly arranged, not showing the palisade arrangement of schwannomas. With a single neurofibroma, management consists of surgical removal (Fig. 13.2; 13.3). With multiple or massive involvement, surgical removal may be impossible to carry out and is indicated only when malignant changes are suspected. With von Recklinghausen’s disease, there is a 5 % to 15 % risk of malignant degeneration. This seems especially true for deeply located lesions (Maceri and Saxon, 1984).

Fig. 13.2. Planning before operation

Fig. 13.3. IV stage of the surgical treatment (made in our clinic)
Neurilemmoma
Neurilemmomas are benign encapsulated tumors of the nerve sheath. Their cell of origin is thought to be Schwann cells derived from the neural crest. These masses usually arise from the side of a nerve, are well encapsulated, and have a very unique histologic pattern. The benign lesion essentially manifests with cosmetic deformity, a palpable mass, and/or symptoms similar to a compressive neuropathy. Neurologic symptoms tend to present late. Symptoms can be vague, with an average interval of up to 5 years before the diagnosis is established. Neurilemmoma is the most common neurogenic tumor. The prevalence of these benign lesions is unknown. The cause for the growth of these neoplasms is unknown. Neurilemmoma can be associated with von Recklinghausen disease, and, when associated, multiple tumors often are present. Neurilemmomas affect persons aged 20–50 years. The head and flexor surface of the upper and lower extremities and the trunk are common locations in decreasing order. The mass is usually mobile in the transverse plane and tethered along the axis of the nerve from which it arises. Tenderness to palpation is often present; secondary neurologic symptoms may be present if the tumor is large. When involving the C7 nerve root, neurilemmoma has been described as a cause of thoracic outlet syndrome. Lesions in the sciatic nerve can mimic discogenic low back pain.
Differential diagnoses include the following: fibroma, neurofibroma, neurosarcoma, ganglion cyst, giant cell tumor of tendon sheath, lipoma.
Lipoma
A lipoma is a benign neoplasm composed of fat cells. Its cause is unknown. Trauma and metaplasia of perivascular connective tissue have been suggested as playing a role. Oral and oropharyngeal lipomas are rather rare. There is no predilection for sex. An oral lipoma rarely occurs before the second decade. A lipoma appears as a sessile, soft, and asymptomatic swelling (Fig. 13.4; 13.5; 13.6; 13.7; 13.8).

Fig. 13.4. Giant lipoma of the neck, frontal area

Fig. 13.5. CT scanning of the lipoma

Fig. 13.6. Planning the incision before operation

Fig. 13.7. Extraction of the tumor within capsule

Fig. 13.8. Macropreparation of the lipoma
When it is located superficially, a yellowish texture can be seen. In rare instances bilateral or multiple occurrence has been reported (Pisanty, 1976). Histologic examination of a lipoma shows a well-delineated mass of lobules of fat cells with fibrous septa interspersed between them. In rare instances one encounters a benign “infiltrative” lipoma, which should not be confused with a liposarcoma (Bennhoff and Wood, 1978). The distinction between a benign lipoma and a low-grade liposarcoma may indeed be difficult in some cases. When fibrous tissue is a substantial part of a lipoma, the term fibrolipoma can be applied. When vascularity is a prominent feature, the term angiolipoma is used.
Leiomyoma
A leiomyoma is a benign neoplasm composed of smooth muscle cells. The source of a smooth muscle tumor in the oral cavity is believed to be the walls of blood vessels or undifferentiated mesenchymal cells. Occurrence of a leiomyoma in the oral cavity is rare. In two reviews of the literature (Natiella et al, 1982; Praal et al, 1982) approximately 80 oral leiomyomas were collected. The majority of reported leiomyomas of the oral cavity and oropharynx were small, circumscribed, and asymptomatic swellings, covered with an apparently intact mucosa. They were either single or multiple. A leiomyoma is composed of whorls of smooth muscle cells. The diagnosis of leiomyoma can be difficult to make just from light microscopic examination. The tumor should be differentiated from fibromatosis and schwannoma on the one hand and leiomyosarcoma on the other hand. Management consists of surgical removal.
Rhabdomyoma
A rhabdomyoma is a benign neoplasm of striated muscle. It is an exceedingly uncommon tumor. The male-female ratio is more than 2 to 1. The mean age of patients with a rhabdomyoma is about 40 years. Although extracardiac rhabdomyomas show a preference for the head and neck, occurrence in the oral cavity and oropharynx is rare. The floor of the mouth is the most common site. Multifocal appearance is exceptional (Schlosnagle et al, 1983). The clinical presentation is a submucosal swelling without any specific signs or symptoms. A rhabdomyoma is a well-circumscribed tumor. Based on histopathologic characteristics and gross morphology, two types are recognized: fetal and adult. The adult type is composed of large, round or polygonal cells with a slight granular cytoplasm. The cytoplasm may contain lipod material. Cross striations may be found in just a few cells. The fetal type almost exclusively occurs in the first few years of life. Histologically that type is characterized by immature skeletal muscle in varying stages of developmental and undifferentiated mesenchymal cells. Differentiating a rhabdomyoma from a rhabdomyosarcoma may be difficult. Management of a rhabdomyoma consists of surgical removal.
Fibrous growths of the oral soft tissues are fairly common and include a diverse group of reactive and neoplastic conditions.
Fibrous overgrowth
Fibrous overgrowths or fibroepithelial polyps are relatively common in the mouth and are usually the result of trauma or frictional irritation. By contrast, fibromas, which are benign neoplasms, are extremely rare. They are most often seen in the cheeks or lips where such irritation from the dentition can be encountered (Fig. 13.9; 13.10).

Fig. 13.9. Fibrous overgrowths

Fig. 13.10. Fibroma of the of the palate
sublingual area
Sometimes known as polyps, they may be semi-pedunculated or sessile in their attachment and are similar in colour to the surrounding normal tissue unless they have been traumatised frictionally, when they may show a whitened keratinised surface. They do not, however, have the cauliflower hyperkeratotic surface of the papilloma, being smooth-surfaced and hence easily distinguished from the papilloma.
Treatment is simple surgical excision. As, histologically, they are simple hyperplasias, there is no requirement to remove a margin of normal tissuenor to extend the excision deeply into the underlying tissues. A suture may be needed to ensure adequate haemostasis in the larger lesions.
Fibrous epulis
An epulis may be defined as a swelling or lump arising from the gingivae, and the fibrous epulis is the most common type. The lesion is basically a hyperplastic response to irritation to the attached gingivae. In some cases, the stimulus or irritant is very obvious, such as an overhanging restoration or subgingival calculus. In others, however, it may be more difficult to detect and only careful examination may reveal a small developmental defect in the enamel or dentine of the tooth at the gingival margin. Clinically, they present as smoothsurfaced, rounded swellings, normally pink in colour and often pedunculated in attachment (Fig. 13.11).

Fig. 13.11. Fibrous epulis
In older, more mature lesions, the surface may show stippling reflecting the attached gingival origin of the overgrowth.
Treatment is by surgical excision, with removal of any irritant focus found. The base of the wound is often dressed with a periodontal pack or if larger with a ribbon gauze impregnated with Whitehead’s varnish. This may be sutured over the raw surface.
Giant cell epulis
This epulis is sometimes known as a peripheral giant-cell granuloma and, as its name implies, the tissue consists of a mass of multinucleated giant cells in a vascular stroma. Many are seen in teenagers or adolescents and are usually found in the anterior regions of the mouth. They may represent an overgrowth of osteoclasts derived from the resorptive process encountered during the loss of the deciduous dentition. They can, however, arise in the older patient. These lesions are typically deep red or even purplish in colour and are often quite broadly based, unlike the paler coloured, often pedunculated fibrous epulis (Fig. 13.12; 13.13).

Fig. 13.12. Giant cell epulis

Fig. 13.13. X-ray examination
of the giant cell epulis
If suspected of being a giant-cell lesion, radiographs should be taken to ensure that it is a peripheral and not a centrally, i.e. bony, originating lesion, which would appear as a radiolucent area. If it is a peripheral epulis then surgical excision with curettage or cautery to its base is normally curative. The base of the lesion can be covered by a periodontal pack if small, or a Whitehead’s varnish packing may be used for larger lesions. If a central giant-cell lesion is evident on the radiograph, it must be distinguished from the brown tumour of hyperparathyroidism by appropriate assessment of blood calcium, phosphate and parathormone levels.
Pregnancy epulis
This lesion is histologically indistinguishable from the pyogenic granuloma, being essentially a vascular overgrowth of granulation tissue. It may be related to an obvious focus such as calculus but it may equally arise from an extraction socket. Hormonal changes during pregnancy are believed to enhance the reactive tissue response to irritation and although many lesions remain small and do not require surgical intervention, some can grow alarmingly fast and attain considerable size even to the point of being traumatised by the opposing teeth. These lesions are therefore surgically excised with appropriate curettage or diathermy to their bases. If small they tend to resolve following the pregnancy.
Epulis Fissuratum (denture-induced hyperplasia, inflammatory hyperplasia, denture hyperplasia, denture-induced fibrous hyperplasia).
Epulis fissuratum is a hyperplastic reactive lesion, often with inflammatory and reparative phases. The histologic picture can be variable. Most frequently, a dense fibrous hyperplasia occurs, often with varying degrees of inflammation and vascularity. Because capillary proliferation is considerable, an overlap with pyogenic granuloma occurs. Mucous glands are often present in the specimen and may show a chronic sialadenitis. Occasionally, the glands may have an associated lymphoid hyperplasia and papillary ductal hyperplasia. The epithelium may be atrophic or hyperplastic and occasionally shows a pseudoepitheliomatous hyperplasia. Ulceration can occur. Infrequently, chondroid or osseous metaplasia can develop within the mass.
Treatment
Surgically excise the epulis fissuratum because even removal of the offending stimulus (ie, denture) will not result in complete resolution. In addition, correct the denture, otherwise the lesion will recur. Either make a new denture or reline the old denture.
Congenital (granular cell) epulis
The rare congenital epulis is typically present at birth as a smooth but prominent soft nodule, usually on the alveolar ridge. Females are predominantly affected and occasionally the mass is so large as to obstruct respiration.
Histologically, large pale granular cells with sharply-defined cell membranes are covered by epithelium which lacks pseudoepitheliomatous hyperplasia. Immunohistochemistry suggests that the origin is myogenous. Excision is curative but spontaneous regression is also seen.
Papilloma
A papilloma is a benign epithelial neoplasm composed of fingerlike projections of squamous epithelium. Some authors use the term squamous papilloma (Abbey et al, 1980). The cause is unknown, although a virus is most likely. The prevalence of oral papillomas is less than 0.1 % (Axell, 1976). Oral and oropharyngeal papillomas may occur as single or multiple, sessile, warty lesions, seldom measuring more than a few millimeters (Fig. 13.14; 13.15). When they involve the oropharynx, the soft palate and the uvula are the usual sites. The clinical differential diagnosis of a papilloma includes verruca vulgaris (Green et al, 1986), fibroepithelial polyp, focal epithelial hyperplasia, and condyloma acuminatum.

Fig. 13.14. Papilloma of the lower
palpebra

Fig. 13.15. Papilloma of the tongue
The histology of a papilloma shows fingerlike projections of squamous epithelium above the level of the surrounding mucosa. In most cases a mild hyperorthokeratosis occurs. Epithelial dysplasia is not a feature of papilloma. Carcinomatous changes in a papilloma are exceptional, if indeed ever proven.
Squamous cell papilloma
This is not an uncommon lesion of the oral mucosa and may arise at virtually any site, but more commonly on palate, buccal mucosa or lips. It is a benign neoplasm of epithelial tissue and most squamous cell papillomata present as pedunculated (stalked attachment) lesions with characteristic white, hyperkeratinised, crenated surfaces, which can be likened to a cauliflower. They are normally small, usually less than 0.5 cm in diameter.
Treatment is simply excision at the base of the stalk.
Pyogenic Granuloma
A pyogenic granuloma is a benign, elevated, and capillary-rich lesion occurring on the skin and mucous membranes. When located at the gingiva of pregnant women, the term pregnancy tumor may be used. The pyogenic granuloma is thought to be the result of an overreaction to minor trauma rather than to infection. The pyogenic granuloma is a lesion that arises from a failure of normal healing causing an exuberant overgrowth of what is essentially granulation tissue. They may grow in relation to extraction sockets or from traumatic injuries to soft tissues, most often tongue or palate. They can be regarded as reactive lesions and obvious irritational factors may be evident clinically or from the patient’s history. Foreign bodies related to extraction sockets, such as fragments of filling material or indeed of small bony sequestra, may form the stimulus, whereas in soft tissues there is occasionally a history of self-medication with a variety of remedies that could be attributed as causal. Hormonal changes may be another cause. It has no predilection for sex or age group. An oral pyogenic granuloma most frequently involves the gingiva. The lower lip and the dorsal surface of the tongue are rather common sites as well.
The lesion is usually pedunculated or sessile, and the surface is often ulcerated. Clinically they appear as red or speckled-red overgrowths of tissue that closely resemble granulation tissue on visual examination.The size of the lesion’s diameter may vary from 0.5 to 2 cm or more.
Histologically a pyogenic granuloma does not consist of true granulomas. Large numbers of vascular spaces can exist together with numerous inflammatory cells, sometimes rising the question of whether one is dealing primarily with a vascular lesion with secondary signs of inflammation or with an inflammatory condition. Mitotic activity may be abundant and should not be mistaken as a sign of malignancy. Differential diagnosis: A very similar lesion may be attributed to a viral origin and is sometimes known as a viral wart. In these cases it is sometimes possible to see finger warts that have clearly been responsible for transmitting the virus to the oral cavity. Treatment is surgical excision with curettage or diathermy to the base of the lesions where appropriate attachment. Surgery is the management of choice. With the exception of the gingival lesions, recurrences of a pyogenic granuloma is rare.
Hemangioma, heamngiopericytoma and phlebectasias
A hemangioma is a benign lesion of blood vessels or vascular elements. Haemangiomas of the head or face are a frequent vascular pathology, consisting in an embryonic dysplasia that involves the cranial-facial vascular network (Fig. 13.16; 13.17).

Fig. 13.16. Hemangioma of the face, capillary form

Fig. 13.17. Big compound hemangioma of the face
Haemangiomas show clinical, morphological, developmental and structural changes during their course. The majority of oral and oropharyngeal hemangiomas seem to be of a developmental nature. In some instances lesions are probably a mixture of hemangioma and lymphangioma, leading to the term angiomatosis (Fig. 13.18).

Fig. 13.18. Systemic angiomatosis
In rare instances a hemangioma is located within the jawbones. Hemangiomas of the oral cavity are often present at birth or shortly thereafter. They have a strong preference for occurrence in the tongue and the floor of the mouth. A hemangioma of the tongue may affect just a part of the tongue or the entire tongue, producing macroglossia (Fig. 13.19; 13.20).

Fig. 13.19. Hemangioma of the mouth

Fig. 13.20. Hemangioma of the and oropharyngeal area tongue, cavernous form
The color of a hemangioma may vary from bluish to purple or fiery red. The texture of the mucosa may be more or less unchanged, showing only an increased vascularity on the surface; in other cases, however, there is a pebbly appearance. Pain is not a prominent feature, except in cases of traumatization or secondary inflammation. In severe cases loss of tongue mobility may occur. Bleeding, either spontaneously or from mechanical irritation, can be a serious problem. Angiography may be an aid in diagnosing a hemangioma.
A hemangioma may histologically consist of numerous irregular, blood – filled spaces, lined by endothelial cells and surrounded by connective tissue. When a large number of proliferating endothelial cells line small capillaries, the lesion is referred to as a capillary hemangioma.
In the case of large dilated blood sinuses, the term cavernous hemangioma is applied. A cavernous hemangioma and a lymphangioma may occasionally be indistinguishable from each other, both clinically and histologically. In the case of ulceration (and thereby the presence of inflammatory cells) distinguishing a hemangioma from a pyogenic granuloma may be impossible. When hemangiomas undergo regression, extensive sclerosis can occur, sometimes followed by calcification. Such concretions are called phleboliths. The majority of hemangiomas do not require treatment and regress spontaneously during childhood.
Therapeutic management of a large, persisting, or even growing hemangioma is a difficult problem. A conservative approach seems justified: that is, managing only the areas that produce bleeding. In large, diffuse lesions the use of cryosurgery or CO2 laser therapy does not seem to be effective. Injection of sclerosing agents has been advocated in the past but has not been shown to be effective. The technique of selective percutaneous embolization before surgery has emerged as a valuable adjunct to surgery in the management of such lesions (Braun et al, 1985; Thompson et al, 1979). Radiotherapy should be avoided because of possible late adverse sequelae.
A hemangiopericytoma is a complex neoplasm that should be regarded as malignant, not in the usual sense of a 5-year survival but over the lifetime of the host (Batsakis, 1979).
Occurrence in the oral cavity and the oropharynx is extremely rare (Morita et al, 1982). The clinical appearance is just a firm, usually well-circumscribed swelling of the mucosa. In patients above the age of 40 to 50 years, single or multiple, bluish, hemangiomalike changes may occur in the oral and lingual mucosa as the result of vein widening. These are so-called phlebectasias (Ettinger and Manderson, 1974). No treatment is required.
Management
The first-line treatment for capillary hemangiomas is simple observation. Since most of these lesions regress on their own, there is no need to intervene unless one of the above criteria is met. Corticosteroids, in various formulations, also have been used in the treatment of capillary hemangiomas. Topical steroid formulations, such as clobetasol propionate cream, can be applied topically to the lesion. The response to these treatments, even with the strongest corticosteroid formulations, is slower than other methods because several weeks are required to obtain a response. Systemic corticosteroids are used for amblyogenic life-threatening lesions.
Surgery
Laser surgery has been attempted to ameliorate capillary hemangiomas but still is controversial. The hemostatic effects of the carbon dioxide laser have been used with success to surgically remove these lesions. Other lasers used include the argon laser and NdYAG laser. The pulsed dye laser is only effective for very superficial lesions; its mechanism of action is too slow for sight-threatening hemangiomas. Overall, variable results have been seen with various laser modalities, and the risks of scarring and ulceration often deter its usage. Incisional surgical techniques also have had variable success. Surgical ligation of the hemangiomas produces equivocal results. Vascular embolization of the lesions should be used for large extraorbital hemangiomas only. Primary excision also has been advocated for infantile hemangiomas.The prognosis for cosmetic and visual recovery is excellent if treatment is instituted at an appropriate time and careful attention is paid to the visual development. Most lesions involute by age 5 years.
Lymphangioma
Lymphangiomas are rare congenital benign lesions occurring mainly in the head, neck and oral cavity. They consist in localized centres of abnormal development of the lymphatic system. Three theories have been proposed to explain the origin of this abnormality. The first suggests that a blockage or arrest of normal growth of the primitive lymph channels occurs during embryogenesis, the second that the primitive lymphatic sac does not reach the venous system, while the third advances the hypothesis that, during embryogenesis, lymphatic tissue lays in the wrong area.
Lymphangiomas are classified as microcystic (capillary lymphangiomas), macrocystic (cavernous lymphangiomas) and cystic hygromas according to the size of the lymphatic cavities incorporated. Cystic lymphangiomas have been reported, in the literature, to be present in up to 67 % of all cystic lymphangiomas There was presented the concept that cystic hygromas and lymphangiomas are variations of a single entity and that its classification is determined by its location in the head and neck. A commonly used classification classifies these lesions into capillary lymphangioma or lymphangioma simplex, cavernous lymphangioma, and cystic lymphangioma or cystic hygroma. When a lymphangioma is confined to fairly dense tissue, such as the tongue, it presents as a cavernous lymphangioma, but when it develops in the relatively loose fascia of the neck, a cystic lesion occurs. These three types are frequently found together in the same patient, depending on the severity of the disease. Cystic hygromas, however, account for approximately 90 % of the lymphangiomas in the head and neck region. Other common sites, outside the head and neck, include the axilla, shoulder, chest wall, mediastinum, abdominal wall, and thigh. Diagnosis is not difficult in most cases. The neoplasms are usually characterized by the presence of a soft, compressible, loculated and ill-defined mass, which is usually located in the posterior cervical triangle. The the tongue lesions are not attached to the skin or movable across deeper tissues, and readily transilluminate.
The anterior triangle of the neck has been indicated as the most common site. Cystic hygroma may be localized in the parotid area, and is the second most common congenital mass of the parotid area (Fig. 13.21; 13.22).

Fig. 13.21. Lymphangioma, cavernous form

Fig. 13.22. Lymphangioma of the tongue
Ultrasound, CT and MRI can be used to define the relationship of the lesion with the neighbouring structures and to help plan surgical strategies 10. US, which provides size and extension of the lesion, should be performed routinely. The clinical course of the pathology varies from a spontaneously regressing cyst to an aggressively invasive lesion. Spontaneous or traumatic haemorrhage of the cysts is the most common complication of the lesion.
Treatment
Surgical resection still remains the best treatment for lymphangiomas; other treatment options, such as sclerotherapy have been proposed as an alternative to reduce the impact and complications of surgery. Various products, such as sodium morrhuate, dextrose, tetracycline, doxycycline, bleomycin, ethibloc and OK-432 (picibanil), have been used as sclerotherapeutic agents. Apart from OK-432, the other agents were reported to cause perilesional fibrosis and thus to complicate eventual surgical excision.
Cysts of the soft tissues
Epidermoid and dermoid cysts are ectoderm-lined inclusion cysts that differ in complexity: Epidermoids have only squamous epithelium; dermoids contain hair, sebaceous and sweat glands, and squamous epithelium. Both arise from trapped pouches of ectoderm, near normal folds, or from failure of surface ectoderm. An epidermoid cyst is a cyst lined by epidermis without the adnexal structures in the fibrous wall that a dermoid cyst has. Sometimes the term dermoid cyst is used in a clinical way, using histologic subdivisions such as dermoid type, epidermoid type, and teratoid type. An epidermoid cyst may result from traumatic implantation of epithelial cells into surface epithelium, whereas in a dermoid cyst entrapment of epithelium during the embryologic phase seems to be the most likely explanation. Both the epidermoid and dermoid cysts rarely occur in the oral cavity and are even rarer in the oropharynx. Epidermoid and dermoid cysts may occur in the floor of the mouth, the lips, and the cheek mucosa (Fig. 13.23; 13.24; 13.25; 13.26).

Fig. 13.23. Epidermoid cyst
of the face

Fig. 13.24. Incision for extaction of the cyst

Fig. 13.25. Extaction of the
epidermoid cys

Fig. 13.26. Epidermoid cyst, macropreparation
Just a few cases of lingual involvement have been reported. The clinical aspect is not characteristic and merely consists of a cystic swelling. Stratified squamous epithelium without adnexal structures lines an epidermoid cyst. When adnexal structures (such as sebaceous glands) exist, a diagnosis of dermoid cyst can be made. In most instances epidermoid and dermoid cysts can be enucleated. Only in very large cysts must marsupialization be considered. Recurrence is rare (Fig. 13.27; 13.28).

Fig. 13.27. Dermoid cyst of the mouth floor

Fig. 13.28. Dermoid cyst of the neck
Congenital cysts and fistule of the neck may be divided into the midline or thyroglossal, and the lateral or so-called branchial cysts and fistulae.
The midline cysts and fistulae are fairly well accepted as arising from the thyroglossal duct. During the development of the human embryo the isthmus of the thyroid gland is derived from a bud of hypoblast which arises in the midventral portion of the floor of the pharynx. This bud migrates downward, forming the thyroglossal duct. Epithelial rests anywhere along the course of this tract may give rise to a cyst or a fistula. The fistula usually reaches the exterior following infection of a cyst by breakipg through the thin skin lining. It is very exceptional to see a midline fistula at birth; ordinarily they are secondary, resulting from infection of a cyst. Wenglowski does not believe in the thyroglossal tract theory, and states that these cysts and fistulhe always end in a blind sac at the level of the hyoid bone to which they may be firmly attached. He further states that the tract between the hyoid bone and the foramen cacum is never patent. In one case we shall see histological evidence of a sinus leading into the foramen cecum, and in another case clinical evidence of patency of the duct. A thyroglossal cyst may develop anywhere from the foramen caecum to the suprasternal notch.. They are far more frequent in the infrahyoid regions. We are taught that thyroglossal cysts are exactly in the midline but we occasionally see them off-centre, particularly those found at the level of the thyroid cartilage, which by its conFig.uration more or less pushes the cyst to one side. Thyroglossal cysts are more frequently observed in children, but may develop at any age. Both sexes appear to be equally affected. The clinical picture is that of a midline “lump or bump,” which may vary in size from a few millimetres to four or five centimetres. It is not adherent to the overlying tissues but moves in a vertical direction on swallowing. Forced protrusion of the tongue also moves the cyst, a sign distinguishing it from a dermoid cyst, which does not move. The picture may be complicated by infection which very often will result in a fistula.
Lateral or branchial cysts
If authors are in reasonable agreement regarding the pathogenesis of the midline cysts and fistule, this is not so in the case of the laterally placed ones (Fig. 13.29; 13.30; 13.31; 13.32).

Fig. 13.29. Lateral cyst of the neck

Fig. 13.30. Lateral cyst, macropreparation

Fig. 13.31. Midline fistule of the neck

Fig. 13.32. Extraction of the midline Fistule
Two distinct theories prevail. The first and oldest maintains that lateral cysts and fistule develop primarily from the branchial apparatus, particularly from the second and the third pouches. The second theory, formulated by Wenglowski and interpreted by Meyer, who reviewed this question in 1932, explains these abnormalities as arising from epithelial rests of the pharyngothymic duct. Arguments for and against every theory have been formulated, and it would be beyond the scope of this paper to go into this controversial subject. For the moment all that can be said is that this question still remains to be clarified. Unlike the midline fistuloe, the lateral fistula is frequently present at birth. Many, however, are acquired as a result of either an infection or an ill-advised incision of a cyst.
At birth the true fistula may consist of only a small dimple and remain as such for a number of years before starting to discharge. The discharge is usually serous until infection sets in, when it becomes purulent and causes irritation of the surrounding skin. The sinus opening is located along the anterior border of the sternomastoid muscle, anywhere from the ear above to the clavicle below. One can sometimes feel the sinus tract as a small subcutaneous cord running up along the anterior border of the muscle. The cyst is usually seen below the angle of the mandible, in front of or beneath the sternomastoid muscle. It develops at any age but is more common in the third decade, and presents itself as a slowly growing nontender mass. The growth may be so slow as to reach a considerable size before being noted by the patient. The cyst very often develops after an infection of the throat or surgical procedure on the throat such as tonsillectomy. Pain is an exceptional symptom unless there is an infection. Pressure upon surrounding structures may, in time, give rise to certain symptoms such as cough through irritation of the vagus nerve. Some authors have reported that congenital cysts and fistulae are more frequently observed in the female sex, but a review of the reported cases indicates that males are probably affected as frequently as females. Fistule are divided into three groups: the complete fistula extending from the pharynx, usually the tonsillar fossa, to the outside; the external fistula having only an external opening; and the internal fistula opening into the pharynx only. This last group is rare.
Diagnosois
The history and complete and careful examination of the patient will help in making the correct diagnosis of congenital cyst or fistula, which should not be confused with the following: dermoid cysts, cystic hygroma, lipoma, tuberculous adenitis, haemangioma, deep cervical abscesses, the various mycoses, carotid body tumour, adenopathies and metastatic carcinoma.
The treatment of these abnormalities is surgical and requires complete and careful excision of the lesion. For thyroglossal tract anomalies the excision must include the midportion of the hyoid bone and a core of tissue from the hyoid bone up to the foramen caecum. For lateral cysts, complete excision by careful dissection through a wide exposure is recommended in order to avoid injury to surrounding structures. Lateral fistule must be followed up to the end. In cases of complete fistula, some authors recommend inverting the stump into the pharynx, but this does not appear to be necessary. The stepladder incision is most useful.
Tumors and tumor-like lesions of salivary glands
Tumors of the salivary glands
According to the classification, developed by World Health Organization (1990) tumors of the salivary glands are grouped into epithelial, nonepithelial, and metastatic.
Over 90 % of salivary gland tumours are epithelial in origin. The WHO classification includes 32 types of epithelial salivary gland tumors, 14 of them are benign. A wide spectrum of histopathological forms is due to the diversity of cell types, composing the glands (acinar cells, ductal cells, and myoepithelial cells). Despite of wide diversity of histological types, their clinical signs and treatment modalities are very common. For this reason only the most common types of epithelial tumors are discussed in this chapter.
Benign nonepithelial tumors include lipoma, hemangioma, lymphangioma, neurinoma, sarcoma and other, located within the salivary gland. They are rare (less than 10 %) and occur almost only in the parotid gland.
In general, the major salivary glands have the higher incidence of tumors and the higher percentage of benign tumors (75–80 %) in comparison to minor glands, where malignances make up to 50 %. The parotid gland is the most typical site for the salivary neoplasms (up to 80 %). The overwhelming majority of them occur in the superficial lobe or tail of the parotis, and most of them are benign (pleomorphic adenomas are predominant).
Salivary gland tumors usually present as a slow growing, well-circumscribed, painless nodule associated with the salivary gland. In early stages, benign and malignant salivary gland tumors cannot be distinguished clinically, so malignancy should be suspected in most of the cases. Another problem is variety of localizations, where salivary gland tumors are observed. It makes the diagnosis and management of salivary gland tumors rather challenging.
The adequate approach for management of the salivary gland tumors demands an accurate histopathologic diagnosis. For this reason fine-needle aspiration and biopsy is often indicated. It can help to differentiate a tumor from lymphadenopathy as well as to indicate the type of salivary tumor. At the same time it is not 100 % sensitive or specific, and sometimes the interpretation of the fine-needle aspiration results is rather difficult. CT scanning, MRI and ultrasonic study are also useful for proper diagnosis. They help to indicate the association of tumor with the salivary glands, deep lobe involvement of the parotid gland and lymphadenopathy in the neck in cases of malignant salivary glands tumors.
Benign epithelial tumors of the salivary glands Pleomorphic adenoma
Pleomorphic adenoma (benign mixed tumor) is the most common benign salivary glands tumor, comprising 78–85 % of all salivary gland neoplasms. Pleomorphic adenoma arises from duct epithelium or myoepithelial cells and consists of epithelial and connective tissue components in varying degrees. In some cases myxoid tissue, cartilage or calcified zones can be seen microscopically. Pleomorphic adenoma is most commonly seen in the parotid gland. Most of the tumors arise from the tail or the superficial lobe, but the deep lobe can be involved (Fig. 13.33).

Fig. 13.33. Pleomorphic adenoma of the right and left parotid glands
For the minor glands, the most common site is the palate, followed by cheek, lip and pharynx (Fig. 13.34).

Fig. 13.34. Pleomorphic adenoma of the minor gland of the soft palate
Adults are predominantly affected. The tumors grow slowly. They usually range from 2 to 5 cm in greatest dimension (Fig. 13.35), although in some cases they may achieve a size of 15–20 cm. Pleomorphic adenoma is usually round or ovoid painless, well-circumscribed mass with smooth or lobulated surface.

Fig. 13.35. Pleomorphic adenoma of the left submundibular gland
The connective tissue capsule is thin, delicate and may be incomplete. It has occasional projections into the surrounding salivary gland tissue, which are considered to be the main source of the tumor recurrence (Fig. 13.36) There is an incidence of malignant degeneration in pleomorphic adenomas in 3–7 % of cases (usually in longstanding tumors).

Fig. 13.36. Pleomorphic adenoma of the parotid gland, macro-preparation
Treatment of pleomorphic adenoma is determined by its clinical and histological peculiarities: incomplete capsule and high recurrence rate. It usually includes complete surgical excision of the affected gland. If the parotid gland is involved, superficial or total parotidectomy with standard facial nerve dissection and preservation are the methods of choice. Attempts at enucleation of the tumor from within its capsule will inevitably leave viable tumor cell nests and predispose to the multifocal recurrence. This rate in cases of simple enucleation is 25–50 %.
Adenolymphoma
Adenolymphoma (Warthin tumor, papillary cystadenoma lymphomatosum, cystic papillary adenoma) is a benign tumor, which consists of epithelial and lymphoid structures. Adenolymphoma is the second most common salivary tumor, comprising 2–6 % of all salivary tumors. In the majority of cases it affects the parotid gland, especially the tail of the parotis (Fig. 13.37). In some cases (10 %) a bilateral localization is observed.

Fig. 13.37. Adenolymphoma
of the right parotid gland
Adenolymphoma has a male predominance and usually occurs in the sixth and seventh decades of life. This lesion presents as a slow-growing, soft, painless mass with a smooth surface. It is well encapsulated and usually contains multiple cysts or one big cyst (Fig. 13.38).

Fig. 13.38. Adenolymphoma, macropreparation
The tumour is thought to arise from the entrapped salivary epithelial rests within developing lymph nodes. Malignant transformation is not typical. Recurrence rate in simple enucleation is 2–5 %.
The treatment of this lesion is surgical excision. In spite of low recurrence rate, a superficial parotidectomy is the treatment of choice, because the accurate diagnosis of adenolymphoma can be confirmed only by pathohistological investigation.
Oncocytoma (oxyphil adenoma)
Oncocytoma is a rare monomorphic salivary tumor, characterized by benign proliferation of oncocytes (cells of the salivary ducts). Oncocytomas are rather uncommon, they account for 1 % of all salivary gland tumors. Usually they are observed in patients older than 50 years (Fig. 13.39), more often in women than in men. The parotid gland is the most common site for this tumor (more than 80 % of cases). Another possible localization is the submandibular gland, while affection of the minor salivary glands is very rare. Oncocytomas manifest as small (less than 5 cm), firm or elastic, slow-growing, spherical, painless, masses, with a distinct capsule. The color of the neoplasm is dark red or brown. The prognosis in cases of radical excision is good. Recurrence rate is less than 10 %. Malignant transformation is uncommon.

Fig. 13.39. Oncocytoma
of the right parotid gland
Other types of salivary gland adenomas are rare, less than 1 % of all salivary tumors. Among them canalicular adenoma, basal cell adenoma, intraductal papilloma and others. They usually manifest as small, movable, painless masses with a comparably smooth surface. They are seen mostly in older patients and have no specific clinical signs. The diagnosis in vast majority of cases is the result of pathomorphological investigation.
Malignant epithelial tumors of the salivary glands
Malignant salivary gland tumors are observed less frequently as benign. The vast majority of malignant salivary gland tumors occur in adulthood and there number significantly increases in older groups. Malignant tumors are more common in the submandibular gland and minor salivary glands: up to 50 % of tumors arising from these glands are malignant.
The etiology of malignant salivary gland tumors is not exactly known. However, long history of smoking, family predisposal, head and neck irradiation and long-standing benign tumors are considered to be important risk factors.
The six most common types of malignant salivary glands tumor are mucoepidermoid, acinic cell carcinoma, adenoid cystic carcinoma, adenocarcinoma, squamous cell carcinoma and malignant transformation of pleomorphic adenoma.
It is often hard or even impossible to differentiate benign and malignant salivary gland tumors, especially in early stages. In these cases histological approval of the diagnosis is necessary. At the same times there are clinical signs, perculiar to the malignant salivary gland tumors, which are of great importance (Table 13.1).
Table 13.1. Differential diagnosis of benign
| Benign salivary gland tumors |
Malignant salivary gland tumors |
Slow-growing
Soft or rubbery consistency
Do not ulcerate
No pain
No associated nerve signs
No methastases
Do not invade surrounding tissues Fixation to surrounding structures is not typical |
Sometimes fast-growing
Sometimes have more hard consistency
May ulcerate
Can be painful
May affect cranial nerve
(facial nerve weakness, rarely affection of lingual or hypoglossal nerves)
Can form regional and distant metastases (lymphadenopathy in the neck, methastases to the bones, lungs, liver) May invade bone, or masticatory muscles causing trismus
Fixation to the mastoid tip or to the skin may be present |
| In their early stages, benign and malignant salivary gland tumors cannot be distinguished clinically. |
|
The treatment of the malignant salivary gland tumors is radical surgical excision, if the procedure is possible. Depending upon the size of the tumour, its localization and histology, this may require removal of the facial nerve and other surrounding structures, including the ear and petrous part of the temporal bone, and part of the mandible, neck dissection and limphadenectomy. Postoperative radiotherapy may be necessary. Radiotherapy can be used as mono therapy as a palliative treatment.
Mucoepidermoid tumor
Mucoepidermoid tumor is a malignant neoplasm arising from the ductal epithelium. It is considered to be the most common malignant salivary gland neoplasm, affecting both major and minor salivary glands. This tumor can have low-grade or high-grade malignant potential depending on its histology. The clinical aggressiveness of the tumor is determined by the ratio of mucus and squamous cells (tumors with a high mucous content tend to have a lower malignant potential).
Low-grade mucoepidermoid tumors behave like benign tumors. They are usually slow growing and nonmetastasizing. High-grade mucoepidermoid tumors can exhibit aggressive growth and invasion resulting in widespread metastasis to cervical lymphatic nodes, lungs, liver, bone, and, finally, death of the patient.
The most common clinical presentation is a slowly growing painless mass of several years duration clinically mimicking a pleomorphic adenoma or other benign tumor. Pain, tenderness or rapid enlargement are seen only in high-grade lesions.
Treatment includes radical surgical excision (adenectomy or block resection). If neck nodes are affected, then a typical neck dissection is also included. In tumors that are histologically high-grade malignances, postoperative radiotherapy is often applied. Prognosis depends on the histological type and stage of the tumor, with 5-year survival rate ranging from 20 to 90 %. Tumors of the submandibular gland have a worse prognosis than tumors of the parotid gland.
Acinic cell carcinoma
Acinic cell carcinoma is a rare low-grade carcinoma, arising from the boundary zone between the acinar and intercalated ducts. It is often considered as an intermediate tumor. Depending on its histological pattern, it can behave in a relatively benign or aggressive malignant fashion.
It is more common in males, and the most common site is parotid gland (80 %). Tumor manifests as a slow growing, well-localised lesion, that is not fixed to the surrounding soft tissue or skin. Pain symptom and facial nerve paresis are observed rarely in a small number of patients with this tumor. Treatment includes complete surgical excision and irradiation in certain cases. Prognosis is generally good, with a 5-year survival of over 80 %.
Adenoid cystic carcinoma
Adenoid cystic carcinoma is the most common malignancy of the submandibular gland and minor salivary glands. It is also the second most common salivary gland cancer overall.
There are three histological types of the tumor: tubular, cribriform and solid. Solid type has the worst prognosis. The tumor is also characterized by perineural spread, repeated recurrences and metastasis via the blood stream. Although this tumor is very slow growing, its relentless course, gives low long-term survival rates.
Clinically adenoid cystic carcinoma manifests as a slow-growing mass. Pain may be present but it is not an obligatory sign. Other symptoms include fixation to adjacent tissues and paraesthesia or paralysis associated with perineural invasion, typical to this tumor. Clinical and radiologic examination of this tumor frequently underestimates its true extent. Ulceration may occur in some cases, and it is more common in intraoral tumors.
Treatment includes wide excision and postoperative radio-therapy aimed to increase local control of the disease. In cases of pereneural invasion the facial nerve should be sacrificed. If neck nodes are affected then a neck dissection is also required.
Prognosis depends on histological type and also on the length of follow-up. Perineural spread is a bad prognostic sign for both local recurrence and distant metastasis. Although it is sometimes very difficult to cure adenoid cystic tumours, they tend to be very slow growing and the patient can live for many years, even in cases of lung and liver metastases.
The infiltrative nature of this lesion and the frequency of perineural involvement with spread along the nerve mandate wide resection margins, and follow-up of 15 to 20 years is required as late recurrences occur.
Adenocarcinoma and squamous cell carcinoma
Adenocarcinoma and squamous cell carcinoma of the salivary gland are very aggressive tumors, which usually occur in elderly patients. Signs and symptoms include a painful rapidly enlarging tumor, invading surrounding tissues with facial nerve palsy present in 50 % of cases. Ulceration of the skin and metastases are often seen at the late stages. The prognosis in these cases is poor, with 5-year survival rate of less than 35 %. Treatment includes wide surgical excision, often combined with neck dissection and postoperative radiotherapy.
Malignant change in pleomorphic adenoma
Malignant change in pleomorphic adenoma arises from a pre-existing pleomorphic adenoma. The parotid gland is the primary site of this tumor in more than 80 % of cases, followed by the submandibular and minor salivary glands.
The presence of malignancy often manifests by onset of new symptoms. Among them – sudden and rapid growth of an existing tumor, development of pain syndrome, paresis of the facial nerve. Malignant transformation is usually seen in long-standing tumors or in recurrences after inadequate excision. Local and distant metastases (to the lungs, bones, especially vertebral column, and liver) are often found in clinical examination.
Histologically, malignant change in pleomorphic adenoma is characterized by carcinomatous areas adjacent to the benign cellular picture of the remainder of the tumor.
Treatment is the same as for the other malignant salivary gland tumors. Prognosis is poor, especially in cases with marked facial nerve palsy. 5-year survival rate is 15–20 %.
Nonepithelial tumors of the salivary glands
Noepithelial tumors develop in the major salivary glands from soft tissue structures (nerves, blood vessel, lipoid, lymphatic or connective tissue). In some cases they spread to the salivary gland from the adjustment tissues. The parotid gland is the most common site for nonepithelial tumors.
The most common tumors of this group are hemangioma, lymphangioma, lipoma, fibroma, neurinoma, lymphoma.
Although the clinical signs and treatment strategies for salivary glands nonepithelial tumors in general correspond to the soft tissue tumors of other localizations, there are some peculiarities in this group.
Hemangiomas. Two forms of hemangiomas, capillary and cavernous, may develop in the major salivary glands. These are vascular tumors directly involving the parotid or submandibular glands. The capillary type is the most prevalent tumor of the parotid gland which may be present at birth or first seen in childhood. These hemangiomas have no capsule and are formed by purple, spongy, lobular masses that infiltrate salivary gland tissue. The salivary gland structure is largely replaced by angiomatous tissue among which glandular elements can be found. They commonly infiltrate neighboring structures, expanding through the capsule of the salivary gland. The diagnosis is made based on clinical features. CT scanning with intravenous contrast may be helpful in demonstrating the vascular nature of these neoplasms. Cavernous hemangiomas, which present in an older age group, usually do not show spontaneous regression and their treatment is a difficult problem. In majority of cases they require surgical resection of the affected gland, embolization, or both.
Lymphangiomas are mostly observed in infants and children. They are spongy, multiloculated masses with a yellowish or bluish surface and are formed by endothelial-lined spaces. Usually, they manifest as painless masses that may involve parotid glands, submandibular glands, or both. Diagnosis is made based on clinical findings. Surgical excision with preservation of the vital structures is the treatment of choice.
lipomas are relatively uncommon in the major salivary glands. They derive from the fat cells and manifest as soft, mobile, painful well-demarcated, bright-yellow masses. They are slow-growing tumors with an average diameter of 3 cm. Treatment is surgical excision. In rare cases adenectomy is preferable.
Lymphomas. The most common non-epithelial malignant tumor of the salivary glands is lymphoma. In some cases they develop as a complication of Sjogren’s syndrome or salivary lymphoepithelial lesion. In other cases salivary gland lymphoma is the first sign of widespread disease. Such a possibility must always be investigated since the prognosis is heavily dependent on the tumour’s stage. The presence of persistently enlarged or nodular parotid or submandibular glands, regional or generalized lymphadenopathy, pulmonary infltrates, hepatomegaly, vasculitis, or a monoclonal gammopathy may be signs of malignancy. If a diagnosis of lymphoma is made, chemotherapy appropriate for the stage and type of lymphoma must be administered.
Metastatic disease of the salivary gland
Carcinomas of different origin, melanoma and occasionally other tumours can metastasise to the salivary glands. Lymphatic nodes within the parotid gland are commonly affected. Metastases to the salivary glands can sometimes resemble primary salivary gland tumors. Diagnosis may depend on finding a primary tumor site or precise pathohystological examination. For patients with metastases to the parotid gland, all potential cutaneous and mucosal sites need examination. This includes fiberoptic examination of the nasopharynx and oropharynx. Particular care is necessary when inspecting potential cutaneous sites, since cutaneous malignancies may be small relative to the size of regional metastases, especially in cases of melanoma. Inconspicuous lesions hiding in the hair, behind the ear, nasal vestibule, and in the external auditory canal are easily overlooked.
Treatment depends on the histological type and stage of the primary tumor. In most cases of salivary glands methastatic affection the prognosis is poor in view of the tumor dissemination.
Tumor-like lesions of the salivary glands
Tumor-like lesions of the salivary glands include sialadenosis, oncocytosis (diffuse oncocytosis and focal adenomatous oncocytic hyperplasia), necrotizing sialometaplasia (salivary gland infarction), benign lymphoepithelial lesion (chronic myoepithelial sialadenitis), salivary duct cysts (mucoceles of the minor salivary glands of extravasation or retention type, cysts of the major salivary glands, ranula and dysgenetic polycystic disease of the parotid gland), chronic sclerosing sialadenitis of the submandibular gland (Kuttner tumour), and cystic lymphoid hyperplasia in AIDS. All these diseases in some cases can mimic the true neoplasm and are usually associated with higher risk for the tumor development.
Mucocele
Mucocele is a tumor-like lesion of the salivary glands, which is a result of obstruction of the salivary outflow tracts and extravasation of mucus into the surrounding tissues. Salivary ducts, especially those of the minor salivary glands, are occasionally traumatized, commonly by lip biting. Subsequent saliva production may then extravasate beneath the surface mucosa into the soft tissues. Saliva leaking from a damaged duct into the superficial surrounding tissues excites an inflammatory reaction. Over time, the pools of saliva form a rounded collection of viscous fluid, surrounded by compressed connective tissue without an epithelial lining. As it has no epithelial lining, mucocele is not a true cyst.
Mucoceles mainly affect the minor salivary glands, particularly of the lip. Other typical sites are buccal mucosa and sublingual gland (ranula). Retention cysts of the minor salivary glands are usually superficial and rarely larger than 1 cm in diameter. They manifests as rounded, soft, compressible mass. Later, they become hemispherical, fluctuant and bluish due to the thin wall. Cyst is filled with viscous clear yelowish or blue-gray mucus (Fig. 13.40). Patients may relate a hystory of cyst rupture followed by lession reccurence.

Fig. 13.40. Mucoceles of the anterior lingual gland
Ranula
Ranulas are large retention cysts occurring in the sublingual gland. Their pathogenesis and histological structure is usually the same as in other salivary retention cysts. The term “ranula” has its derivation traced to the oral anatomy of the frog.
The origin of a ranula is due to obliteration of one of the minor ducts of the sublingual gland, while the main excretory duct remains patent. Extravasation of saliva moves throughout the sublingual gland and into the submucosal space via hydrostatic pressure as the sublingual gland continues to produce saliva. The extravasated mucus can gradually spread around or through the mylohyoid muscle into the submental or submandibular spaces.
Simple ranulas are located above the mylohyoid muscle in the sublingual space. Complex or plunging ranulas develop when the lesion extends beyond the level of the mylohyoid muscle into the submandibular or submental space. Plunging ranula may be quite large and extend to the inferior aspect of the neck or the chest wall (Fig. 13.41).

Fig. 13.41. Plunging ranula of the right sublingual gland (superior and inferior parts)
The ranula clinically manifests as a painless mucus pseudocyst on the floor of the mouth. Usually they have 2 or 3 cm in diameter, but occasionally extend across the whole of the floor of the mouth. They are soft, fluctuant on bimanual palpation, painless and bluish in color. They usually enlarge slowly but may become large enough to elevate the tongue and interfere with speech or mastication.
The usual presentation of a plunging ranula is a soft, compressible mass in the submandibular or submental region. These may be initially misdiagnosed as sialadenitis or a salivary tumor. Transillumination of the mass may be feasible in the larger ranula. Intraoral examination should demonstrate an intraoral component combined with the cervical component.
Magnetic resonance imaging (MRI) in this cases can show herniation of the sublingual tissue and cystic material through the mylohyoid muscle. T1–weighted images are usually low enhancing while T2–weighted images are bright. The use of ultrasound of the neck in the evaluation of a plunging ranula may also reveal deficiencies in the mylohyoid muscle with herniation of the sublingual gland. With computed tomography (CT), a plunging ranula can be readily identified preoperatively as a cystic unilocular mass in the suprahyoid anterior neck.
Cysts of the parotid gland. Retention cists that occur in the parotid gland are more common in men often in their seventh or eighth decades. They present as a slow growing swelling in the affected gland, which on aspiration reveals a clear colored fluid. They also often completely disappear on aspiration. In the majority of cases the diagnosis is only made when the cyst is removed. It is not always easy to distinguish it from cystic form of adenolymphoma preoperatively.
Treatment of the salivary glands cysts
Treatment of a small superficial mucocele consists of excision of the mucocele and the associated minor salivary glands that contributed to its formation. If the damaged minor salivary gland has not been removed recurrence of the disease is very likely. An operation is usually performed under the local anesthesia. Infiltration or mental nerve block can be used. It is advised to delineate the boundaries of the mucocele first because the local infiltration of anesthetic may distort the anatomy.
An elliptical superficial incision through the mucosa is made around the mucocele. Careful dissection around the cyst may permit its complete removal. The regional associated minor salivary glands are also removed and sent for pathohistologic evaluation. Hemostasis is achieved with an electrocautery device and the wound is closed with absorbable suture.
The recurrence rates of mucoceles after surgical removal are not very high and usually they are caused by incomplete removal or repeat trauma to the minor salivary glands.
In cases of ranula different treatment modalities can be used. The usual treatment is marsupialization, in which a portion of the oral mucosa of the floor of the mouth is excised, along with the superior wall of the ranula. Subsequently, the ranula wall is sutured to the oral mucosa of the floor of the mouth and allowed to heal by secondary intention.
The preferred treatment for recurrent or plunging ranulas is excision of the ranula and sublingual gland via an intraoral or extraoral approach (Fig. 13.42).

Fig. 13.42. Planing and extraoral approach during the operation of the plunging anulas
In this cases the general anesthesia with nasal intubation is often required. An intraoral approach is made with an incision along the axis of the gland. The submandibular duct is identified, either by dissection or following cannulation with a probe to prevent its injury during the resection. The sublingual gland and the cyst are dissected in a subcapsular space. At the posterior pole of the gland the lingual nerve is identified as it crosses the Wharton’s duct and is preserved. The sublingual gland is dissected from anteriorly, and the final excision is the posterior pole after visualizing the lingual nerve. After completion of the dissection and removal of the gland, careful hemostasis is achieved. Closure of the wound is performed with absorbable sutures in a single layer.
Some patients plunging ranulas with may require an incision on the neck for exposure and excision of the ranula. This incision is performed 2,5 cm below the inferior margin of the mandible. The submandibular gland is identified and carefully mobilized away from the ranula. In addition to identifying the submandibular duct and lingual nerve during the dissection, in this cases care must be taken not to rupture the pseudocyst as the ranula is followed through the mylohyoid muscle. Completion of the posterior and inferior extent of the plunging ranula is performed after careful identification of the facial artery and veins to prevent bleeding in the operative site. After the cyst removal incision is closed by layered suture. In cases when adenocystectomy is performed the recurrences are rather uncommon.
Complications of the surgical treatment for retention cysts of the salivary glands include recurrence, injury of the lingual or hypoglossal nerves, Wharton’s duct injury, bleeding and development of infection.
Benign lymphoepithelial lesion
Benign lymphoepithelial lesion is the group of the diseases which manifest as a diffuse enlargement of all or part of the salivary glands, or as a disrete mass. Histologically, the lesion is composed of a diffused, well-organized lymphoid tissue and lymphocytic interstitial infiltrate with obliteration of the acinar structures. Benign lymphoepithelial hyperplasia is observed in Sjogren’s syndrome, Mikulich disease, some forms of chronic parotitis.
Sjogren’s syndrome
Sjogren’s syndrome is a multisystem disease with a variable presentation. Sjogren’s syndrome characterized by xerostomia (dry mouth), keratoconjunctivitis sicca (dry eyes), and an associated connective tissue disorder, most commonly rheumatoid arthritis.
Sjogren’s syndrome is an autoimmune disease with primary connective tissue affection and a variety of immunological signs. Histological changes in salivary glands include periductal infiltration by proliferating limphocites. Infiltration progressively spreads through the glandular tissue, causing the destruction of secretory acini. Finally the total lymphocytic replacement of the normal glandular elements is possible. A decreased function of both the major and minor salivary glands results in marked xerostomia.
Sjogren’s syndrome has a strong female predilection (9 : 1), with a mean age of 50 years. It affects 15 % of patients with rheumatoid arthritis, possibly 25–30 % of patients with lupus erythematosus and a variable proportion of patients with other connective-tissue diseases (Fig. 13.43).

Fig. 13.43. Sjogren`s syndrome, deformation of the joints are caused by polyarthritis
Generally, the first symptoms to appear are arthritic complaints, followed by ocular symptoms, and, late in the disease process, salivary gland symptoms. Main oral effects of Sjogren’s syndrome are discomfort, difficulties with eating or swallowing, disturbed taste sensation, disturbed quality of speech, predisposition to infection. All this results from decreased saliva secretion and xerostomia.
In the early stages, the mucosa may appear moist but salivary flow measurement shows diminished secretion. In established cases the oral mucosa is obviously dry and red in color. The tongue is typically red; its dorsum becomes lobulated with a cobblestone appearance.
With diminished salivary secretion the oral flora changes and candidal infections are common. They are the main cause of soreness of the mouth in Sjogren’s syndrome and cause generalised erythema of the mucosa, often with angular stomatitis. Plaque accumulates and there may be rapidly progressive dental caries. The most severe infective complication is suppurative parotitis.
Swelling of the parotid glands in Sjogren’s syndrome usually shows no inflammation and is rarely painful. But in cases of infection development (suppurative parotitis) parotid swelling becomes hot, tender with red, shiny overlying skin. Parotid swelling appearing years after the onset strongly suggests lymphomatous change. An increased incidence of malignancy, especially non-Hodgkin’s lymphoma, associated with Sjogren’s syndrome determines the significance of this condition to surgical practice. These patients should therefore be followed-up to rule-out a lymphoma.
Sjogren’s syndrome can also have serious ocular effects associated with decrease in tear secretion. Among them failure of foreign particles clearance from the cornea and conjunctiva, gritty sensation in the eyes and inflammation (keratoconjunctivitis sicca) with a risk of impairment or loss of sight.
The diagnosis of Sjogren’s syndrome is suggested by the patient’s complaints and by a variety of abnormal immunologic laboratory tests. The oral component of SS may be diagnosed using salivary flow rate studies and sialography, but the use of a labial minor salivary gland biopsy currently is considered to be highly accurate in aiding the diagnosis. The histopathologic changes seen in the minor glands correlate closely with those in the major glands: biopsy shows the periductal lymphocytic infiltrate.
Syalography shows the typical “snowstorm” appearance (so-called sialectasis). Imunological tests shows the increased levels of rheumatoid factor and Ro (SS-A) and La (SS-B) antibodies.
There is no specific treatment for Sjogren’s syndrome apart from symptomatic treatment and treatment of the underlying connective tissue disease present. As the salivary gland damage is irreversible, dryness of the mouth can be relieved to some degree by providing artificial saliva. Cholinesterase inhibitors such as pilocarpine are also recommended to stimulate salivary salivary flow from the remaining functional salivary gland tissue. All other factors contributing to the xerostomia (for example medications) are to be checked, symptomatic treatment for mucosal diseases and caries control are necessary. Regularly follow up for possible development of ascending parotitis or lymphoma is one of the main principles in Sjogren’s syndrome management.
Ophthalmological examination is particularly important to exclude keratoconjunctisitis sicca, which is symptomless in its early stages. The artificial tears and symptomatic therapy are prescribed for the dry eyes.
Mikulicz disease
Mikulicz disease is a rare pathological condition, characterized by gradual enlargement of salivary and lachrymal glands. Histologically the signs of benign lymphoepithelial hyperplasia are observed. Affection of eyes and salivary glands is not associated with any connective tissue disease. Mikulicz disease is more frequent in females than in males, and its peak incidence is in the fourth and fifth decades. Occasionally, both parotids are involved. Growth of this tumor is slowly progressive, and usually painless. In rare cases it gives rise to pain around the ear or the retromandibular area. There is no specific treatment for this condition. Symptomatic treatment and follow up observation is performed by oral surgeon, ophthalmologist and rheumatologist.
Sialosis (Sialadenosis)
Sialosis is a non-inflammatory salivary gland disease caused by metabolic and secretory disorders of the gland parenchyma, accompanied by recurrent, usually painless, bilateral swelling of the glands due to acinar enlargement. Histologically, there is hypertrophy of serous acini, oedema of interstitial connective tissue and fatty infiltration on the late stages.
Sialosis has an equal incidence in both males and females and occurs most commonly in the fourth to seventh decades of life. The disease is associated with some underlying conditions.
Sialosis often occurs in patients with a history of alcohol abuse. Gland enlargement has been also described in most endocrine diseases but it is particularly linked to diabetes mellitis. Other important endocrine conditions include thyroid disease, gonadal dysfunction and pregnancy. Sialosis is commonly seen in chronic starvation and is thought to be linked to the deficiency of proteins and vitamins. The nutritional causes of the sialosis are also cirrhosis, anorexia, kwashiorkor, and pellagra. Dysfunction of the autonomic nervous system can give rise to sialosis and this is most commonly seen in people taking drugs that affect the autonomic nervous system, such as some antihypertensive drugs. Other neurochemical causes include vegetative state, chronic intoxication with lead, mercury, iodine. In cases when the direct cause of the sialosis is not find out it is called idiopathic.
Clinical manifestation of the disease is usually associated with recurrent painless enlargement of both pairs of the major salivary glands, espetially the parotids and less commonly the submandibular glands (Fig. 13.44). Minor salivary gland involvement can be seen rarely.

Fig. 13.44. Sialosis of the right parotid gland
The persistence of sialosis is dependent on the severity and duration of the underlying disease.
The gland enlargement can persist from weeks to months. In some cases the infection process may arise in affected glands and alter the clinical picture.
The diagnosis is made upon the history and clinical appearance associated with an underlying cause. A parotid biopsy is needed occasionally, and histology will then show acinar enlargement.
The treatment for sialosis is usually conservative. It always includes the treatment for underlying disease, patogenetic and symptomatic therapy for salivary gland pathology. However even with treatment of the underlying condition, it is common for the parotid enlargement to persist. In this cases surgical treatment (parotidectomy) may be performed for cosmetic purposes.
Oncocytosis
Oncocytosis is a diffuse or multifocal proliferation of oncocytes within the major salivary glands. Oncocytosis occur usually in the sixth decade more frequently in males. The parotid gland is the most common (more than 80 %) site, while the remainder arise almost exclusively in the submandibular gland. Clinically oncocytosis presents as unilateral or bilateral salivary gland enlargement, typically of the parotid gland. Multifocal nodular oncocytic hyperplasia is far more common than difuse oncocytosis. Difuse oncocytosis presents as a difuse enlargement while multifocal nodular oncocytic hyperplasia has at least two nodules within the salivary parenchyma. In patients with oncocitosis the true neoplasms oncocytomas can arise rathe frequently. They may be solitary, bilateral, or arise in the setting of multinodular oncocytic hyperplasia. The pathogenesis of oncocytosis and is unclear, but is likely a progression from the age-related precursor of oncocytic metaplasia. The disease progress very slowly and no specific therapy is necessary in the majority of cases. Surgical interventions (salivary gland biopsy) are performed to rule out other tumors, especially malignant neoplasms.
Cystic lymphoid hyperplasia of salivary glands in AIDS
HIV-associated salivary gland disease includes lymphoepithelial lesions and cysts involving the salivary gland tissue and/or intraglandular lymph nodes. Young males are predominantly affected. Main clinical signs include xerostomia, cystic parotid gland swellings usually associated with generalised lymphadenopathy. The histological features are essentially similar to those of Sjogren’s syndrome, apart from gross cyst formation. However, autoantibodies typical of Sjogren’s syndrome are not revealed by immunological tests. The treatment HIV salivary gland cysts respond to highly active retroviral therapy. The symptomatic therapy for xerostomia is also necessary.
Kuttner tumor
Kuttner tumor, known also as chronic sclerosing sialadenitis, is a chronic inflammatory disease of the salivary gland. Clinically, it produces a firm swelling of the glands and may be difficult to distinguish from neoplasia. The disease is very rare and affects almost exclusively submandibular glands. The diagnosis can only be made histologically and should not be difficult if the pathologist is aware of the condition’s existence. Adequate treatment is excision of the mass, usually carried out diagnostically.
Cysts of the jaws
A cyst is a pathological cavity that is usually lined with epithelium and which contains fluid or semi-fluid. Most jaw cysts are epithelial and odontogenic origin. Usually they grow slowly and expansively. Initially cysts of the jaws are often symptom-free and in this stage they may be found by chance on routine radiography. Radiologically they form sharply-defined radioluciencies with smooth borders. They differ mainly in relationship to teeth, radiographic features and pathomorphology. Cysts are much more common than true neoplasms of the jaw bones Depending on their origin and pathomorphological characteristics they are classified as following.
A. Non-epithelial cysts:
- Solitary (simple) bone cyst
- Aneurysmal bone cyst
B. Epithelial Developmental cysts:
- Odontogenic:
- Gingival cyst.
- Dentigerous (follicular) cyst.
- Eruption cyst.
- Odontogenic keratocysts.
- Non-odontogenic:
- Nasopalatine duct (incisive canal) cyst Nasolabial cyst.
- Globulomaxillary cyst.
C. Inflammatory (radicular) cysts.
Aneurysmal bone cyst
Aneurismal bone cyst is a tumor-like lesion, associated with trauma or vascular disorders in bone; it is neither a cyst nor an aneurysm. Etiology and pathogenesis of this lesion are still unclear. Possible mechanisms for the formation of the aneurysmal bone cyst include alterations in local hemodynamics leading to venous engorgement, resorption, and replacement with connective tissue and osteoid; futile attempts at repair of a hematoma and microcyst formation secondary to cellular edema.
Aneurysmal bone cysts of the maxilla-facial area are very rare. They occur in jaws of people of all ages, but they are more common in younger patients. Aneurysmal bone cysts are more likely to occur in the mandible than in the maxilla. They may displace but usually do not resorb the teeth, nerve disturbances are not typical. The radiographic appearance is described as cystic, honeycomb, or soap bubble radiolucent lesion with eccentric expansion. Cortical bone may be thinned or destroyed, and a periosteal reaction may be present.
Histologically, the aneurysmal bone cyst reveals a fibrous connective tissue stroma with many cavernous or sinusoidal blood-filled spaces. Young fibroblasts are present throughout the stroma, and multinucleated giant cells are scattered throughout the lesion.
Treatment of the aneurysmal bone cyst includes complete removal with aggressive curettage of the underlying bone. Excellent exposure to facilitate this treatment is necessary because these lesions may bleed copiously, and timely but thorough removal of the lesion helps to decrease blood loss. Failure to completely remove all traces of the lesion carries a significant risk of recurrence. For recurrent lesions some authors recommend combination of excision with cryosurgery, while other authors advocate block resection followed by reconstruction with bone graft.
Traumatic bone cyst
The traumatic bone cyst also is known as solitary bone cyst, hemorrhagic cyst, extravasation cyst, simple bone cyst, and idiopathic bone cavity.
The traumatic bone cyst is a rare tumor-like lesion of the jaw bones. This cyst is not a true cyst in so far as it has no epithelial lining. The etiology of these cysts is not clearly defined, although several mechanisms have been proposed. The most accepted theory is that these lesions originate from intramedullary hemorrhage caused by trauma. In these cases, failure of organization of the blood clot occurs followed by subsequent degeneration of the clot, eventually leading to an empty bone cavity. Restricted venous drainage leads to increasing edema, which in turn causes continued resorption of trabeculae and expansion of the lesion in the spongious bone. Expansion of the cyst stops when cortical bone is reached, thus these lesions are not characterized by any cortical damage. The cyst cavity are generally either empty or filled with a small amount of straw-colored fluid. Histologically, they have a thin connective tissue membrane lining or no lining at all.
The lesion most commonly is found in young persons, and the mental area or body of the mandible is the most typical localization. Clinically they are usually asymptomatic and cause no expansion of the bone. In majority of cases they are found out on radiographs taken for other purposes as incidental findings. It is also not unusual that some patients are unable to recall any trauma to the involved jaw.
Radiographically, these lesions look as smoothly outlined radiolucencies that scallop around the roots of the of the lower molar and premolar teeth. They do not displace teeth or resorb roots, and the lamina dura is intact. In radiographic examination the outline of the radiolucency is less well defined than would be obtained from other cysts. They may range from very small (< 1 cm) to very large (involving most of the mandible). Any signs of cortical involvement are not typical.
Treatment includes surgical intervention to establish a diagnosis, which is made upon finding an empty cavity. A curettage of the cyst wall is than performed to fill the cavity with blood. Soft tissues are closed, and the lesion tends to heal without further intervention.
Nasopalatine cysts
Nasopalatine cysts are also known as cysts of the incisor canal. These cysts arise from epithelial remnants within or near to the nasopalatine foramen. They are classified as fissural cysts, and they are one of the most common types of fissural cysts of the jaws.
Clinical features
Presence of a midline anterior palatine swelling is the only usual clinical finding. They may become infected and in this cases nasopalatine cysts cause pain and overlying tenderness. These cysts grow slowly, but in some cases may grow to a considerable size. In many cases cysts are diagnosed through chance by radiographs of the teeth in this region. It can be difficult when such radiolucencies are found on routine radiographic assessment of the central incisors. The radiographic image of the nasopalayinal cyst is a round or inverted pear-shaped radiolucency with radio-opaque margins. When they are large, they can cause separation of the central incisor roots, but the laminae dura of the teeth remain intact.
If there is doubt whether the cyst is a radicular cyst related to one or other incisor, pulp testing can be carried out and close examination of the apices radiographically should show an intact lamina dura.
Treatment. Nasopalatinal cysts are treated by cystectomy. Enucleation is carried out with a palatal flap taken around the gingival margins of the premolars on one side to the premolars of the other. After enucleation, interdental interrupted sutures are used to replace the flap and in larger cysts. It is sometimes useful to have constructed a palatal plate from preoperative impressions to support the flap and prevent the formation of a painful haematoma.
Nasolabial cyst
This is a fissural cyst that is formed by cystic degeneration of epithelium from the lower part of the nasolacrimal duct during embryological development. Clinically, they may present as painless swellings in the nasolabial fold, where they may be palpated either externally on the skin surface or intraorally high in the buccal sulcus anteriorly. Radiographically, although they are not intrabony cysts they may, if they attain a reasonable size, cause a depression of the radio-opaque margin of the floor and lateral wall of the nose, which is best viewed by an oblique anterior occlusal radiograph. Treatment is surgical enucleation.
Globulomaxillary cyst
This cyst is a rare fissural cyst which develops between roots of the vital upper lateral incisor and canine teeth. Globulomaxillary cysts grow slowly, but in some cases may reach a considerable size. Clinically they are asymptomatic unless infected. On late stages they can be palpated as a firm swelling in the buccal fold caused by expansion of the cortical plate. Sometimes retention or displacement of the upper lateral incisor or canine is observed.
Radiologically globulomaxillary cyst appears as a lucent area, in shape of the inverted pear. Deviation of roots is typical signs, but the laminae dura of the teeth remain intact (Fig. 13.45).

Fig. 13.45. The globulomaxillary cyst
Treatment of choice for globulomaxillary cysts is cystectomy, with recurrence rate being very low.
Dentigerous cysts
These cysts are developmental odontogenic cysts, which arise when cystic transformation occurs in the epithelium of the dental follicle. Dentigerous cyst are seen around unerupted tooth, most commonly in the third molar areas both upper and lower. Other common associations are with maxillary canines, and mandibular second premolars. Although dentigerous cysts occur over a wide age range, they are most commonly seen in second and third decades of life.
The histologic features of dentigerous cysts may vary greatly depending mainly on whether or not the cyst is inflamed. In the noninflamed dentigerous cyst, a thin epithelial lining may be present with the fibrous connective tissue wall loosely arranged. In the inflamed dentigerous cyst, the epithelium commonly demonstrates hyperplastic rete ridges, and the fibrous cyst wall shows an inflammatory infiltrate.
Most dentigerous cysts are small asymptomatic lesions that are discovered incidentally on routine radiographs. Although some may grow to considerable size, move teeth and cause bony expansion that is usually painless until secondary infection occurs. These cysts grow slowly and cause bony expansion only at late stages. If the cortical layer is destroyed, a soft fluctuant swelling over the area of the unerupted tooth will develop. Large dentigerous cysts are often associated with the significant risk for pathologic jaw fracture.
Radiographic imaging and, sometimes, aspiration are the main diagnostic procedures for dentigerous cysts. Radiographically, the dentigerous cyst presents as a welldemarcated unilocular radiolucency, often with a sclerotic border (Fig. 13.46; 13.47).

Fig. 13.46. The dentigerous cyst

Fig. 13.47. The dentigerous cyst of the mandible of the mandible from the 45 tooth from the 32 tooth
Since the epithelial lining is derived from the reduced enamel epithelium, this radiolucency surrounds the crown of the tooth, which is projected into the cyst cavity. The radiographic differentiation between a dentigerous cyst and a normal dental follicle is based merely on size. A very large dentigerous cyst in the lower third molar area can displace the wisdom tooth and may require to be differentiated from other lesions such as a keratocyst or ameloblastoma.
Treatment
Treatment will either be enucleation along with extraction of the unerupted tooth or cystotomy (marsupialisation). Histopathologic examination of the cyst wall is obligatory in both cases. Cystotomy is the method of choice if it is hoped to encourage eruption of the buried tooth, but it is only possible if the tooth is in a satisfactory position in terms of its angulation and depth.
Cystotomy is also used in large dentigerous cysts when enucleation and curettage might otherwise result in neurosensory dysfunction or predispose the patient to an increased chance of pathologic fracture. The prognosis for most dentigerous cysts is excellent, with recurrence rate being very low.
Gingival cyst of the newborn
Gingival cysts of newborns originate from remnants of the dental lamina and are located in the corium below the surface epithelium. These structures generally occur as small multiple or solitary nodules. They are located on the alveolar ridges of newborns or young infants. Occasionally, they may become large enough to be clinically noticeable as discrete white swellings on the alveolar ridges. They are generally asymptomatic and do not produce any discomfort for the infant.
Histologically, the gingival cyst of the newborn is a true cyst with a thin epithelial lining. The cyst cavity is usually filled with keratin but may contain some inflammatory cells, dystrophic calcifications, and hyaline bodies.
Epstein pearls are similar lesion with which gingival cysts sometimes may be confused; however, the location and etiology of these lesions are somewhat different. Epstein pearls are cystic keratin-filled nodules found along the midpalatine raphe and are thought to be derived from entrapped epithelial remnants along the line of fusion.
No treatment is required for these lesions, which usually disappear either by opening onto the surface mucosa or through disruption by erupting teeth.
Odontogenic keratocyst
The odontogenic keratocyst is a distinctive form of developmental odontogenic cyst that deserves special consideration because of its specific histopathologic features and aggressive clinical behavior. Keratocysts derive from remnants of the dental lamina. They can be found anywhere in the jaws but the most common site is the angle of the mandible (Fig. 13.48).

Fig. 13.48. The odontogenic keratocyst of the angle of the mandible
Unlike other cysts of the jaws, their epithelium is a keratinising stratified squamous epithelium and their contents are therefore filled with desquamated squames and keratin, which form a foul-smelling semisolid cheese-like material. Odontogenic keratocysts grow in a neoplastic fashion and not in response to internal pressure. The thin and friable wall of the cyst usually can pose problems for removal in one piece intraoperatively.
The lesions grow in a multilocular bosselated fashion with daughter cysts which protrude into the surrounding bone. Because of this relationship, the recurrence rate reported in patients with odontogenic keratocysts is high, particularly if the original surgical treatment does not result in complete removal of the lesion.
Odontogenic keratocysts may be found in patients ranging in age from infancy to old age; however, most of cases are seen in people of the second and third decades of life. A slight male predilection is usually seen, and 60 to 80 % of cases involve the mandible, particularly in the posterior body and ascending ramus. In younger patients these cysts are commonly found as part of the basal cell nevus syndrome, also known as Gorlin – Goltz syndrome (Fig. 13.49). In this case multiple keratocysts are found in different parts of the jaws (Fig. 13.50).

Fig. 13.49. Gorlin – Goltz
syndrome

Fig. 13.50. Panoramic x-ray, multiple jaw cysts
Clinical features
Odontogenic keratocysts are different from other jaw cysts; they are aggressive and can be difficult to remove. They can grow quite rapidly, and recurrences are frequent.
The active growth of keratocysts appears not to be evenly distributed, so the cyst does not expand uniformly as a sphere or oval-shaped lesion. Different rates of activity within areas of the lining probably account for the formation of locules, which, once the cyst has achieved a moderate size, will give rise radiographically to the typical multilocular appearance. On the late stages the cyst may reach a considerable size, causing the expansion and later on a destruction of the outer cortical plates. Lingual expansion is noted as well as buccal once.
Unless infected, these sometimes very large lesions are painless and do not exert sufficient pressure on vital structures such as the inferior dental nerve to cause paraesthesia of the lip and chin. When infected, however, they can become very painful, cause anaesthesia and may discharge into the mouth, with consequent bad taste and bad breath as additional clinical features.
Infection occurs mostly when the cyst is quite large and where soft tissue trauma results in bacterial contamination. It is not infrequent to find that with expansion the cyst communicates with the surface through the periodontal space of an adjacent tooth.
As with other cysts, the diagnosis of odontogenic keratocysus is based on clinical features, radiographic findings (Fig. 13.51) and the results of aspiration and biopsy. Two extraoral radiographic views at right angles to each other, such as an orthopantomogram and posteroanterior mandibular view, may be required with large keratocysts.

Fig. 13.51. CT scanning. Keratocyst of the maxilla growing to the left infratemporal fossa
Classically, the appearance is of a multilocular radiolucency with marked expansion of both buccal and lingual plates. Unerupted wisdom teeth may well be pushed into ectopic positions such as inverted high into the ramus of the mandible. The inferior dental canal may be difficult to see and may reflect the more active growth of these cysts around the canal with less evidence of significant repositioning as is seen with radicular cysts. Displacement or tilting of the teeth can be a feature, as well as the resorption of dental roots. In large or recurrent cysts the usage of computer tomography is recommended for accurate estimation of the cyst size and to define its extension outside the bone.
Aspiration will yield a “dirty” cream-colored semisolid material composed of keratinized squames. These can be confirmed histologically and provide good evidence that the lesion is a keratocyst.
Odontogenic keratocyst has variety of clinical and radiological manifestations and can mimic other jaw cysts and tumors. It belongs in the differential diagnoses of any radiolucency of the jaws. Because of this diagnosis of the lesion should be proved histologically in all cases.
Treatment
Adequate diagnosis and treatment of the odontogenic keratocyst is important because this cyst is recognized as being more aggressive than other odontogenic cysts, the odontogenic keratocyst has a higher rate of recurrence than other odontogenic cysts, and the association with nevoid basal cell carcinoma syndrome requires that the clinician examine a patient with multiple cysts of the jaws for physical findings that might diagnose this syndrome.
Like the treatment of most odontogenic cysts, the odontogenic keratocyst may be treated with enucleation and curettage and must be removed in one piece, which requires acceptable access and lighting. As such, many patients are suitably treated in an operating room setting under general anesthesia. This is particularly helpful when removing large cysts.
Keratocysts have a higher recurrence rate than other cysts and especially when they are large and multilocular. Enucleation is suitable for most keratocysts but may be difficult in large ones where, for example, they extend upwards into the vertical ramus of the mandible. Surgical access may be difficult and with the multilocular pattern of growth it may be impossible to ensure that the whole lining is removed. It is known that small clusters of epithelium known as microcysts, or satellite cysts can lie outside the epithelial lining may account for eventual recurrence. For this reason, in large or recurrent cysts enucleation with peripheral ostectomy and/or cryosurgery are recommended as a treatment of choice.
Cystotomy can be used particularly with large keratocysts where it can be sometimes effective. It may be appropriate in some cases to use the technique to reduce the size of the lesion before enucleating it. Whatever method is used, long-term (for years) follow-up radiography is imperative to ensure that there is no recurrence. The reported frequency of recurrence of the odontogenic keratocyst is approximately 30 %.
Gorlin – Goltz syndrome known also as the nevoid basal cell carcinoma syndrome, basal cell nevus syndrome, Gorlin’s syndrome is an autosomaldominant inherited condition that exhibits high penetrance and variable expressivity. It is caused by mutations in the PTCH tumor suppressor gene, mapped to chromosome 9q22.3 – q31. Affected patients may demonstrate the presence of multiple keratocists and skin lesions in the form of basal-cell naevi or carcinomas, and skeletal abnormalities affecting the vertebral column and the ribs.
Clinical signs of the syndrome include mild ocular hypertelorism, midface hypoplasia, relative frontal bossing and mandibular prognathism, mental retardation, schizophrenia, multiple basal cell carcinomas, calcification of the falx cerebri, rib anomalies (splayed, fused, partially missing,bifid), palmar pitting (the pits later develop into basal cell carcinoma), and multiple odontogenic keratocysts.
Other symptoms seen less commonly are epidermal cysts of the skin, spina bifida occulta of cervical or thoracic vertebrae, calcified ovarian fibromas, and short fourth metacarpals, kyphoscoliosis or other vertebral anomalies, medulloblastoma, meningioma, lymphomesenteric cysts, cardiac fibroma, fetal rhabdomyoma, cleft lip and palate, hypogonadism in males.
The most significant clinical feature is the tendency to develop multiple basal cell carcinomas that may affect both exposed and non-sun-exposed areas of the skin. Pitting defects on the palms and soles can be found in nearly two-thirds of affected patients. The discovery of multiple odontogenic keratocysts is usually the first manifestation of the syndrome that leads to the diagnosis. For this reason, any patient with an odontogenic keratocyst should be evaluated for this condition. Of patients with odontogenic keratocysts, 5 % have basal cell nevus syndrome. Early identification of these patients and their lesions is the key to improving long-term survival and quality of life.
Although the cysts in patients with the nevoid basal cell carcinoma syndrome cannot definitely be distinguished microscopically from those not associated with the syndrome, they often demonstrate more epithelial proliferation and daughter cyst formation in the cyst wall.
The treatment of the odontogenic keratocyst in patients with the nevoid basal cell carcinoma syndrome can be difficult owing to the large number of “recurrences” in these patients.
Radicular cysts
Radicular (periapical) cysts are pathological cavities, lined with epithelium, and contain fluid or semi-fluid material. They are the most common cystic lesions of the jaws and originate from the epithelial remnants of Malassez rests, which are stimulated after inflammation at the apices of nonvital teeth.
The usual etiology is a tooth that becomes infected, leading to necrosis of the pulp. Toxins exit the apex of the tooth, leading to periapical inflammation. This inflammation stimulates the Malassez epithelial rests, which are found in the periodontal ligament, resulting in their proliferation and formation of a periapical granuloma. Eventually, this epithelium undergoes necrosis caused by a lack of blood supply, and the granuloma becomes a cyst. The formation of an epithelial semipermeable lining to the cyst content, that allows fluids to enter the lumen by osmosis, leads to its gradual enlargement in response to hydrostatic pressure.
Hystologically, the epithelium of the cyst lining is a nondescript stratified squamous epithelium without keratin formation. Inflammatory changes may be observed in the cyst wall, and these changes, in turn, may lead to epithelial changes (eg, ulceration, atrophy, hyperplasia).
Clinical presentation. The majority of radicular cysts are asymptomatic, especially on early stages. The small lesions are not usually clinically detectable and most often are discovered as incidental findings on radiographic examination.
With continued growth, the cyst eventually approaches the surface of the alveolar bone and manifests as a buccal, lingual or palatal swelling. As the apices of most teeth lie closer to the buccal than the palatal or lingual plates, it is the buccal plate which is affected most commonly. Palatal expansion of the cyst is usually associated with an upper lateral incisor, reflecting the palatal inclination of its apex. This bony swelling (known as bony expansion) is the first real evidence of a cyst. On late stages the expansion of the cortical plate becomes thinned and may demonstrate a crackling sound (crepitus). If the bone is completely destroyed, the cyst is connected to the periosteum and the mucosa in this area looks bluish-red. The cyst in this case became a soft fluctuant (fluid-filled) on palpation.
Loosening or tilting of adjacent teeth is only encountered in very large cysts, and resorption of roots usually results from repeated infection of the cyst and is very uncommon. Unless a radicular cyst becomes infected, it will remain painless and vital structures will be gently moved aside to accommodate it. This can be seen clearly in larger mandibular cysts, which push the inferior dental canal downwards to the lower border of the mandible. No paraesthesia of the lip or chin will be noted unless the pressure within the cavity rises rapidly as with an acute infection.
In radicular cyst the decayed non-vital tooth responsible for the lesion is usually present. With large cysts occasionally this tooth elicits a rather hollow note on percussion. From time-to-time the teeth responsible for the formation of a radicular cyst may be extracted but the cyst remains and may well increase in size subsequent to the extraction. In this circumstance the name residual cyst is commonly used.
Acute infection can supervene at any time during this process of cyst evolution and in this cases pain as well as other symptoms which resemble an acute periodontitis or periostitis. The acutely infected cyst may bursts and discharges into the mouth with fistula formation.
Diagnosis of radicular cysts is based on clinical and radiographic examination, as well as aspiration of the contents of the cystic sac. It should be also confirmed hystologically after the surgical treatment of the lesion.
Radiographically, radicular cysts present as a round or oval-shaped osteolytic or radiolucent lesions surrounded by a well-defined radiopaque borders (looking as a thin white line of increased bone density) (Fig. 13.52). This radio-opaque surrounding is due to reactive bone sclerosis around the lesion in an attempt to wall it off. It is also associated with slow rate of growth typical to most radicular cysts. The affected tooth will show loss of its apical lamina dura. Very occasionally there may be the evidence of resorption of adjacent teeth and this reflects repeated acute episodes of infection within the cyst.

Fig. 13.52. Radicular cysts of the maxilla and mandible
Similarly, such infection can cause haziness in the sharp radio-opaque delineations of the margin of the cyst. In larger mandibular cysts there may be clear evidence of the inferior dental canal having been displaced downwards by the advancing lesion.
In maxillary cysts, penetrating into the sinus cavity, the signs of reactive sinusitis are often observed, as well as the semi-round shadow of the cyst, projecting to the sinus cavity (Fig. 13.53).
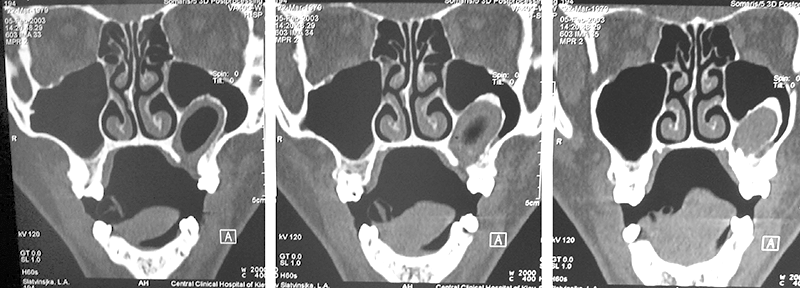
Fig. 13.53. CT scaning of the radicular cyst, penetrating into the sinus cavity
In addition to the clinical and radiographic examination, aspiration of the contents of the cystic sac may be a valuable diagnostic aid. This procedure is possible in the large cysts with little or no bony covering. Usually the fluid appears as straw-coloured in which a shimmer may be seen due to its cholesterol content. However, if the cyst has been infected, this characteristic appearance may be lost and the fluid may consist of pus or blood-stained pus.
Several treatment options exist for radicular cysts. Depending on the clinical situation cysectomy, cystotomy, plastic cystotomy can be used. Most lesions should be surgically removed (cystectomy) and histopathologically examined. The tooth, responsible for the lesion, should be treated endodontically or removed.
Diagnostic tests used in patients with the jaw cysts
Radiographs – intra and extra-oral views:
- Round or oval radiolucence with well demarcated sclerotic border typical for most of the cysts.
- Associated with non-vital decayed tooth (radicular cyst).
- Associated with the crown of unerrupted tooth (dentigerous cyst).
- Not associated with the roots of the teeth (fissural cysts).
- Multilocolar or unilocular lesion (odontogenic keratocysts).
Vitality testing of teeth (electroodontometry).
Aspiration of fluid contents:
- Straw-coloured fluid containing cholesterol crystal from most cysts.
- Air, some blood or serosanguious fluid from solitary bone cysts.
- Blood from aneurismal bone cyst.
- Pus from infected cyst.
- Pale, yellow fluid containing keratin from odontogenic keratocyst.
Biopsy of lining, provides definitive diagnosis.
Management of the jaw cysts
There are several approaches that can be used for surgical treatment of the jaw cysts.
The main procedures used for these lesions listed below.
- Enucleation with primary closure (cystectomia) is the most common and generally the treatment of choice. It consists of removing the cyst lining from the bony walls of the cavity and repositioning the access flap. Any relevant dental pathology is treated at the same time.
- Enucleation with packing and delayed closure is used when badly infected cysts, particularly very large ones, are unsuitable for primary closure.
- Enucleation with primary bone grafting.
- Cystotomy (marsupialization) – opening of the cyst to allow continuity with the oral mucosa. Healing is slower than with enucleation and a cavity persists for some time.
- Plastic cystotomy – enucleation of the cyst followed by icertion of the mucoperiosteal flap into the bone cavity.
- Operations for cysts penetrating into the maxillary sinus – usually include the formation of the anastomosis between the cyst cavity and the sinus and, sometimes, with the nasal cavity.
Among these numerous operation types two techniques are employed in clinical practice for the surgical removal of cysts most commonly: cystectomy (removal of the lining in total) and cystotomy (creation of a permanent opening into the cyst cavity). The vast majority of cysts are treated by cystectomy, with cystotomy (marsupialisation) tending to be reserved for certain categories of patients, usually with larger cysts.
Cystectomy (Parch II operation)
Cystectomy involves complete removal of the cystic sac and healing of the wound by primary intention. This technique is suitable for all small to moderate-sized cysts and the majority of large cysts. This is the most satisfactory method of a cyst treatment and is indicated in all cases where cysts are involved, whose wall may be removed without damaging adjacent teeth and other anatomic structures.
After taking a radiograph to determine the exact localization and size of the lesion, a trapezoidal flap is created, whose extent must ensure adequate access and visualization of the surgical field.
Root-treating and conserving the tooth causing the cyst may be worthwhile and surgery may therefore be preceded by endodontic treatment.
The surgical procedure for treatment of a cyst with enucleation includes the following steps:
- Reflection of a mucoperiosteal flap.
- Removal of bone and exposure of part of the cyst.
- Enucleation of the cystic sac.
- Care of the wound and suturing.
After reflection of the mucoperiosteum, the bone covering the lesion is evaluated. It may be normal, thinned, or completely destroyed. In normal bone, a round bur is used to remove a portion of the buccal cortical plate covering the cyst, and, depending on its extent, the created osseous window is than enlarged if necessary. The osseous window must be large enough so that all parts of the cystic cavity may be accessed and removed without particular difficulty.
If the bony wall is thinned or perforated, it is removed peripherally until it reaches compact bone. A curette is used for enucleation of small cysts, while for larger cysts, the broad end of a periosteal elevator is preferred, which is placed inside the cavity pressing gently between the cystic wall and bone, while the cyst is carefully grasped with forceps. The lining should be sent for histopathological investigation.
After removal of the cysts, a curette is used to inspect the cavity for the presence of remnants of the cyst. After irrigating with sterile saline the flap is sutured back to its anatomical position. If the tooth has been root filled, an apicectomy should be performed at the same time with retrograde sealing of the canal if appropriate.
The operation for all but very large cysts is usually carried out under local anaesthesia with or without sedation according to the patient’s preference. Postoperative complications are rare, although breakdown of the wound in large mandibular cysts can occur. The patient is normally recalled about 4–6 months postoperatively, when a radiograph should show evidence of bony infilling of the cyst cavity.
Cystotomy. This method is usually employed for the removal of large cysts and entails opening a surgical window at an appropriate site above the lesion.
The rationale of this treatment is the permanent destruction of the integrity (wholeness) of the cyst. This, in effect, depressurises the cyst cavity, stops its continued expansion and encourages a shrinkage of the lining by new bone formation around its periphery.
It is more suitable for large cysts where enucleation may endanger vital structures such as the inferior dental nerve or there is a risk of fracture during enucleation. The limited surgery involved is very suitable for outpatient care under local anaesthesia and it can therefore be particularly appropriate for elderly or medically compromised patients who would be at risk from a general anaesthetic.
In order to create the surgical window, initially a circular incision is made, which includes the mucoperiosteum, the underlying perforated bone, and the respective wall of the cystic sac. After this procedure, the content of the cyst is evacuated, and interrupted sutures are placed around the periphery of the cyst, suturing the mucoperiosteum and the cystic wall together.
Afterwards, the cystic cavity is irrigated with saline solution and packed with iodoform gauze, which is removed a week later together with the sutures. During that period, the wound margins will have healed, establishing permanent communication. Irrigation of the cystic cavity is performed several times daily, keeping it clean of food debris and averting a potential infection.
Healing of the wound is by secondary intention, and the epithelium of the cyst is thus transformed into oral mucosa.
Any decision to marsupialise a cyst cavity should be preceded by histological evidence that confirms the lesion as a cyst and this involves a small incisional biopsy or retrieving tissue from the cyst cavity at the time of the procedure.
With the lining no longer complete, the bone heals inwards around the cyst, reducing it progressively in size. In some cases cyst can be removed by enucleation when it has reduced to a more manageable size.
In some cases the plastic cystotomy is used after performing the cyst enucleation. The mucoperiosteal flap is then turned into the remaining cavity and fixed with iodoform gauze. This procedure is used in cases of severe injury of the muco-periosteal flap during the operation, its defect, infection development or breakdown of the wound after cystectomy of the large cysts.
Marsupialisation of a large cyst may take many months for healing to occur and the onus is therefore on the patient to maintain cleanliness by frequent irrigations of the cyst cavity, as described above.
In infected cysts two-stage treatment is used. On the first stage the cyst is drained via the vertical incision or using the special needles. Antibiotics are prescribed and endodontic treatment of the non-vital teeth associated with the cyst is performed. When the signs of acute inflammation resolve, the final surgical procedure (usually cystectomy) is performed.
Benign odontogenic tumors and tumor-like lesions of the jaws
Tumours or tumour-like wellings of the jaws can be odontogenic or nonodontogenic. Odontogenic tumors comprise a complex group of lesions of the jaws, derived from primordial tooth-forming tissues and presenting in a large number of histologic patterns. They are lesions of great importance to oral and maxillofacial surgeons. Many of them are true tumors derived from tooth-forming tissue, whereas some are developmental malformations or hamartomas. Odontogenic tumors may arise from epithelial or mesenchymal tissue. Like normal odontogenesis, odontogenic tumors demonstrate varying inductive interactions between odontogenic epithelium and odontogenic mesenchyme.
Odontogenic lesions arise from tissue with the potential for differentiation into tooth or periodontal ligament structures, and they are found predominantly at tooth-bearing sites. Variable but distinctive histological features of odontogenic lesions include formation of tooth-related extracellular substance, some of which may calcify and be visible on radiographs, and epithelial-mesenchymal interactions.
In general terms, odontogenic tumors tend to be more common in younger patients but can occur at any age. They originate in the jaws and usually are found in the tooth-bearing sites. They are often associated with impacted or missing teeth. The common sites for odontogenic tumors are the mandibular molar region and the maxillary cuspid region. Odontogenic tumors are usually slow-growing and asymptomatic. Pain is not a feature of benign tumors of the jaws but is a common symptom of malignant tumors of the jaws. The odontogenic tumors are expansile lesions and may expand the bony cortex, but usually do not invade or perforate it.
Most odontogenic tumors are essentially benign lesions but are rather aggressive and can infiltrate the adjacent bone. This form of bony infiltration is not the true invasiveness of malignant tumors but represents a clinical problem that the tumor can recur after surgical therapy if the bony margins still contain some of the tumor remnants. A block resection leaving the cortical lower border of the mandible intact is favored. These benign tumors are relatively unaffected by radiation, and the risk of radiation stimulating the development of a malignant tumor or of radiation necrosis is unwarranted for a benign tumor.
True malignant transformation of benign odontogenic lesions or the development of malignancy de novo from odontogenic tissues have both been reported, but such occurrences are extremely rare. In general, the less-differentiated odontogenic lesions (the immature ones) are more likely to have indistinct radiographic borders, invasive growth patterns, and relatively aggressive clinical behavior, while the mature or well-differentiated entities are more likely to produce recognizable extracellular product, to be well circumscribed, and to be self-limiting in terms of growth.
Odontogenic tumours have been classified by the WHO as shown in Table 13.2.
Table 13.2. WHO classification of the odontogenic tumours
| Benign neoplasms |
Malignant neoplasms |
Ameloblastoma
Adenomatoid odontogenic tumour
Calcifying odontogenic tumour
Calcifying epithelial odontogenic tumour
Calcifying odontogenic cyst
Ameloblastic fibroma
Ameloblastic fibro-odontoma
Odontogenic fibroma
Odontogenic myxoma
Melanotic Neuroectodermal Tumor of
Infancy
Cementoma
Odontomas (compound and complex) |
Odontogenmc carcinomas
Primary intraosseous carcinoma
Ameloblastic carcinoma
Malignant ameloblastoma
Clear cell odontogenic carcinoma
Squamous odontogenic tumor
Odontogencc sarcomas
Ameloblastic fibrosarcoma
Ameloblastic odontontosarcoma |
Ameloblastoma
Ameloblastoma is an epithelial tumor arising from the dental lamina, Hertwig sheath, the enamel organ, or the lining of dental follicles. Ameloblastomas are the most common odontogenic tumors of the jaws. This lesion occurs in both the maxilla and mandible, but the posterior mandible is the most common location. 70 % of all ameloblastomas develop in the posterior lower molar region, and often involve the ramus of the mandible. The lesion is distributed equally between males and females.
Ameloblastomas are usually first recognized between the ages of 20 and 40 years. They are rare in children in their first decade of life and relatively uncommon in the second decade and in old people (Fig. 13.54; 13.55).

Fig. 13.54. Ameloblastoma of the mandible, Left part

Fig. 13.55. Ameloblastoma of the mandible, Right part
Although ameloblastoma is not a malignant lesion, it is very aggressive and infiltrative. It does not metastasize but is stadely growing, persistent, and hard to eradicate.
Ameloblastomas are symptomless until the swelling becomes obtrusive. Therefore ameloblastoma is usually noticed as an incidental finding on radiographs taken for other purposes or its first symptom is painless bony expansion. Neurosensory changes are uncommon, even with large tumors.
Slow growth is the typical for ameloblastoma, but this tumor may reach a large size, leading to tremendous facial disfigurement.
Radiographically ameloblastomas usually appear as a rounded, cyst-like multilocular radiolucency with well-defined margins in the area of the lower third molar (however they may be found anywhere in the jaws). These lesions may be unilocular when small. Buccal and lingual cortical expansion is common, frequently to the point of perforation. Resorption of adjacent tooth roots is common (Fig. 13.56).

Fig. 13.56. Polycystic ameloblastoma of the corpus, angle of the mandible
Unicystic ameloblastomas (Fig. 13.57), most commonly seen in young patients, with about 50 % of these tumors being diagnosed during the second decade of life manifest as a unilocular radiolucency, mimicking a dentigerous cyst.

Fig. 13.57. Unicystic ameloblastoma
corpus of the mandible
Pathogenetically, this type of ameloblastoma is considered to be less agressive.
Differentiation of ameloblastoma from non-neoplastic cysts and other tumours or tumour-like lesions of the jaws is not possible by radiography and clinical signs alone.
Histologic patterns of ameloblastoma are multiple and include follicular, acanthomatous,plexiform, granular cell, basdal cell and other variants. In all cases the neoplastic component is purely epithelial with a reactive connective tissue component. In folicular ameloblastomas, which is the most common and easely recognisable type, the stellate reticulum is located within the center of the islands and trabecule of odontogenic epithelial cells. Epithelial structures consist of a well-organised single layer of tall, columnar, ameloblast-like cells. Plexiform type of ameloblastomas consists mainly of thin trabeculae of small epithelial cells in a connective tissue stroma. The stellate reticulum is located outside of the odontogenic rest.
Acanthomatous ameloblastomas show squamous metaplasia of the odontogenic epithelium. Granular cell ameloblastomas are rare and consists the epithelium, which forms sheets of large cells with granular eosinophilic cytoplasm in the central areas of the tumour islands. Basal cell variant is the least common. It consists of basaloid cells predominantly in a trabecular patternt, with a strong resemblance to basal cell carcinoma. In this latter tumor stellate reticulum is not present in the central portions of the nests. The variety of the hystological patterns make it difficult to diagnose the ameloblastoma even for experienced hystologist.
Treatment. The diagnosis of ameloblastoma must be confirmed by biopsy in all cases. The treatment of ameloblastoma is surgical excision with wide free margins. In the mandible, 1 cm clear margins are considered the standard. This may be accomplished with block or segmental resection, depending on the relationship of the lesion to the inferior cortical border.
The maxillary ameloblastoma is not confined by the strong cortical plate found in the mandible. In addition, the posterior maxilla lies in close relationship to many vital structures. These factors make strong arguments for aggressive and definitive surgical treatment of the maxillary ameloblastoma.
Complete excision is curative but enucleation is usually followed by recurrence. Ameloblastoma tends to infiltrate between intact cancellous bone trabeculae at the periphery of the tumor before bone resorption becomes radiographically evident. Therefore, the actual margin of the tumor often extends beyond its apparent radiographic or clinical margin. Attempts to remove the tumor by curettage, therefore, predictably leave behind small islands of tumor within the bone, which are later determined to be recurrent disease.
Complete excision of a large ameloblastoma usually means total resection of the jaw. Appropriate reconstruction by the bone graft may be performed at the same time.
The single exception to this may be the unicystic ameloblastoma. Unlike other types of ameloblastomas, it is believed that this lesion can be removed with enucleation/curettage procedures alone. These lesions however may recur, and in this cases more aggressive treatment is required.
All patients with ameloblastoma, regardless of surgical treatment method or histologic type, must be monitored radiographically for several years. If necessary re-operation is performed. The patient must be warned of the necessity of regular follow-up and, possibly, of a further operation.
Odontomas
Odontomas are developmental malformations (hamartomas) of odontogenic epithelium and mesenchyme and not true neoplasms. Even when the morphology is grossly distorted (as in complex odontomas), structures which resemble the pulp, dentine, enamel and cementum can be found in normal hystologic relationships with one another. When odontoma became fully calcified on its late stages they stop growing and do not develop further. In some cases the “eruption” of odontomas is observed, like in normal teeth.
Odontomas are the most frequently occurring odontogenic tumors and usually found between ages 10 and 20 years. They affect the maxilla slightly more frequently than the mandible and are often recognised in early adolescence by the dense opacity of the enamel component in routine radiographs. When odontomas have erupted, infection develops and abscess formation is commonly observed. In some cases, odontomss displace teeth or block their eruption.
The main types of odontomas are simple odontomas, compound odontomas and complex odontomas. Simple odontomas are the malformations arising from one tooth germ. In this type of odontoma pulp, dentine, enamel and cementum have normal anatomical relationships with one another, and the form of this lesion is near to normal (Fig. 13.58).

Fig. 13.58. Simple odontomas
Morfological distorsion may affect only the crown or the crown and root together. They can pose both aesthetic and orthodontic problems. In cases where extraction is necessary; simple odontoma may cause difficulties due to its complex In some classifications this type of odontomas is not considered as tumors or tumor-like lesion. Other types of odontomas are compound, in which multiple small toothlike structures exist; and complex, in which irregular masses of dentin and enamel are present with no anatomic resemblance to a tooth.
Compound odontomas are predominantly seen in the anterior maxilla, whereas complex odontomas are typically seen in the posterior maxilla or mandible.
Compound odontomas
Compound odontoma consists of many (2 to 30) small, tooth-like structures massed together within an outer capsule. This structures (denticles) are probably produced by localized, multiple budding-off from the dental lamina and formation of many tooth germs (Fig. 13.59). It represents the product of both histodifferentiation and morphodifferentiation of odontogenic tissues, resulting in what appears as a cluster of multiple abortive teeth.

Fig. 13.59. Compound odontoma
It most commonly forms in the anterior part of the maxilla but may be located anywhere within the tooth-bearing segments of the jaws. In some cases it gives rise to a painless swelling and it is often responsible for preventing normal tooth eruption, thus it usually is discovered during adolescence. The odontoma may be small, with only a few tiny teeth, or it may be of considerable size and contain many denticles.
Histologically, compound odontomas approaches to normal tooth structure. The denticles are embedded in fibrous connective tissue, and have a fibrous capsule. In majority of cases the macroscopical examination is sufficient for diagnosis.
Radiographically compound odontoma consists of multiple tiny toothlike densely-calcified structures contained within a fine radiolucent rim.
Complex odontoma
Complex odontomas consist of an irregular mass of hard and soft dental tissues, having no morphological resemblance to a tooth and frequently forming a cauliflower-like mass. This developmental aberration results in a random laying-down of all the dental elements in a totally haphazard fashion.
Clinically, complex odontomas are usually detected in adolescence, but may escape diagnosis until late in life. They usually have a predilection for the mandibular molar regions; however, they can be found in other areas of the jaws. Typically, a hard painless swelling is present, but the mass may start to erupt and in these cases infection may develop.
Radiographically, when calcification is complete, an irregular radiopaque mass is seen containing areas of different radiopaq density. Enamel, dentine, cement and pulpal tissues are all represented and the radiographic image may reflect these different tissues with varying degrees of opacity and radiolucency. The radioopaque zone is surrounded by a thin, uniform, radiolucent rim. Distinct line of cortication usually separates lesion from normal bone (Fig. 13.60; 13.61).

Fig. 13.60. Complex
odontomas

Fig. 13.61. Complex odontomas, macropreparation
Although this radiographic picture may have some resemblance to the radiographic picture of osteosarcoma, the association with a tooth, the clear demarcation of the lesions’ borders, and the lack of pain and/or swelling serve to delineate this very benign lesion from osteosarcoma.
Histologically, the mass consists of all the dental tissues in a disordered arrangement. Histodifferentiation but no morphodifferentiation is typical to this lesion. The epithelium in this lesion has involuted, leaving disorganized dental hard tissues in place. A mixed honeycomb presentation of enamel, cementum, dentin, and pulpal tissue is present. The pulp is usually finely branched so that the mass is perforated, like a sponge, by small branches of pulp.
Differential diagnoses of odontomas include focal sclerosing osteitis, osteoma, periapical cemental dysplasia, ossifying fibroma, cementoma.
The method of treatment used in all types of odontomas is surgical removal and curettage of the fibrous capsule. Being enucleated from bone these lesions do not recur.
Adenomatoid odontogenic tumour
The adenomatoid odontogenic tumor is a fairly uncommon benign tumor, but it usually can be easily identified from its clinical and radiographic appearance. These lesions are usually diagnosed in the second and third decades of life and make up from 3 to 7 % of all odontogenic tumors. This lesion was preveously believed to be a variant of ameloblastoma and was designated adenoameloblastoma. Now it is considered as a hamartomous lesion originating from the reduced enamel epithelium of the dental follicle. Its clinical features and biologic behavior permit distinction from the ameloblastoma.
Adenoamatoid odontogenic tumor has a predilection for the anterior region of the jaws. Most of the cases occur in the anterior maxilla, the second most common place of its occurance is the anterior mandible. Two thirds of the cases are associated with unerupted tooth (usually the canine). Females are affected about twice as often as males. Clinically, adenomatoid odontogenic tumours are usually found either in late adolescence or young adults.
Tumor has a limited growth potential and therefore it is considered as a hamartoma rather than a true neoplasm. Histologically it has a thick fibrous capsule filled with a proliferation of epithelial elements that form nodules and microcysts, resembling ducts cut in cross-section and lined by columnar cells similar to ameloblasts. Tubular or duct-like structures are characteristic for the adenomatoid odontogenic tumor. The product of the tumor cells, a pre-enamel matrix, is thought to degenerate and ultimately leave areas of dystrophic calcification and amyloid. When the lesion is bisected, the central portion of the tumor may be essentially solid or may show varying degrees of cystic change with intraluminal proliferation of tissue.
Clinical signs.
Adenoamatoid odontogenic tumor is generally asymptomatic but may present with mild swelling or in association with a clinically missing tooth. The tumour is most frequently sited in the anterior maxilla and forms a very slow-growing swelling. It also may be noticed by chance on a radiograph where it frequently simulates a radicular or dentigerous cyst. Most specimens are small, rarely exceeding 3 cm in diameter.
Radiographically this lesion generally appears as a well-demarcated radiolucency, which may contain radiopaque flecks, representsng calcified material. In 75 % of cases, it is associated with an unerupted canine and can be indistinguishable from a dentigerous cyst.
Treatment and Prognosis.
The treatment of choice for adenomatoid odontogenic tumor is simple removal. Owing to this lesion being encapsulated, it separates easily from the surrounding bone. If the tumor is completely removed at biopsy, the reccurences are very uncommon.
Melanotic neuroectodermal tumor of infancy
Melanotic neuroectodermal tumor of infancy (MNTI) is a relatively uncommon osteolytic pigmented neoplasm that primarily affects the jaws of newborn infants. In most patients (more than 90 %), tumor manifests in the first year of life, usually from age 1–6 months. Although MNTI is classified as a benign lesion, it is often clinically worrisome because of its rapid onset and alarming local growth rate. Often, sucking and feeding are impaired secondary to the swelling. The typical MNTI begins as a nonulcerated, lightly pigmented, blue or black lesion on the anterior aspect of the maxilla and rapidly expands to form a swelling or a tumescence that is cosmetically obvious to the parents of the infant. The intraoral lesion appears as a sessile, lobulated mass, often reaching 2–4 cm in diameter by the time of diagnosis. Bone destruction often occurs because of the intraosseous expansion of the tumor, which can displace or destroy the developing deciduous and permanent dentition. Although the lesion expands rapidly, the overlying mucosa remains intact.
Plain dental radiography, CT scanning, and MRI are used in diagnosis of MNTI. The radiographic appearance of the tumor is a well-circumscribed irregular radiolucency, although diffuse, ill-defined cases have also been reported. The bone is destroyed as the tumor advances. Although a few cases have been described as multiloculated, most MNTI are unilocular. CT scanning with intravenous contrast is often used to delineate the margins of osseous involvement. Additionally, MRI with gadolinium contrast can be used to evaluate the extent of the lesion. Most MNTI appear as typical soft tissue tumors with nonenhancing heterogeneous tissue density.
The fast-growing pattern of the lesion, in many cases suggests a clinical impression of infection or malignant neoplasm. So, if a differential diagnosis is established from the clinical and radiographic findings, histologic evaluation of a surgical specimen is necessary to determine the final diagnosis. Although the histologic appearance is characteristic, special immunohistochemical stains and electron microscopy may be necessary to make a definitive diagnosis.
Grossly, the tumor has a gray, hard, rubbery consistency with foci of blue- black pigmentation. Additionally, entrapped developing tooth buds may be noted in the specimen as MNTI grows in and around the odontogenic apparatus.
The histologic appearance of MNTI is unique and characteristic in that a distinct biphasic pattern exists. The peripheral borders of the tumor are faintly noted as a thin, delicate, fibrous layer. In majority of cases tumor shows local infiltration into the adjacent bone.
One portion of the lesion contains large polygonal cells arranged in sheets or alveolarlike structures. These large cells have pale abundant cytoplasm and pale nuclei with finely dispersed chromatin. They often contain the melanin pigment that gives the MNTI its blue-black clinical appearance. The central portion of the alveolar spaces contains the second smaller characteristic cell type. These cells are lymphocytelike or neuroblastlike with small, dark nuclei and little, if any, cytoplasm.
Treatment and prognosis. MNTI is benign tumor, which can be effectively managed by aggressive surgical excision. This treatment can usually be accomplished with a partial maxillectomy by using a Weber – Ferguson incision and a facial degloving approach. Teeth, developing teeth, and the adjacent bone must be sacrificed when they lie near the borders of MNTI. It is recommended, that 5 mm margin of healthy tissue should be included in the surgical specimen.
The possibility of local recurrence in patients with MNTI remains a significant problem. The average recurrence rate is 15–20 %. The recurrent lesions, possibly secondary to inadequate excision or multicentricity, usually become apparent within the first year after surgery. In instances of inoperable recurrence or where clear margins are impossible to obtain, radiation therapy and/or chemotherapy can be used.
Although MNTI is an aggressive benign tumor, malignant variants have been also reported, ranging from 1.5 % to 2.1 % of total MNTI. Metastatic spread of MNTI occurs infrequently, in less than 5 % of malignant cases. Management of these rare cases is different with poor prognosis.
In all cases of MNTI postoperative care by monitoring the patient with physical and radiographic examination at monthly intervals for the first postoperative year is obligatory. Reconstruction of the affected jaw may be challenging. Permanent reconstruction of the maxillary alveolus and missing dentition in some cases is delayed until the growth is completed, often in the teenage years. In the interim, transitional removable partial dentures may be necessary. The skills of an orthodontist, prosthodontist, oral surgeon, and/or dentist may be required, based on the extent of the missing structures, to correct any functional and cosmetic deformity.
Calcifying (GHOST CELL) odontogenic cyst
The calcifying odontogenic cyst, or Gorlin cyst, is not actually a cyst but rather a true neoplasm with cystic tendencies.The are rare with no age, sex, or location predilections (it can be found anywhere in the jaws). It is a benign neoplasm but may undergo a malignant transformation.
If is not discovered as an incidental finding on radiographs, the earliest clinical presentation is a localized swelling. If not treated, the tumor may become quite large.
On radiographs, the appearance is usually nondescript radiolucency but it may be multilocular or contain flecks of calcification. Occasionally roots of adjacent teeth are eroded.
Hystologically the lining of cystic areas consists of squamous epithelium with cuboidal or ameloblast-like basal cells. Calcifying odontogenic cyst appears somewhat similar to the ameloblastoma, with masses of keratinized squamous epithelial cells. However, these cells have no nuclei and are called ghost cells. The ghost cells typically calcify in patchy fashion, and where this keratin-like material comes into contact with connective tissue it excites a foreign body reaction. More simply, this lesion represents enamel epithelium that has a tendency to mature but is unable to form enamel. Thise epithelium is more mature than in ameloblastoma, and, accordingly, the lesion have less growth potential.
Treatment and Prognosis
Calcifying odontogenic cysts are surgically removed by simple enucleation and rarely recur after excision.
Calcifying epithelial odontogenic tumour
The calcifying epithelial odontogenic tumor is a benign infiltrative tumor. It is derived from the stratum intermedium and has a lower growth potential than ameloblastoma. No cases of malignant transformation are reported. This rare neoplasm can occur at any site in the upper or lower jaw but is most commonly found in the mandibular molar/premolar region. It causes painless expansion of the affected area and in 50 % of cases it is associated with an unerupted or impacted tooth. Radiographs show a radiolucency, which may be multiloculated, and there may be areas of radiodensity within the central area of the radiolucency. Demarcation of the tumour from normal bone is not always clear.
Treatment
The treatment of this lesion is complete surgical excision. Because the lesion is locally invasive into the surrounding bone it is treated by a localised resection with a small margin of normal bone around it to reduce the chance of recurrence. The average recurrence rate for calcifying epithelial odontogenic tumor is 4 %. The lesion is slow growing and requires long-term follow-up monitoring for recurrence (at least 5–10 years).
Ameloblastic fibroma
Ameloblastic fibroma is a true mixed tumor arising from a combination of 2 embryonic tissues (epithelial and mesenchymal). This tumour is important in the differential diagnosis of ameloblastoma.
The ameloblastic fibroma tends to affect young persons in the first two decades of life. The posterior mandible is the most common site of the tumor. Ameloblastic fibroma is benign and grows expansively rather than invading surrounding tissues. It is slow-growing and usually asymptomatic, but eventually expands the jaw. The malignant change of the tumor is possible, though very rare. Approximately 45 % of ameloblastic fibrosarcomas develop in the setting of a recurrent ameloblastic fibroma. Radiographically, either a unilocular or multilocular lesion is observed most often in the posterior mandible. The radiographic appearance is identical to that of unicystic ameloblastoma, and both lesions should be differentially by diagnosed because they affect similar age groups and have similar clinical and radiographic appearances. Hystologicaly tumor is formed by both epithelium and connective tissue. The epithelial component of this lesion is almost identical to that of ameloblastoma. It consists of ameloblast-like or cuboidal cells surrounding others resembling stellate reticulum or more compact epithelium. The epithelium is sharply circumscribed by a basal membrane and forms islands in a loose but cellular, fibromyxoid connective tissue, which resembles the immature dentine papilla. It is a immature, cellular, homogenous connective tissue without much dense collagen. The epithelial and connective tissue components grow together inside a capsule.
Treatment and Prognosis
Ameloblastic fibromas do not infiltrate bone and separate readily from their bony walls. It is effectively treated by an enucleation and curettage surgery. But, if the tumor enucleation is incomplete, recurrence follows. Although recurrence is rare under the circumstances, resection should be reserved for recurrent lesions.
Odontogenic myxoma
The odontogenic myxoma is an uncommon benign infiltrative lesion of the jaws, which derive from dental ectomesenchyme.
These tumors are slow growing with a potential for aggressive behavior and a high recurrence rate after subtherapeutic removal. They occur over a wide age range, but most frequently in the second and third decades of life.
Clinically, young people are predominantly affected. Although the tumor can occur anywhere in the jaws, there is a slight predilection for the posterior mandible. If odontogenic myxoma is left untreated, it is invasive and destructive. The tumour gives rise to a fusiform swelling, erode bone and enlarge to form multilocular, radiolucent regions with scalloped margins or a soap-bubble appearance that can be very difficult to differentiate from other multilocular lesions such as ameloblastoma or odontogenic keratocysts. It may displace or cause root resorption of teeth in the area of the tumor. Although not pathognomonic of the odontogenic myxoma, the radiolucent defect may contain thin wispy trabeculae of residual bone, which are often arranged at right angles to one another in a “stepladder” pattern.
Histologically odontogenic myxoma resembles the dental papilla of the developing tooth. Histologically, the tumor is composed of haphazardly arranged stellate, spindle-shaped, and round cells in an abundant loose myxoid stroma that contains only a few collagen fibrils. The margins of the tumour are illdefined and peripheral bone is progressively resorbed. In some patients the tumor may have a greater tendency to form collagen fibers; such lesions are designated fibromyxomas.
Treatment and Prognosis
Odontogenic myxomas should be treated with resection with 1.0 cm bony linear margins as confirmed with a specimen radiograph. These tumors are not encapsulated and can infiltrate widely the surrounding bone such that complete removal by curettage is nearly impossible. Recurrences occur although with somewhat less frequency than with ameloblastoma.
Tumours and dysplasias of cementum
Cementoblastoma
Cementoblastoma is a true neoplasm of cementum neoplasm of cementum. Cementoblastoma is a benign neoplasm which forms a mass of cementum-like tissue as an irregular or rounded mass attached to the root of a tooth, usually a mandibular first molar. The lesion is usually asymptomatic, though occasionally the associated tooth may be slightly sensitive to percussion.
They are slow-growing and the jaw is not usually expanded. The tumor only rarely causes gross bony swelling and pain.
Radiographically, there is typically an opaque sunburst mass attached to the apex of a tooth with a thin radiolucent margin. The lession may be rounded or irregular in shape. Resorption of related roots is common, but the tooth remains vital (Fig. 13.62).

Fig. 13.62. Cementoblastoma from the 44 and 47 teeth
The tumor should be differenciated from sclerotizing (condensing) osteitis, a common lesion resulting from low-grade periapical irritation that stimulates bone growth. Although the most usual location for this lesions is the same, condensing osteitis does not obscure the periodontal ligament space and tends to be more irregular in outline.
Hystologically cementoblastoma consists of plump cementoblasts separated by cemental partitions. Cells are therefore enclosed within the cementum, and in the irregular spaces are many osteoclasts and osteoblast-like cells. The tumor is surrounded by a broad zone of unmineralised tissue and a connective tissue capsule.
Treatment. Removal of attached tooth and tumor is the method of treatment. Cementoblastomas are benign, and, if completely excised and the tooth extracted, there are no recurrences. Incomplete removal leads to continued growth.
Cemento-osseous displasias
Lesions formerly categorised as cementomas consists a group of the tumor like lesions which are now categorized as cemento-osseous displasias.
They are non-neoplastic proliferations originated from cementum and periodontal ligament origin. In this condition there is a disordered production of bone and cementum-like tissue in the jaws. They may occur singly or may affect many teeth in the dentition. Most of them are asymptomatic and are usually diagnosed by radiographic appearance. In the early stages they cause radiolucency, which later mineralises into cement-like tissue. The teeth affected are vital throughout this process.
There are three forms of cement-osseus displasias including periapical, focal, florid osseous dysplasias, and familial gigantiform cementoma, which are probably variants of the same pathologic process differentiated only by clinical and radiographic features. Histologically the three types of cemento-osseous dysplasia are indistinguishable, showing new woven bone trabeculae and/or zones of cementum-like material, which often blend into the cortical bone. A fibrous tissue stroma is also present with a very little inflammatory component. The etiology of these lesions remains unclean, but local trauma may play some role.
Periapical Cemento-osseous Dysplasia. Periapical cemento-osseous dysplasia presents as circumscribed lesions in periapical areas associated with vital teeth. Anterior mandible is the most common localization. Radiographically the lesions can be radiolucent, of mixed density, or radiopaque, depending on their stage of development.
Focal Cemento-osseous Dysplasia. Lesions of focal cemento-osseous dysplasia have a predilection for middle-aged females and present as nonexpansile radiolucencies with associated opacities, often in edentulous areas of the mandible. They frequently occur in sites of previous dental extractions and may represent some type of abnormal healing following dental extraction. Since they are usually asymptomatic, cases are often noted on routine panoramic radiographs. They are normally well circumscribed and rarely exceed 2 cm.
Florid cemento-osseous dysplasia presents as a painless nonexpansile lesion often involving two or more
Jaw quadrants. Radiographically, florid cemento-osseous dysplasia appears as multiple radiopaque, somewhat irregular lobular masses without a radiolucent border, located in tooth-bearing areas, wich can be mistaken for chronic osteomyelitis. Radiographically it appears as confluent radiopaque masses in. Lesions may be associated with superimposed infection and osteomyelitis, and have also been associated with idiopathic bone cysts. Histologically they have an unencapsulated proliferation of cellular fibrous tissue with trabeculae or woven bone and calcification. More mature lesions may become acellular and avascular with coalescent sclerotic bone masses. Many patients are partially or totally edentulous when the condition is first discovered. Therefore of dysplasia is usually asymptomatic unless they become infected, but can expand the jaw. Cortical expansion in this cases is usually of limited degree.
Familial Gigantiform Cementoma. Familial gigantiform cementoma represents a rare autosomal dominant variant of osseous dysplasia usually involving multiple quadrants with variably expansile lesions, often in the anterior mandible (Fig. 13.63).

Fig. 13.63. Familial gigantiform cementoma of the mandible (by H.O. Sedano)
This particular form of osseous dysplasia has no racial predilection. The lesions often evolve during childhood and can grow rapidly. Treatment is usually surgical and symptomatic and is limited to cosmetic recontouring.
Ossifying Fibroma
Ossifying fibroma (cemento-ossifying fibroma) usually presents as a well-demarcated mixed radiolucency/radiopacity with smooth and often sclerotic borders. The lesions are usually solitary and most commonly occur in the mandible. Histologically they contain a relatively avascular cellular fibrous stroma with reticular bone trabeculae and cementum-like zones.
The ossifying fibroma is probably a true neoplasm wich occurs usually in the third and early in the fourth decades. Growth rates of this tumor are variable.
The treatment is surgical: the lesions are easily enucleated at surgery, although there is recurrence, the rate of which varies from 10 to 50 %. When present in the craniofacial complex, treatment may have to be more aggressive to protect the vital structures and in some cases include the partial resection of the affected bone.
Benign non-odontogenic tumours of the jaws
Almost any type of bone tumour can arise in the jaws but most of them are considerably more common in other parts of the skeleton. However, neoplasms derived from bone itself are relatively infrequent in the jaws. Benign nonodontogenic lesions of the jaws represent a mixed group of tumors, which in many cases are difficult to classify (Table 13.3). The main types of them are fibro-osseous displasia, osteoblastoma and osteoid osteoma, benign tumors of bone-forming cells,synovial chondromatosis and osteochondroma, lesions containing giant cells,vascular malformations, Langerhans cell histiocytosis, nonodontogenic cysts ofthe jaws,neurogenic tumors, Paget’s disease, and tori.
Table 13.3. Non-odontogenic tumours of bone
| Primary-benign |
Primary-malignant |
Metastases |
Osteoma
Osteochondroma
Cemento-ossifying fibroma
Central giant-cell granuloma
Haemangioma
Melanotic neuroectodermal
tumour |
Osteosarcoma
Chondrosarcoma
Ewing’s sarcoma
Multifocal or potentially multifocal:
Myeloma Langerhans cell histiocytosis |
Carcinoma |
Osteoma
Osteomas are benign tumors consisting of mature compact or cancellous bone. They may arise on the surface of bone (periosteal osteomas) or centrally within the bone (endosteal osteomas). They are often discovered in the form of a painless hard swelling or as asymptomatic radiopacities.
Osteomas are discovered in all age groups, more commonly during the fifth decade of life. Males appear to be affected more frequently than females (Fig. 13.64; 13.65).

Fig. 13.64. Osteoma of the frontal bone

Fig. 13.65. Osteoma of the mandible condylar with lateral displacement of the jaw
Periosteal osteomas usually present as asymptomatic slow-growing bony masses. Endosteal osteomas are usually asymptomatic and are noted on routine radiographs. Radiographically they appear as well-circumscribed round or oval-shaped radiodense masses (Fig. 13.66).

Fig. 13.66. CT scanning, frontal plane (the same patient)
In cancellous osteomas bone trabeculae with irregular orientation are seen. Histologically they consist of either dense compact bone with sparse marrow spaces or lamellar trabeculae of cancellous bone with fibrofatty marrow spaces. Osteoblastic activity is often predominant.
Gardner’s syndrome is an autosomal dominant condition in which patients have intestinal polyposis, multiple osteomas (usually endosteal), fibromas of the skin, epidermal cysts, impacted teeth, and odontomas. The condition is important because the syndrome exhibits multiple intestinal polyposis and these polyps have the potential for malignant transformation. Urgent referral to a gastroenterologist is therefore needed.
The associated osteomas are often found in the jaws, particularly in the angle region of the mandible, as well as the facial bones and long bones. It has been suggested that any patient with multiple mandibular osteomas should be investigated for the possibility of Gardner’s syndrome. If the diagnosis is confirmed, a prophylactic colonectomy should be performed.
Treatment of osteomas is surgical excision. Asymptomatic cases may be followed up clinically and radiographically without treatment. If the swelling is interfering with function, it can be surgically removed. Following excision, recurrences are very rare. 3-D reconstruction and stereolithographical model using CT scanning can be used for planning of the operation (Fig. 13.67).

Fig. 13.67. 3-D reconstruction and stereolithographical model using CT scanning
(the same patient)
Torus palatinus
The palatine torus appears as a bony hard swelling along the midline of the palate. It can be discrete or may be large and lobular. It usually occurs in the second or third decade of life, and has a tendency to grow throughout life. If torus palatinus is large, it may require surgical removal because of its interference either with speech or feeding or with prosthetic reconstruction. The common surgical approach is via a double Y-shaped incision and subsequent bone removal. The bone is virtually always solid cortical bone and is actually fairly difficult to remove. The recommended technique is to make a number of vertical cuts in the bone with a fissure bur. Then the intervening ridges of bone can be snapped off and a final smoothing of the residual bone carried out, taking care not to perforate through into the nasal cavity. It may be advisable to insert a dressing plate after the procedure to prevent excessive hematoma formation and possible recurrence of the torus.
Torus mandibularis
Mandibular tori are bony exophytic growths that present on the lingual aspect of the mandible opposite the bicuspids or premolars. In most of the cases they are bilateral. They manifest in the second or third decade of life and tend to grow with age. Larger tori may require surgical removal because they interfere with tongue positioning, speech, and prosthetic reconstruction, as well as with oral hygiene around the lower posterior teeth (Fig. 13.68).

Fig. 13.68. Mandibular tori
If surgical removal is required, it is carried out via an extensive gingival margin incision with a possible lingual releasing incision, followed by removal of the bone. This is carried out by making a number of vertical cuts with a fissure bur, and then snapping off the intervening ridges of bone with a periosteal elevator. The residual irregularities are then smoothed with a larger bur. If mandibular tori are on a fairly narrow neck they can be removed totally by mallet and chisel. Recurrence of tori after surgical excision is not typical.
Osteoblastoma and osteoid osteoma
Osteoblastoma and osteoid osteoma are benign tumors arising from the bone tissue. They considered as the variants of the same neoplastic lesion.
The osteoblastoma represents large and more aggressive tumor which occurs in the maxilla-facial area very rarely. In the head and neck, the mandible is the most common site. Clinically osteoblastoma grows rapidly and the main clinical sign is pain, which is generally localized to the lesion itself. Most cases of osteoblastoma occur in the second decade of life. Males appear to be affected more commonly than females.
Radiographic features are variable, usually consisting of a combination of radiolucency and radiopacity. The lesions dimensions are more than 2 cm. They are well circumscribed radiographically with a thin radiolucency surrounding the variably calcified contents.
The histologic appearance shows irregular trabeculae of osteoid and immature bone within a predominantly vascular stromal network. There are various degrees of calcification present. Stromal cells are generally small and slender.
The osteoid osteoma represents a smaller version of the osteoblastoma. It is normally less than 2 cm in diameter clinically and radiographically. It occurs in the second and third decades of life with a male predominance. Pain is also the major clinical feature. Classically, the pain is worse at night and is relieved by acetylsalicylic acid. If the lesion is located near the cortex, it may produce a localized tender swelling. Radiographically the lesion again shows a well defined mixed radiolucency/radiopacity with a small radiolucent rim around the lesion, which is walled by sclerotic bone.
Histologically it resembles the osteoblastoma with a rich vascular stroma, trabeculae of osteoid and immature bone. The bone is rimmed by layers of active osteoblasts. Histologically it is impossible to differentiate it from the osteoblastoma.
Treatment of the osteoblastoma and osteoid-osteoma is surgical excision either with curettage or local resection. Recurrences are rare but have been reported. In these cases more aggressive treatment such as en bloc resection is often necessary.
Chondroma
Chondroma is a benign tumor of mature cartilage. The occurrence of these lesions in the jaws is extremely rare. Most cases appear in the mandibular condyle or anterior maxilla, suggesting that these lesions may arise from cartilaginous remnants. The chondroma presents as a painless slowly progressive swelling, which may result in mucosal ulceration. The gender distribution is equal, and most tumors occur under the age of 50 years. Radiographically they present as irregular radiolucent lesions, although foci of calcification may occasionally be present. Resorption of tooth roots has been reported. Histologically, chondromas consist of hyaline cartilage, but the cells are irregular in size and distribution. Calcification or ossification may develop.
Chondromas of the maxillofacial area are often misdiagnosed with low-grade chondrosarcomas. They also have a high potential to malignant transformation. Because of this the method of choice in treatment of maxilla-facial chondromas is en-block resection of the affected bone. Excision should include a wide margin of normal tissue to ensure the radical removal of the neoplastic tissue.
Giant Cell Tumor and Central giant-cell granuloma
The giant cell tumor is the tumor commonly found in the long bones and its manifestation in the jaws is comparably rare. This lesion is an aggressive tumor originating from the monocitic and macrophage system. Histologically it is very similar to the central giant cell granuloma, except that the giant cells are larger with more nuclei, and they are more evenly spread throughout the lesion and not as focally placed as in the central giant cell granuloma.
Clinically anterior mandible and upper premolar regions are commonly affected. In the mandible, the presence of a tumour may give rise to expansion of the outer and/or the inner cortical plates of the bone (Fig. 13.69; 13.70).

Fig. 13.69. The giant cell tumor
of the mandible

Fig. 13.70. The giant cell tumor
(lytic form) of the mandible
In the maxilla the cortical expansion is less significant. There may be mobility of related teeth and resorption of their roots. Occasionally, the soft tissue of the giant cell tumor may grow through the upper border of the alveolar process and appear as a dark red or mass under the oral mucosa. The lesion is usually non-painful but may be tender to palpation (Fig. 13.71).

Fig. 13.71. The giant cell tumor
of the right maxilla (CT scanning)
Central giant-cell granuloma is an endosteally originating resorptive process causing a cyst-like lesion filled with a very vascular fibrous tissue rich in multinucleated giant cells. Its clinical and radiographical appearance in the jaws may be exactly the same as in the giant cell tumour. The diagnosis is therefore made on histological grounds.
Treatment of the giant cell tumor and central giant cell granuloma is usually performed by local curettage. However the recurrence rate after local curettage is high, and the appropriate treatment is in doubt. In the same cases the bony walls of the cavity are frozen with liquid nitrogen after curettage in an attempt to prevent the recurrence.
Some authorities advocate local resections in cases of large or recurrent lesions.
Hemangioma of the jaws
Hemangeomas and vascular malformations can occur anywhere in the body including jaw bones. True hemangioma is a neoplasm of vascular endothelium and is normally present at birth, often enlarges, and then frequently involutes. The vascular malformation generally is not present at birth, appears later, and does not involute. Vascular malformations can take a number of forms. The most practical classification is to divide them into high-flow and low-flow vascular malformations. The high-flow vascular malformations are either arterial lesions or arteriovenous fistulas. The low-flow malformations are mainly venous in nature. The clinical significance of a vascular malformation is that a central high-flow vascular malformation can cause torrential hemorrhage when surgical intervention ensues. This has been fatal on occasion.
Many of these lesions are asymptomatic and may even be difficult to detect preoperatively on radiographs. If there is a clinical presentation, it is often a slow-growing asymmetric expansile lesion of the jaw, and if it is high flow, it may be associated with a bruit. Radiographically jaw haemangeoma may appear as an irregular poorly defined soap bubble-type lesion, which may cause resorption of the roots of teeth and does not normally cause nerve involvement.
Diagnosis is usually confirmed by computed tomography. In some cases a diagnostic needle aspiration can be carried out preoperatively. If bright red blood under pressure is encountered it is patognomic to high-flow vascular malformations.
Since the radiographic and clinical appearances of a vascular malformation are not diagnostic, the differential diagnosis normally includes a number of odontogenic and nonodontogenic lesions, including the central giant cell granuloma, the aneurysmal bone cyst, ameloblastoma, odontogenic keratocyst, and odontogenic myxoma. All of these lesions should undergo needle aspiration prior to biopsy or surgical treatment to rule out a highflow vascular malformation. When a vascular malformation is suspected or diagnosed, selective angiography is normally performed via a femoral approach.
Treatment
If a vascular tumor of jaw is diagnosed, treatment includes preoperative embolization followed by wide resective surgery. The embolization can involve a number of materials, including muscle, polyvinyl, pellets, and platinum coils, which are inserted via the angiography catheter or on direct puncture. On entering the lesion they unwind and expand.
Postembolization angiography carried out immediately after the embolization normally shows a diminution in blood flow to the lesion. However, because of the powerful angiogenic effect of these lesions (probably by production of angiogenesis growth factor), reestablishment of smaller collateral vessels usually occurs within a few days, and it is often impossible to reembolize these smaller collateral vessels. Therefore, definitive surgery should be carried out within a small number of days after embolization. Definitive surgery normally takes the form of resection under hypotensive anesthesia with adequate resuscitative measures available. Following resection appropriate reconstruction can be performed. Other approaches such as injection of a variety of substances into the lesion including glue, fibrin gel, and platinum coils, for example, have been attempted.
Neurogenic tumors of the jaws
Neurilemmoma (schwannoma) is a benign tumor of the nerve sheath. Although usually found in the soft tissues, it can occur in bone, where it usually exists as a well-defined radiolucency. Histologically lesions are well encapsulated and predominantly of spindle cells showing either an Antoni A (spindle cells arranged in palisaded whorls and waves) or Antoni B (spindle cells with a more haphazard appearance). Following biopsy to confirm the diagnosis, treatment usually consists of surgical excision. Recurrences are rare.
Neurofibroma
Neurofibromas derived from the fibrous elements of the neural sheath and may exist as solitary lesions or as part of generalized neurofibromatosis or von Recklinghausen’s disease. Although most commonly reported in soft tissues, neurofibromas occur in bone affecting most commonly in the inferior alveolar nerve, where they appear as a fusiform swelling in continuity with the inferior alveolar canal. Other bone changes associated with neurofibromatosis can include cortical erosion from adjacent soft tissue lesions or medullary resorption from interosseous lesions. In cases associated with the inferior alveolar nerve, pain or paresthesia can result.
The normally recommended treatment following biopsy is localized excision. The lesions are often vascular, and extensive blood loss has been reported from surgical management of mandibular lesions.
Tumor-like lesions of the jaws
Hyperparathyroidism
Hyperparathyroidism is a pathological condition associated with overproduction of parathormone. Primary is caused by hyperplasia or adenoma of the parathyroid glands. Secondary hyperparathyroidism is due to the conditions that reduce calcium levels in the blood, such as chronic renal disease. Increased levels of parathormone mobilise calcium from the bony skeleton and raises the plasma calcium level.
Post-menopausal women are mainly affected. The major symptoms result from renal damage which leads formation of renal calculi, hypertension or other cardiovascular disease. In the bone, however, where the jaws can be affected, cyst-like spaces known as “brown tumours” may develop. The bone in these tumours is resorbed by vascular fibrous tissue with multinucleated giant cells in profusion.
The mandible is more commonly affected by such lesions than the maxilla. In the mandible, the presence of a brown tumour may give rise to expansion of the outer and/or the inner cortical plates of bone. Occasionally, the soft tissue of the brown tumour may grow through the upper border of the alveolar process and appear as a dark red or purplecoloured mass under the oral mucosa. The lesion is usually non-painful but may be tender to palpation.
Histologically, the cyst-like areas are foci of osteoclasts in a highly vascular stroma. Extensive haemosiderin deposits cause the lesion to appear as a brown tumour.
Radiographically, the main effects are thinning of bone trabeculae, subperiosteal resorption of the bone of the fingers and resorplion of the terminal phalangeal tufts. In severe disease, a well circumscribed radiolucent cyst-like areas often with a multiloculated appearance are a typical but rare finding. Alveolar bone may also be resorbed but reforms with treatment. The out-line may have a scalloped margin lamina dura surrounding the cyst is less defined than is normally found in a true cystic lesion.
In patients with hyperparathyroidism there are characteristic changes in blood chemistry and multifocal involvement of different bones. Biochemical findings in primary hyperparathyroidism include raised plasma calcium (2,8 mmol/1 or more), low plasma phosphorus (less than 0,8 mmol/1), elevated levels of parathormone in plasma, raised plasma alkaline phosphatase (over 100 IU/1). Blood chemistry examination is essential in patients same histological picture of osteoclastic proliferation. Occasionally, bone lesions cause pathological fractures. The increased excretion of calcium leads ultimately to renal calcmosis or stone formation and renal damage.
Treatment and Prognosis
Primary hyperparathyroidism is normally treated surgically by removal of an adenoma of the parathyroid gland. The bone lesions usually resolve spontaneously following this surgery. For secondary hyperparathyroidism the renal failure should be treated if possible. Bone lesions may respond to oral administration of vitamin D, whose metabolism is abnormal as a result of the renal disease.
Paget’s disease of bone (osteitis deformans)
Paget`s desease is characterized by irregular resorption of bone with subsequent redeposition which disrupt normal bony architecture. It is a slowly progressive bone condition of unknown etiology, predominantly affecting males over the age of 50 years, which causes bone distortion and weakening. Bone resorption and replacement becomes rapid, irregular, exaggerated and purposeless. The changes progress erratically but the ultimate result is thickening of affected bones without localised swellings.
During the resorptive phases, areas of bone may be severely resorbed, leading to distortion under normal weight bearing function. There may be pain in the bones, large vascular regions in the medullary spaces. In the formative phase, occlusion of bony foramina can prove a problem and the relative avascularity following redeposition of bone can then make infection in bone more difficult to manage. Since closely adjacent parts of the bone may show different stages of the disease, a common result is the patchy area of osteoporosis and of sclerosis.
The cause of the disease is unknown. One of the possible mechanisms is the delayed or slow reaction to a myxovirus or other virus stimulus in both osteoblasts and osteoclasts. A genetic factor may also be involved.
Bones most frequently affected are sacrum, spine, skull, femora and pelvis. Vertebral column and lower limbs in severe cases are unable to deal with the forces and deform as a result. The disease may be widespread and is usually symmetrical, but sometimes a single bone is affected.
In the uncommon severe form, the main features are an enlarged head, thickening of the weight-bearing long bones, and tenderness or aching pain which can be severe and almost intractable. The vault of the skull is more often affected than the facial skeleton, and the maxilla considerably more frequently than the mandible.
When the jaws are affected, the alveolar process becomes symmetrically and grossly enlarged. The classic presentation used to be a patient whose hat no longer fitted correctly, or in whom false teeth, particularly the maxillary denture, did not fit owing to bone swelling. There may also be gross and irregular hypercementosis of teeth, which may become fused to sclerotic areas of the bone (Fig. 13.72; 13.73). Attempts to extract affected teeth may succeed only by tearing away a large mass of bone. Severe bleeding or osteomyelitis of ischaemic bone may follow. Narrowing of foramina can occasionally cause cranial nerve deficits and severe headaches.
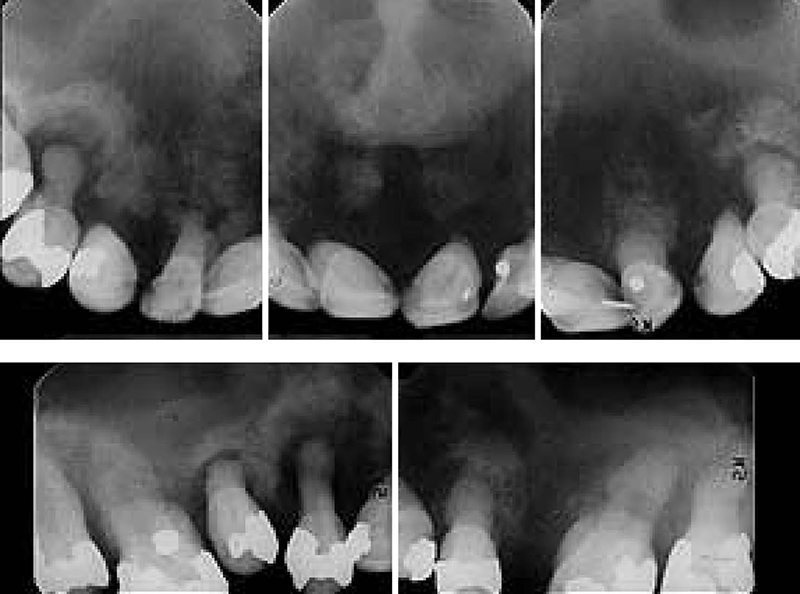
Fig. 13.72. Pagets desease
(by H. O. Sedano)

Fig. 13.73. Pagets desease, irregular hypercementosis of teeth
Sarcomatous change has been reported in 5 to 15 % of patients with Paget’s disease, which should be considered a premalignant condition.
The main radiographic features are lower density of the bone in the early stages and sclerosis in the later stages. Radiographs show patchy areas of radiolucency interspersed with radio-opaque density. The term “cotton wool” is often used to describe these changes in the skull and maxilla of affected patients. Hypercementosisi observed around the roots of teeth, as well as loss of lamina dura and obliteration of the periodontal ligament space. Root resorption has also been noted.
The main histological changes are the irregular pattern of reversal lines, many osteoblasts and osteoclasts (often abnormally large), fibrosis of the marrow spaces and increased vascularity. Bone biopsy show irregular areas of resorption or evidence of previous resorption in the form of reversal lines. These are heavily staining haematoxilin lines, which denote the boundary of previous resorptive activity. Their irregular pattern characteristically produces a mosaic appearance in the bone. In the late stages, affected bones are thick, the cortex and medulla are obliterated and the whole bone is spongy in texture.
Blood samples may show very high levels of alkaline phosphatase that may reach 700 u/1with normal values for calcium and phosphate.
Treatment and Prognosis
Treatment of the Pagets disease is both systemic and local. Systemic treatment includes the usage of calcitonin and bisphosphonates to inhibit bone resorption. Calcitonin can be taken either subcutaneously or by nasal spray and is more effective for reducing bone pain and osteolysis, but can cause nausea and an unpleasant taste. Calcitonin is also given preoperatively to reduce bleeding from the highly vascular bone and may help to relieve cranial nerve deficits.
Bisphosphonates can be given orally or by injection. They have a direct effect on hydroxyapatite crystals, which make the bone less receptive to resorptive activity and hence reduce the rate of turnover. Treatment causes stabilization of the bone and a lowering of the raised alkaline phosphatase levels.
Local treatment is directed to cosmetic and/or functional recontouring of bone. It should be noted that the bone of Paget’s disease is often vascular, and bleeding during recontouring can be extensive. However, healing is often delayed owing to the intervening sclerotic areas of bone.
Dental problems may be encountered in the form of excessive bleeding if the area of the jaw affected is undergoing active resorption, and infection can be a complication where the bone has reformed and become relatively avascular. Added to these problems may be hyper cementosis of the roots resulting in large-rooted teeth that may be difficult to extract conventionally. Prophylactic antibiotics are often prescribed for extractions if the bone is sclerotic.
Fibrous dysplasia
Fibrous dysplasia is a developmental hamartomatous disease of unknown etiology. It may represent developmental arrest in a benign fibro-osseous proliferation that lacks the ability to fully differentiate. In fibrous dysplasia a replacement of normal bone by an immature bone with extensive vascular fibrous tissue elements is present. In majority of cases this condition manifests in children. The abnormality may affect many bones (polyostotic) or one bone (monostotic), and the maxilla is far more commonly affected than the mandible. Two rare variants are also identified, one being cherubism and the other Albright’s syndrome, which is a form of polyostotic fibrous dysplasia with additional features of skin pigmentation and precocious puberty in females. Fibrous dysplasia is usually self-limiting and tends to “burn out” on completion of skeletal growth (Fig. 13.74). It can, however, cause quite marked disurement in severe cases and in the polyostotic form can encroach on bony foramina leading to compression of nerves.

Fig. 13.74. Fibrous dysplasia of the maxilla and the mandible (diffusive form)
The jaws are commonly associated with all forms of fibrous dysplasia. In the jaws the onset is usually during the first and second decades, and it produces painless swelling of the involved bones.
In the monostotic form, the usual presentation is a painless enlargement of the jaw on the affected side. Buccal and palatal aspects of the alveolar bone may be enlarged and expanded and this may cause spacing between the teeth compared to the unaffected side. The occlusion, however, is seldom significantly affected other than the spacing and the teeth erupt normally and are not unduly mobile. The overgrowth can usually be seen as a facial asymmetry with fullness of the cheekbone and nasolabial fold.
Classically, the radiographic appearance shows a weak opacity without clearly defined borders and a fine orange-peel texture and an eggshell-thin cortex of expanded bone. The degree of radiopacity depends on the amount of lesional bone which may give a predominantly radiolucent or more sclerotic appearance. The key feature is that the margins merge imperceptibly with the surrounding normal bone (Fig. 13.75).

Fig. 13.75. Fibrous dysplasia, deformation of the alveolar ridges, adentia, displacement of the teeth (the same patient)
In its cranio-facial form the maxilla, zygoma, sphenoid, frontal bones, nasal bones, and base of the skull can be involved. Expansion can cause compression of nerves and blood vessels. The optic canal can be narrowed by fibrous dysplasia, although it seems unlikely that any associated vision loss can be relieved by orbital decompression.
Typically lesions undergo periods of activity and periods of quiescence. When they are active, they are often symptomatic in that the patient may perceive a throbbing or discomfort, the swelling increases, and the lesions appear hot on a bone scan and can mimic osteomyelitis. In a quiescent phase they may be totally asymptomatic.
The diagnosis is normally made on three grounds: the age of the patient and clinical features described; the radiographic appearance and the histopathology. Radiographs of the affected bone or bones typically show a granular appearance that has been likened to ground glass. There is an obvious excess of this abnormal bone and it merges with the normal appearance of bone without a clearly defined separation.
A bone biopsy will generally show loose cellular fibrous tissue containing slender trabeculae of woven bone of variable shape which merge imperceptibly into surrounding normal bone. Osteoblasts are scattered throughout the substance of the trabeculae rather than surrounding them. Some lamellar bone or calcified spherules and occasional loose foci of giant cells can also be seen.
Bone biochemistry is usually unhelpful, with calcium, phosphate and alkaline phosphatase levels within normal limits. The alkaline phosphatase level, which is a measure of osteoblastic bone formative activity, may be raised if the sample is taken during an active growth phase of the child, and its relevance is therefore almost impossible to determine.
Although not normally recognized as a premalignant lesion, sarcomatous change has been noted in fibrous dysplasia. Early cases appear to have been associated with the use of radiation therapy for treatment, but cases of spontaneous sarcomatous degeneration have been noted. Additionally, some cases have been difficult to diagnose and may have represented a low-grade osteosarcoma from the outset. For operation planning CT scanning, 3 D reconstruction of the facial scull’s bones is used frequently (Fig. 13.76).

Fig. 13.76. CT scanning, 3-D reconstruction of the facial scull’s bones
Albright’s syndrome comprises polyostotic fibrous dysplasia, skin pigmentation and sexual precocity. Polyostotic fibrous dysplasia involves the head and neck region in up to 50 % of cases. A jaw lesion may then be the most conspicuous feature and polystotic disease may not be suspected initially. In a young girl in particular, investigation for other skeletal lesions and pigmentation may therefore be indicated. Skin pigmentation consists of brownish macules which frequently overlie affected bones and appear especially on the back of the neck, trunk, buttocks, or thighs, but hardly ever on the oral mucosa.
Treatment
The disease is self-limiting, but grossly disfiguring lesions may need to be excised. If the lesions are asymptomatic, a biopsy diagnosis alone may be adequate without carrying out any definitive treatment. Surgical treatment should be also limited during an active phase because the lesions are vascular and can bleed quite profusely. Treatment is best reserved for quiescent periods, at which time cosmetic recontouring is the normal treatment of choice. In some cases more aggressive surgical procedures including mandibular and maxillary resections are used.
Cherubism
Cherubism is a familial genetically dominant condition regarded as a form of fibrous dysplasia. It is characterised by an increased width and fullness of the angles of mandible bilaterally (Fig. 13.77). The bone itself is immature in these regions with areas of vascular fibrous tissue. Affected family members often have multiple lesions mainly affecting the facial bones. Because of the involvement of the maxilla and orbital floor, the face has a rounded appearance and the eyes tend to look upward, giving the patient a cherubic appearance. The genetic defect in this condition has been identified on chromosome 4p16.3. Like other genetic diseases, many non-familial cases are seen as a result of new mutations.

Fig. 13.77. Cherubism (child 6 years old)
Expression is variable, with some patients having subclinical lesions discovered only on radiographs and some having extensive and clinically obvious lesions.
The onset is typically between the ages of 6 months to 7 years, but rarely is delayed until late teenage or after puberty. Typically, symmetrical swellings are noticed at the age of 2 to 4 years in the region of the angles of the mandibles and, in severe cases, in the maxillae. The symmetrical mandibular swellings give the face an excessively chubby appearance. The alveolar ridges are expanded and the mandibular swellings may sometimes be so gross lingually as to interfere with speech, swallowing or even breathing, but the rapidity of progress is variable. Expansion of the maxillae may also cause stretching of the skin and some retraction of the lower lids. Maxillary involvement can also cause the palate to assume an inverted V shape.
Teeth are often displaced, and in active periods the lesions are extremely vascular. Despite lack of inflammation, there is frequently cervical lymphadenopathy, due to reactive hyperplasia and fibrosis.
This is typically seen in the early stages and may completely subside by puberty.
Radiographically the lesions appear honeycombed and can be very extensive. The angles of the mandible are particularly involved but the process extends towards the coronoid notch and sometimes also forwards along the body. The lesions simulate multilocular cysts as a result of fine bony septa extending between the soft tissue masses. Panoramic radiographs help to determine the extent of the disease but it is more clearly visualised by CT scanning.
Histologically the lesions are very similar to central giant cell granuloma, with focal accumulations of giant cells in a spindle cell matrix. Perivascular cuffing is often present, and in some cases can be used to differentiate the two lesions.
Treatment of cherubism is usually conservative and expectant and into the teenage years is devoted to trying to aid eruption of the teeth, which is often abnormal. Later it is directed toward cosmetic recontouring of the affected bones. The lesions normally become less active and less vascular toward the end of the second decade and into the third decade, and it is at this time that most cosmetic remodeling is carried out. If disfigurement is severe the lesions respond to curettage or to paring down of excessive tissue but, in the early stages the recurrence rate is high.
Langerhans cell histiocytosis
Langerhans cell histiocytosis is the term currently employed for what was previously known as histiocytosis X, and before that the three separate conditions Letterer – Siwe disease, Hand – Schuller – Christian disease, and eosinophilic granuloma. Letterer – Siwe disease represent the acute disseminated form of Langerhans cell histiocytosis, whereas Hand – Schuller – Christian disease represents the chronic disseminated form, and eosinophilic granuloma represents the chronic localized form.
The cells of origin of this disease have now been identified as the Langerhans cells, which are dendritic cells in the skin and mucosa that have a macrophage-like function. At the present time what causes these cells to proliferate in a clonal fashion with phenotypic evidence ofactivation and give rise to Langerhans cell disease is unknown. Some studies suggested that it may have some of the properties of a tumor or have a viral etiology.
The acute disseminated form usually affects young children. It is multisystem in nature, affecting the skin, bones, and internal organs (especially lungs and liver), and is frequently fatal. Treatment is chemotherapy.
The chronic disseminated form of the disease is classically associated with a triad of punched-out bone lesions (often affecting the skull and jaws), diabetes insipidus (owing to posterior pituitary involvement), and exophthalmos (owing to deposits in the posterior orbit). This normally affects an older age group, often in the second and third decades but sometimes much older.
The treatment of the chronic disseminated form of the disease is variable. and for well-circumscribed lesions can consist of local curettage. However, for more aggressive forms, chemotherapy is frequently employed as well. Low-dose radiation therapy has also been used on isolated lesions, and it does remain one of the very few indications for low-dose radiation therapy.
The chronic localized form of the disease (eosinophilic granuloma) is commonly found in the jaws and usually shows as a well-defined radiolucency, often in the bicuspid region and more frequently in the mandible. The bone lesions often affect the jaws. Although they usually appear as fairly well-defined punched-out radiolucencies, they can also be less well defined and can affect the apices of the teeth only and lead to a possible differential diagnosis of periapical infection. A frequent aspect of presentation is loose teeth; radiographically they often appear as “floating teeth”. Treatment usually consists of aggressive local curettage, and the recurrence rate is low.
Chapter 14. Malignant tumors of the maxillofacial area and neck
Cancer means a malignant tumor of epithelial origin. Approximately 5 % of all malignant tumors fall on cancer of vermilion border and oral mucosa. The most frequently affected areas are red border of the lip (posterior area), tongue (lateral surface) and floor of the mouth. The majority of patients with cancer of vermilion border and oral mucosa are men at the age older than 40 years.
The majority of patients with cancer suffered previously from some of the diseases of oral mucosa and vermilion border called precancerous diseases. The reasons of their occurence are traumas, in particular chronic ones, smoking, betel and tobacco chewing, alcohol consumption. Traumas are considered to be external factor of cancerogenesis. Cancer is often associated with proliferative processes, benign tumors, chronic inflammatory diseases accompanied by erosions and chancres. Precancerous disease exists for a long time (from several months to decades), then it can transform into (not necessarily) cancer. Prompt diagnostics and treatment of precancerous diseases eliminates threat of cancer development or enables to undertake timely, more efficient and harmless treatment.
With respect to probability of malignization there are obligate and facultative pretumor processes. Obligate precancers cause cancer development in different periods if not treated in time. In the majority of cases they are cancer in situ from the very beginning. Facultative precancers cause cancer not always.
Classification of pretumor processes of oral mucosa
With high frequency of malignization (obligate): morbus Bowen.
With little frequency of malignization (facultative):
- verrucuos and erosive leukokeratosis;
- polypapilloma;
- erosive ulcerous and hyperkeratotic forms of erythema centrifugum and lichen acuminatus;
- postradial stomatitis.
Classification of pretumor processes of red border
With high frequency of malignization (obligate):
- verrucous precarcinoma;
- limited precancerous hyperkeratosis;
- abrasiva praecancerosa cheilitis Manganotti.
With little frequency of malignization (facultative):
- leukokeratosis;
- keratoacanthoma;
- cutaneous horn;
- papilloma with cornification;
- erosive ulcerous and hyperkeratotic forms of erythema centrifugum and lichen acuminatus;
- postradial cheilitis.
Morbus Bowen
Bowen was the first to describe this disease in 1912. From the very beginning it appears to be cancer in situ.
Clinical presentation. The affected area is as a rule single hyperemic bright red spot, smooth or with velutinate surface due to small papillary projections. The central area resembles leukokeratosis with pit-and-mount surface or lichen acuminatus with cornification focuses on hyperemic background. Due to atrophy of mucosa, the focus falls in slightly compare to surrounding areas, slightly bleeding erosions can appear on it. The affected area is from 1–2 mm to 5–6 cm, its contours are not smooth but rather distinct. Induration in its basis is not determined. If lesion is localized on the tongue, lingual papillae at affected area disappear. Regional lymph nodes are not palpable as a rule. Subjective sensations are minor but in cases of erosions tenderness can be present. Clinical presentation of Morbus Bowen on oral mucosa is not always apparent. The disease can manifest only by the small area of hyperemia or resemble leukokeratosis without evident inflammation. The disease may be present for indefinite time, in some cases invasive growth advances and traumatization accelerates this process, in other cases the disease remains at stage of cancer in situ. The diagnosis must be confirmed by histological study. Pathomorphologically morbus Bowen is characterized by signs of intraepithelial epidermoid cancer: polymorphism of spicular layer cells up to atypia, increase of mitosis number, its impairment, presence of giant cells, multinuclear cells, acanthosis, and in several cases hyperkeratosis and parakerathosis. The basal membrane and basal layer are preserved. There is small infiltration with lymphocytes and plasmocytes at the upper part of stroma.
Differential diagnostics includes leukoplacia, lichen acuminatus, chronic traumatic affection.
Praecancer verrucosus
It was described by A. L. Mashkilleison in 1965. It appears almost in all cases on the lower lip and resembles painless semiround node with verrucous surface 4–10 mm in diameter. The color of the node is from nearly normal coloring of vermilion border to stagnant red one. At the top the node is covered with hardly removable grey scaly crusts. The lesion is located on intact vermilion border but the signs of the small hyperemia may be present in some cases.
Histologically the signs of limited epithelium proliferation are revealed due to expansion of belemnold layer, in some cases hyperkeratosis and parakeratosis, polymorphism of cells of belemnold layer of different manifestation rate, even violent one. Basal membrane is preserved. Transfer into invasive cancer type appears quickly – in 1–2 months after beginning of disease. Differential diagnostics must be performed with papilloma and verruca. The diagnosis is confirmed by histological examination.
Hyperkeratosis praecancrosa circumscripta
The lesion is polygonal cornification locus not bigger than 2 mm. The affected area in majority of patients is covered with the mucous coat, often falls in slightly but it can be a little bit raised with flat surface covered with thin closely placed scaly crusts, which can not be removed by scraping. Palpation reveals superficial lamellar induration. Background changes are absent; this cancer type appears more rarely on the background of non-specific inflammation.
Histological examination reveals the limited acanthosis area, cells discomplement and polymorphism is often seen as well as hyperkeratosis on the surface. Differential diagnostics is carried out with leucoplasia and lichen acuminatus. Malignization occurs after some months or years.
Cheilitis abrasiva praecancrosa Manganotti
This type of precancerous lesions was identified and described by Manganotti in 1933. It occurs predominantly in men over 50 years. Traumas, insolation, herpes may cause the emergence of this disease.
Clinical presentation. Unlike low-grade limited or expanded chronic catarrhal inflammation of the lower lip one or rarely several red anabrosis with flat surface are seen. They can be sometimes covered with tight blood-tinged or serous crust, which is hard to remove. Anabrosis uncovered with scab tends to bleed. Induration at the base of the lesion is absent. Anabrosis can be hardly treated with ointments and applications of topical medications. Existing for a long time they can epithelize but then they appear again at the same or other areas. Histologically the deficiency of epithelium is observed as well as inflammatory infiltration in underlying connective tissue. Epithelium on the anabrosis edges is in the state of acanthosis or is atrophic. Epithelial bundles deviate deep into stroma. In some areas acanthocytes demonstrate different rate of discomplement and atypia. Cytological examination can reveal the signs of dyskariosis of epithelial cells, inflammatory elements but more often only inflammation. The process lasts from 1–2 months up to many years. If not treated it undergo malignization, which manifests clinically by induration of the anabrosis base and surrounded areas, emergence of papillary projections on the surface of anabrosis, its bleeding and cornification around the anabrosis. The diagnosis is confirmed by revelation of atypical cells in scrapes from the diseased area or by results of histological examination. The differential diagnostics must be performed with anabrosis forms of leukoplasia, lichen acuminatus, erythema centrifugum, vesicular fever, herpes iris, actinic cheilitis, herpetic anabrosis.
Treatment. It is necessary to remove properly all local irritators, and then oral cavity sanation must be executed including adequate prosthesis, smoking and consumption of irritating food must be forbidden, removal of insolation is also recommended. It is necessary to reveal and to treat accompanying diseases of other organs and systems. Vitamin A is prescribed intraoraly (solution of retinol acetate in oil 3.44 % or solution retinol palmitate in oil 5.5 %) 10 drops 2–3 times per day, as well as other polyvitamins. Applications with oil solution of vitamin A are prescribed topically, in case of baseline inflammation – ointments with corticosteroids and antibiotics. Nonsurgical therapy must not be carried out for more than 1 month. The best results are achieved by surgical removal of focus in the limits of healthy tissues. Only in case of Manganotti cheilitis the nonoperative treatment is permitted. The treatment of all types of obligate precancer is surgical procedure – full dissection of the diseased area in the limits of healthy tissues followed by immediate histological examination. Dissected tissue is surveyed by means of preparation of serial sections. Operation must be preceded by oral cavity sanation and removal of irritators. If operative treatment is impossible, radiation therapy is required.
Cornu cutaneum
Cornu cutaneum is limited hyperplasia of the epithelium with strong hyperkeratosis that resembles horn taking into account its appearance and solidity. It occurs on vermilion border, more often on lower lip, and is characteristic for people over 60, it is nontender. Its color is grey or grey-braun, diameter is up to 1 cm, length is up to 1 cm. Cutaneous horn is a long lasting disease (for years). Emergence of inflammation and induration around horn base, intensification of cornification are the main signs of its malignization. The diagnosis is confirmed after removal of lesion and its histological examination. Surgical treatment is removal of cutaneous horn in the limits of healthy cells.
Keratoacanthoma
Keratoacanthoma is epidermal benign tumor that develops quickly and regresses spontaneously (Fig. 14.1). The disease occurs on vermilion border, rarely on tongue. Keratoacanthoma appears as a grey-red solid papule with choanoid deepening in the center filled with horn mass that can be easily removed. The tumor grows rapidly and in a month it reaches its maximum dimensions (2.5 × 1 cm).

Fig. 14.1. Keratoacanthoma of the lower lip
Keratoacanthoma is nontender, movable and do not infiltrate surrounding tissues. In 6–8 months the tumor either regresses spontaneously and disappears leaving a scar or becomes malignant one and causes cancer. Keratoacanthoma must be distinguished from verrucous carcinoma and precancer. Cancer has firmer texture, solid base, after removal of horn masses bleeding emerges. Surgical treatment of keratoacanthoma is ligatory.
Skin cancer
Skin cancer is the most common tumor in European population. In the majority of cases it can be revealed even at early stages without any special diagnostic procedures so people begin treatment in more than 90 % of cases. Despite the fact that ultraviolet sun beams do not always cause skin carcinoma, in people with insufficient melanin pigmentation of skin the beams with wave length of 290–320 nm are the main, and very often the single, cause of the disease. This means that carcinoma develops more often on open skin areas. Genetic factors play also an important role in the development of skin cancer (cancerogenese). Such rare heritable diseases as albinism, xeroderma pigmentosum, syndrome of nevoid basal cell epithelioma are conditions that are also associated with increased risk of skin cancer development. Usage of effective sun-protective means by these patients contributes to decrease of disease risk. Chemical carcinogens, in particular inorganic compounds of arsenic and some organic hydrocarbons, belong to independent or additional reasons of skin cancer, especially its epidermoid type. Pathogenetic mechanisms of carcinoma development at ultraviolet irradiation and effect of chemical substances are similar. Ionizing radiation including simple X-rays and rays with wave length 0.1–0.3 nm
and also gamma-rays have cancerogenic effect. Skin cancer as well as cancer of other organs develops more often under conditions of immune insufficiency, for example in lymphomas and immunodepressants treatment.
It was proved that influence of ultraviolet rays on skin is accompanied with immune insufficiency as a result of:
- destruction of activating lymphocytes Ia-antigens at the surface of lymphoid cells;
- failure of immune response;
- induction of suppressor lymphocytes;
- disappearance of functionally active Langerhans cells from epidermis (these cells play an important role in contact dermatitis development and other types of retarded hypersensitivity reaction). Despite the fact that any type of skin cells can be subjected to malignant transformation the basal-cellular and planocellular carcinomas develops more commonly.
Basal-cellular carcinoma. This type of cancer embraces more than 75 % of all skin tumors. It develops from epidermis and its cells are similar to intact basal cells. The slight tends to ordinary differentiation into keratin-producing squamous cells is commonly observed. Although these tumors metastasize very rarely, they show high local invasiveness and if effective and immediate treatment is not carried out, they can spread on the surface and ingrain deeply into underlying structures including nerves, bones, brain. Like the majority of cancer types the skin carcinoma is characterized by its indolence so it is often underestimated during long period. Typical basalcellular carcinoma appears to be an uninflamed papule with smooth wax surface that looks transparent at first sight. As a rule telangiectatically enlarged vessels can be seen near it. The tumor may contain certain amount of melanin pigment in form of small dots. These papules exulcerate and incrustate.Ulcers can reepithelize, the patient takes it incorrectly as good signs. Basal-cellular carcinoma can occur in other forms including subtle infiltration lesions not protruding over skin surface or fibrosis lesions resembling scars. In order to verify the diagnosis it is necessary to perform ordinary biopsy. Probably the patient with one canceromathose papule has other co-existing or developing ones in the forthcoming years. Some patients consult a doctor when they notice multiple primary basal-cellular carcinomas. Despite the absence of any visible skin alterations preceding the development of basal-cellular carcinoma, it is usually characteristic for persons who have got stigmas on skin areas exposed to sun or X-ray irradiation. The treatment depends on dimensions, depth and localization of tumor, sex, age and patient’s condition and, of course, abilities and qualification of a doctor. Judging by its cosmetic effect, no intervention can be compared with simple tumor resection (of course, if it is sufficient). Curretage (scraping) and electrocoagulation of minor basaliomas (as well as treatment with X-rays) provide total recovery of more than 95 % patients. Similar results can be achieved by cryodestruction of tumor tissue with liquid nitrogen, by the way this method is cosmetically more reasonable. Better results (recovery in nearly 99 % patients) can be achieved by tumor resection layer-by-layer under microscopic control (Mouh’s method). It is recommended in cases of reluctant and recurrent carcinomas not exposed to effect of other treatment means. Local chemotherapy using 5-fluorouracil is not recommended as a routine method of treatment of basal-cell carcinomas but it can turn out to be efficient in multiple superficial lesions. Immunotechniques of treatment are under exploitation. The patients must be aware of effect of ultraviolet rays in development of malignant skin tumors and methods of protection. It should be recommended for them to wear clothes which protect them from effects of sun beams, to avoid the influence of direct sun beams, in particular at midday, and to use special sun-protective means with protective action coefficient 15. After appearance of every new basal-cell carcinoma, it is necessary to carry out examination of the patient 1–2 times a year during 5 years. In 97 % cases it anticipates in the form of metastases and only in 3–5 % cases new basaliomas emerge on places of its former focuses. It is necessary to take into account the fact that patients with skin carcinoma have the higher risk of development of additional tumors.
Epidermoid carcinoma
This type of carcinoma also develops from epidermis but shows apparent planocellular differentiation and ability to produce keratin. These tumors are characterized by different predisposition to metastasis depending on their dimensions and localization, volume and depth of infiltration and also on the fact whether it develops from premalignized focus (scar tissue on places of burns, chronically inflamed skin areas) or from normal epidermis. Typical epidermoid skin carcinoma resembles solid nontender papule or red patch with apparent superficial cornific scaly crusts that can be ulcerated and covered with crusts. Relatively undifferentiated epidermoid carcinoma does not produce enough keratin so at its surface crusts can be absent. Unlike basal-cell carcinomas the epidermoid skin cancer usually develops from preexisting focus of actinic (sun or solar) keratosis. These precancer keratosis appear to be squamate scabrous red patches on skin areas chronically exposed to insolation. Despite the fact that only a small part of actinic keratosis advance to skin cancer, the most malignant type of epidermoid carcinoma develops from them. This type of epidermoid carcinoma metastasizes rarely (less than 2 % of all cases). Nevertheless, due to potential danger of malignant transformation of sun keratosis, it is recommended to remove them, particularly in persons of juvenile age. At present it is thought that applications of 5-fluoruracyle (1–5 %) in form of ointment or lotion (fomentation) are the most effective ones and as a result of this treatment scars usually do not transform into skin cancer.
Cryosurgical method of treatment using liquid nitrogen is also effective but it is fraught with high risk of cicatrisation. Epidermoid skin cancer developing in mucous coats, mucocutaneous areas, at places of burn scars, chronic ulcers, in atriums or in nearly healthy skin tends to metastasize. At the in situ stage epidermoid skin carcinoma is known under the name of Bowen disease. Despite the fact that epidermoid cancer in situ can develop as a result of chronic influence of sun beams, it is predetermined more frequently by preceding (accidental or due to therapeutic procedures) contact with inorganic compounds of arsenic, moreover from the moment of contact to disease development 10 years may pass. These patients have increased risk of respiratory, urogenital and gastrointestinal carcinoma development. The patients with epidermoid skin cancer must be carefully examined in terms of metastases revelation in order to work out the adequate treatment modality. If metastases are absent, the tumor is treated in the same manner as basal-cellular carcinoma. In this case it is more preferred to resect skin lesion or to use radio therapy to suppress potential metastases. In case of major local or metastatic lesions systemic treatment is used, sometimes local perfusion is applied.
Patients with epidermoid skin cancer should be warned to avoid ultraviolet irradiation and they should be under supervision of doctor at least during 5 years to control local recurrences, development of additional primary focuses and sometimes metastases in internal organs.
Cancer of oral mucosa and cancer of vermilion border
Malignant tumors of mouth and guttur tunica mucosa make total of nearly 5 % of all human tumors. They occur in men more frequently than in women, more commonly at the age 40–60 years.
Etiology
It is suggested that in the majority of cases cancer develops within pathologically changed tissues. As a rule it is long-lasting inflammatory processes of various etiology and dyskeratosis belonging to so called precancer. Such bad habits as smoking, abuse of strong drinks, consumption of “nasa” in Middle Asia and chewing of betel leaves in India, play an important role in development of pathological processes in mouth cavity. We can also mention such factors as chronic mechanical trauma caused by destructed crown of tooth, sharp edge of filling or poor quality prosthesis. Nutrition plays a definite role in development of pretumor conditions. Insufficient content of vitamin A in food or failure of body accessibility cause changes in cornification processes. Systematic consumption of very hot and spicy food is also harmful to oral mucosa.
In the majority of cases cornific epidermoid cancer, rarely non-squarmous one, develops on vermilion border and in oral mucosa. The clinical course of early cancer forms depends on preexisting diseases and tumor growth (exophytic, endophytic, mixed forms). At first cancer can proceed without serious consequences but in cases of tongue localization severe, irradiating pain often appears. Authors distinguish papillary, infiltrative and ulcerous forms of the oral cancer judging by external view at the beginning of disease.
Papillary form. At first a limited induration in form of papillose excrescence on wide base or on pedicle appears. Its surface is covered with papillary projections and horn masses (Fig. 14.2). Palpation reveals superficial infiltration around its base. Tumor grows in scope and depth, necrotic changes develops rather quickly in the center resulting in ulcer formation.

Fig. 14.2. Cancer of the tongue papillary form
Infiltrative form of the cancer is the most unfavourable one (Fig. 14.3). At the beginning of disease nontender induration emerges, it is often located under the mucous layer. Infiltrate grows, necrotize in the central areas and typical cancer ulcer occurs.

Fig. 14.3. Cancer of the tongue infiltrative form
Ulcerous form is the most common one because in the majority of cases a tumor begins to decay at early stage and resembles anabrosis and then ulcer. At the beginning of invasive growth the cancer is characterized by induration around an ulcer in form of roller and in its base being revealed by touch. At primary stage the induration is minor or it is not even revealed clinically, then due to rapid growth of tumor it increases reaching sometimes stone-like density.
At later stages the differentiation of forms is not possible, ulcerous infiltrative growth prevails (Fig. 14.4).

Fig. 14.4. Cancer of the tongue ulcerous form
As a rule an ulcer has raised twisted solid edges, irregular grainy bottom covered with grey-yellow fur or grey necrotic fur in the oral cavity; on vermilion border an ulcer is covered with solid grey fur or bloody grey crusts in case of bleeding. Inflammatory processes in surrounding tissues may be evident or clinically absent. Traumas caused by sharp edges of teeth, prostheses, consumption of hot food, smoking, burning etc. speed up the growth of tumor. It is forbidden to use burning means for ulcers of any etiology but it is dangerous in cases of malignant tumors in particular. After appearance of cancer metastases into lymphatic nodes they gradually consolidate, increase and then infiltrate surrounding tissues. Tongue cancer gives metastases very early; probably it is due to its high mobility.
Cancer of the oral cavity and vermilion border belongs to cancers of visual localizations that facilitates its diagnostics, enables to undertake examination and palpation of diseased area without special equipment (Fig. 14.5).

Fig. 14.5. Cancer of the oral cavity and vermilion border
Using stomatoscope you can observe earlier morphological changes. Clinical diagnosis must be confirmed with morphological investigations – the cytological or histological method. The cytological method of investigation enables to make a correct diagnosis in 90–95 % cases. The material for the cytological investigation is taken by means of scraping or puncture. Differential diagnostics of cancer must be carried out with respect to leukoplasia, benign tumors, traumatic and trophic ulcers, specific diseases (tuberculosis, syphilis, and leprosy), ulcers at lichen acuminatus and other chronic inflammatory processes.
Cancer of the buccal mucosa has the same histological presentation as in case of tongue cancer and oral cavity cancer. However, malignant tumors of minor salivary glands can rarely occur in this area. The buccal mucosa often became infiltrated by tumor secondarily from the side of tonsils, lip and skin. At fist reference to doctor regional metastases are seen rarely, the exceptions are tumors localized in the retromolar area and spreading onto tonsils and palatal arches.
Cancer of the palate mucosa – malignant tumors develop more frequently on the hard palate, they develops from minor salivary glands (cylindromatous carcinoma – cylindroma, adenocarcinoma). Composite tumors (polymorphous adenomas) occur rarely, their differential diagnostics is very often difficult even for histologists. Epidermoid cancer develops on the hard palate rarely. On the soft palate primary growths originating from minor salivary glands occur rarely and epidermoid cancer embraces the absolute majority of tumors. This morphological peculiarity of tumors of hard and soft palate impacts their clinical course.
Epidermoid cancer of the hard palate ulcerates rather quickly causing unpleasant feelings or pain. The patients usually consult a doctor when tumors are not very large.
New growths originating from minor salivary glands remain encapsulated for a long time sometimes becoming sizeable. These patients have the first and the main complaint – presence of tumor on the hard palate. With the increase of its size the pressure of the tumor upon the mucous coat increases and ulceration is commonly seen, then infection and aches develops. It should be noted that at early stage adenocarcinomas and composite tumors of hard have the same clinical picture with tendency to encapsulated growth for a long time. Then adenocarcinoma grows and destructs the underlying skeletal structures.
Cancer of mucous coat of alveolar edge of low and upper jaws
These new growths have almost always the structure of epidermoid cancer. They come out rather early because teeth become involved into the process, tooth ache appear. Treatment is often carried out when these aches appear, and a tooth can be even extracted. Improper tooth extraction caused the expansion of cancer growth into sockets and then into bone. At early stage a tumor is usually local one and bleeds when touching. The infiltration of underlying bone tissue (alveolar edge of low and upper jaw) occurs in several months and must be considered as late presentation of disease. The rate of tumor expansion in bone is determined by X-ray, but it should be taken into account that chronic diseases of teeth also cause presentation of demineralization of bone tissue. Depending on localization the gingival cancer spreads into the buccal mucosa, palate mucosa and oral cavity mucosa. Regional metastases occur early and are diagnosed in approximately one third of patients. Malignant tumors originating from minor salivary glands appear rarely.
Diagnostics
Clinical definition of epidermoid cancer of the oral cavity is based on peculiarities of this malignant tumor development (mentioned above) and does not cause any difficulties. It is necessary to determine the localization of tumor, its size, rate of expansion and clinical growth form. At present the rate of tumor expansion is determined visually and by touch.
Secondary affection of the facial skeleton by tumor is defined using X-ray method and scintigraphy. However in the infiltration of periosteum by tumor can not be determined by these methods so it must be considered as an affected zone. The aim of the morphological investigation is identification of tumor nature of biopsic material, histological structure of malignant growth, differentiation of epidermoid cancer, presence of tumor infiltration in surrounding tissues and vessels. All these features play an important role for prediction of disease progress and selection of treatment method. Cytological method plays an important role in differential diagnostics of minor tumors and precancer diseases.
As a rule, the diagnostics of regional metastases does not cause difficulties. In order to predict the disease progress and to select the most efficient treatment method it is necessary to estimate the amount of regional metastases and their localization in the corresponding groups of neck lymphatic nodes being defined by touch and using ultrasound scanning. Cytological investigation of punctates from metastatic node enables to make a correct diagnosis in 80 % of cases. Diagnostics of distant metastasis requires the examination of organs the most frequently affected by epidermoid cancer. The following examinations can be used: X-ray test, functional examination of liver (biochemical blood analysis, isotopic examination), ultrasound liver examination.
Treatment
Treatment of oral cancer can be divided into two stages: treatment of primary focus and treatment of regional metastases.
I stage – treatment of primary focus. In order to treat primary tumor the radiation, combined and surgical methods are used.
Radiation method. It is one of the most popular treatment methods for oral cancer. It is used for 88.7 % patients with tumors of oral cavity organs, and for 72.4 % – as an individual method. It is regarded as the main method of treatment at early stages of tumor development.
Gamma-ray teletherapy is used more frequently, intracavitary gamma teletherapy and their combination are used less frequently.
The results, according to native and foreign scientists are following: in case of primary cancer of the movable part of tongue corresponding to stages I and II (T1 and T2) the usage of different techniques of radiation therapy gave the possibility to cure 70–85 % and 38–56 % patients during 5 years respectively. In case of I stage of the oral cancer 53–66 % patients recover during 5 years, in case of II stage – 43–46 %, cheek cancer – 81 and 61 % respectively.
The results of radiation treatment of III stage cancer of the oral mucosa are worse – 16–25 %.
Combined method. At present the combined treatment of oral cancer is widely used, its main component is surgical operation. At the first stage of treatment the majority of specialists suggest gamma-ray teletherapy, at the second stage – operative treatment. The dosage of preoperative irradiation is 35–45 Gr. Favourable results of 5-year combined treatment for I and II stage cancer are comparable with results of radiation therapy along and reach 80–94 % and 39–65 % respectively. In cases of tumors of other localizations I and II stages 30–53 % patients with cancer of floor of the mouth recovered, 42,8 % patients with cancer of the mandibular alveolar bone and 94 and 65 % patients with cheek cancer respectively. In case of III stage disease the results of combined cancer treatment of any localization in the oral cavity make up 37 % recoveries during 5 years. This method is used as major one for treatment of locally advanced cancer. The main component is operation, its type depend on rate of primary tumor expansion, form of its development and its histological structure.
Surgical method
At present the half tongue electrocision is widely used in tongue surgery. This operation is conducted in case of I–II stage cancer as well as for the large tumors as a part of combined interventions (on 2 and more organs). Resection limits are not less than 2–4 cm of healthy tissues.
In case of locally advanced cancer of the movable part of the tongue and oral cavity bottom the combined half tongue electrocision is executed together with resection of oral cavity bottom (upon evidence – resection of the low jaw) with single-stage grafting of defects of tongue tissues and oral cavity bottom with musculocutaneous flaps.
II stage – influence on areas with regional metastases.
Regional metastases of cancer of the oral cavity of all localizations are observed in 23–40 %. The highest percentage of metastases in neck lymphatic nodes is identified in primary tumors with size 4 cm and more. In case of primary tumor 4 cm and more with morphologically confirmed metastases during 5 years only 17–20 % patients survive without recurrences and metastases. Regardless of the size of primary tumor with regional metastases 9–33 % patients survive, in their absence – 50–70 %. The most favourable treatment method of regional metastases is surgical method.
For this purpose fascial casing resection of neck dietary fibre and Crile operation are executed.
In order to avoid the development of regional metastases some radiologists use elective irradiation of areas of regional lymphatic outflow.
Dentists as well as doctors of any other specialization must demonstrate oncological suspicion when examining a patient. Regardless of the complaints that a patient has, the examination of the oral cavity and vermilion border is obligatory for a doctor. He must pay attention to any deviation from norm. Early evidences of cancer may not be evident for the patient but a doctor is obliged to reveal them as soon as possible. The term “oncological suspicion” means first of all particular oncological knowledge that enables a doctor to execute early and timely cancer diagnostics. This term also includes the knowledge of precancer diseases and their treatment, knowledge of organization of oncological assistance, chain of oncological treatment establishments, and immediate patient referral for treatment. In cases, that are difficult for diagnostics doctors should pay attention to possible growth of malignant tumor and make a diagnosis in as short period as possible. The treatment without proper diagnosis must not be conducted more than 7 days. It is required to remove local irritants, not to use means contributing to growth of tumor (burnings, physiotherapy etc.). In difficult cases a doctor must request assistance of more experienced specialists when examining a patient.
The treatment is conducted by oncologists. After cancer or precancer disease treatment patients must be at dispensary observation.
Malignant tumors of the jaws
Malignant tumors unlike benign neoplasms are more invasive, have a greater degree of anaptasia and have the ability to metastasize regionally to lymph nodes or distantly to other sites. Malignant tumors that arise de novo are termed primary tumors, and those that originate from distant tumors are termed secondary or methastatic.
Malignancies that commonly affect the jaws are carcinomas (lesions of epithelial origin), metastatic lesions from distant sites, sarcomas (lesions of mesenchymal origin), and malignancies of the hematopoietic system. Malignant tumors may occur at any age in either gender.
The following clinical signs are observed in malignant tumors: swelling, displaced teeth, loosened teeth over a short duration, foul smell, ulceration, presence of an indurated or rolled border, exposure of underlying bone, sensory or motor neural deficits, lymphadenopathy, weight loss, dysgeusia, dysphagia, dysphonia, hemorrhage, lack of normal healing, or pain with no demonstrable dental cause. Dentists must vigilantly watch for the possibility of malignancy in their patients. The risks of lack of attention to this possibility are delayed diagnosis, delayed treatment, increased need for aggressive treatment with added morbidity, and, in the worst case, premature death.
Diagnostic procedures in jaw malignences
The most informative imaging techniques in the head and neck are radiography and computerised tomography (CT), magnetic resonance imaging (MRI) and ultrasound.
Radiographic examination
Radiology has an important role in the management of the patient with cancer. First, diagnostic images may aid in the establishment of an initial diagnosis of a tumor. Diagnostic imaging also aids in the appropriate staging of disease from early small cancers to large cancers that have spread. Appropriate radiologic investigations assist the surgeon or radiation oncologist to determine the appropriate dimensions of the tumor so that it can be excised or irradiated adequately. Radiologic investigation has the potential to determine the presence of osseous involvement from soft tissue tumors and allow the practitioner to assess the presence of nodal disease and the outcome of treatment.
The following features may suggest the presence of a malignant tumor.
Location. Primary and metastatic malignant tumors may occur anywhere in the oral and maxillofacial region. Primary carcinomas are more commonly seen in the tongue, floor of the mouth, tonsillar area, lip, soft palate, or gingiva and may invade the jaws from any of these sites. Sarcomas are more common in the mandible and in posterior regions of both jaws. Metastatic tumors are most common in the posterior mandible and maxilla.
Periphery and shape
The typical appearance of the periphery of a malignant lesion is an ill-defined border with a lack of cortication and absence of encapsulation (a soft tissue or radiolucent periphery). This infiltrative border has uneven extensions of bone destruction. Fingerlike extension of the tumor occurs in many directions; this extension is followed by osseous destruction producing a region of radiolucency. Evidence of osseous destruction with adjacent soft tissue mass is highly suggestive of malignancy. Such a mass may exhibit a smooth or ulcerated peripheral border if cast against a radiolucent background. The shape of a malignant tumor of the jaw is irregular.
Because most malignancies do not produce bone nor do they stimulate the formation of reactive bone, the internal aspect is typically radiolucent in most instances. Occasionally residual islands of bone are present, resulting in a pattern of patchy destruction with some scattered residual internal osseous structure. Some tumors, such as prostate and breast metastatic lesions, can induce bone formation, resulting in an abnormal-appearing internal osseous architecture, whereas others, such as osteogenic sarcomas, can be productive in nature.
Effects on surrounding structures
Malignancy is destructive and often rapidly growing. The effect on surrounding structures mirrors this behavior. Rapidly growing malignant lesions generally destroy supporting alveolar bone so that teeth may appear to be floating in space.
Occasionally root resorption is present, this being more common in sarcomas. Internal trabecular bone is destroyed, as are cortical boundaries such as the sinus floor, inferior border of the mandible, follicular cortices, and the cortex of the inferior alveolar neurovascular canal. Because malignant tumors tend to grow rapidly, they invade by means of the easiest routes such as through the maxillary antrum or through the periodontal ligament space around teeth, resulting in, irregular widening with destruction of the lamina dura. Where the tumor has destroyed the outer cortex of bone, usually no periosteal reaction occurs; however, some tumors stimulate unusual periosteal new bone formation. Lesions such as osteosarcoma and prostate metastatic lesions as well as other tumors can stimulate the formation of thin straight spicules of bone, giving a sunburst appearance.
Plain radiography is widely available but the value of additional techniques should be understood. It is also advisable to request a formal radiologist’s report on radiographic films, whenever the radiographic features appear unusual or beyond the experience of the clinician.
Computerised tomography (CT)
CT is a cross-sectional radiologic imaging technique that is particularly useful in the evaluation of bone lesions. Not only can the density and margins of the lesion in question be evaluated with this technique but cortical expansion and fine internal details can often be more readily appreciated compared with plain film images. Use of contrast media has extended the utility of this technique in areas of soft tissue pathology. Furthermore, more recent designs such as spiral CT scanners have made data acquisition much more rapid and have reduced radiation dose to the patient while maintaining or improving resolution.
Magnetic resonance imaging (MRI)
MRI is a newer form of crosssectional imaging that does not expose patients to ionizing radiation. Although primarily used in the evaluation of soft tissue lesions, it is also capable of providing diagnostic information regarding bony lesions. Two distinct views are typically generated: T1 and T2.
Adipose tissue has the highest signal in the Tl-weighted image, and this view is often used for identifying anatomic structures. By comparison, the T2 image highlights tissues with high water content and is especially useful in depicting inflammatory processes and neoplasms.
Radionuclide imaging
Radionuclide imaging relies on the specific uptake of any one of several isotopes by various types of tissues or cells. Localization of the isotope is determined by examining the patient with a gamma scintillation camera.
The most commonly used isotope, Technetium-99m pertechnetate, can demonstrate areas of high metabolic activity. It is useful in identifying inflammatory conditions such as osteomyelitis, areas of active skeletal lesions of fibrous dysplasia or osteitis deformans, and metastatic disease.
PET (positron emissive tomography) scan
PET scan is the most recently developed cross-sectional imaging technology. This technique relies on the identification of metabolically active cells, such as metastatic deposits of squamous cell carcinoma, that exhibit preferential uptake of radionuclide-labeled glucose. In conjunction with CT/MRI, preoperative PET imaging of patients with head and neck cancer has lead to increased sensitivity and specificity for detection of oral cavity carcinoma, esophageal carcinoma, and clinically occult metastatic disease in the neck.
PET scans have proved particularly useful in the post-treatment follow-up by helping to distinguish altered anatomic landmarks or areas of fibrosis from recurrent tumor as well as the detection of distant metastases from head and neck primaries.
The technique is not recommended for neoplasms that are relatively inactive metabolically (eg, low-grade mucoepidermoid carcinoma). In addition, the lower limit of tumor mass detection by current technology is no better than that of CT/MRI, and false-positives owing to inflammatory changes are reported.
Osteosarcoma
Osteosarcoma is highly malignant neoplasm of bone in which osteoid is produced directly by malignant stroma. The three major histologic types are chondroblastic, osteoblastic, and fibroblastic osteosarcoma.
Osteosarcoma of the jaws is quite rare and accounts for approximately 7 % of all osteosarcomas. It is more common in young people under the age of 30 but can occur in older patients and a small number of people with Paget’s disease develop osteosarcoma as a rare complication. The age of presentation of the disease appears to be significantly older in the jaws than in other bones, and it may affect the maxilla or mandible. The most commonly reported symptom is rapidly growing swelling. Other signs are pain, movable teeth, and tenderness, erythema of overlying mucosa, ulceration, epistaxis, hemorrhage, nasal obstruction, exophthalmos, trismus, and blindness. Hypoesthesia is observed in cases involving neurovascular canals.
The mandible is more commonly affected than the maxilla. Although the lesion can occur in any part of either jaw, the posterior mandible, including the tooth-bearing area, angle, and vertical ramus, is most commonly affected. Osteosarcoma has an ill-defined border in most instances. When viewed against normal bone, the lesion is usually radiolucent with no peripheral sclerosis or encapsulation. If the lesion involves the periosteum directly or by extension, one may see the typical sunray spicules or trabeculae. Osteosarcoma maybe entirely radiolucent, mixed radiolucent-radiopaque, or quite radiopaque. The internal osseous structure may take the appearance of granular- or sclerotic-appearing bone, cotton balls, wisps, or honeycombed internal structures in areas with adjacent destruction of the preexisting osseous architecture. Whatever the resultant internal structure, the normal trabecular structure of the jaws is lost.
Effects on surrounding structures, widening of the periodontal membrane suggests osteosarcoma but is also seen in other malignancies. The antral or nasal wall cortices may be lost in maxillary lesions. Mandibular lesions may destroy the cortex of the mandibular canal and adjacent lamina dura.
If the internal structure is minimal or absent, fibrosarcoma or metastatic carcinoma may appear similar to osteosarcoma. If the osseous structure is visible, the practitioner should also consider chondrosarcoma. If spiculated periosteal new bone is present, prostate and breast metastases should be
considered. Comprehensive physical examination and laboratory tests assist in determining if the lesion is primary or metastatic. Benign tumors such as ossifying fibroma and benign conditions such as fibrous dysplasia may mimic osteosarcoma. The former conditions, however, are usually better demarcated and have a more uniform internal structine. Ewing’s sarcoma, solitary plasmacytoma, and even osteomyelitis share some of the radiographic characteristics of osteosarcoma.
Treatment and prognosis. The management of osteosarcoma is resection with a large border of adjacent normal bone. This may be possible in orthopedic cases but may be complicated by the presence of important adjacent anatomic structures in the head and neck. Generally radiation therapy and chemotherapy are used only for controlling metastatic spread or for palliation.
Carcinoma
Squamous cell carcinoma originatin in soft tissue
Squamous cell carcinoma, the most common oral malignancy, is a malignant tumor originating from the surface epithelium. It is characterized initially by invasion of malignant epithelial cells into the underlying connective tissue with subsequent spread into deeper soft tissues and occasionally into adjacent bone, local-regional lymph nodes, and ultimately to distant sites such as the lung, liver, and skeleton. Males are more commonly affected than females. Most squamous cell carcinomas occur in persons older than 50 years.
Squamous cell carcinoma appears initially as white or red (sometimes mixed) irregular patchy lesions of the affected epithelium. With time these lesions exhibit central ulceration; a rolled or indurated border, which represents invasion of malignant cells; and palpable infiltration into adjacent muscle or bone. Pain may be variable, and regional lymphadenopathy with hard lymph nodes that may or may not be tethered to underlying structures may be present. Other clinical features include a soft tissue mass, paresthesia, anesthesia, dyscsthesia, pain, foul smell, trismus, grossly loosened teeth, or hemorrhage. Large lesions can obstruct the airway, the opening of the eustachian tube (leading to diminished hearing), or the nasopharynx. Patients often report a significant weight loss and feel unwell. The condition is often fatal, if untreated.
Radiographically squamous cell carcinoma commonly involves the lateral border of the tongue. Therefore a common site to observe bone invasion is the posterior mandible. Lesions of the lip and floor of the mouth may invade the anterior mandible. Lesions involving attached gingiva and underlying alveolar bone may mimic inflammatory disease such as periodontal disease. Squamous cell carcinoma may erode into underlying bone from any direction, producing a radiolucency that is polymorphous and irregular in outline. Invasion occurs in one half of cases and is characterized most commonly by non-corticated border. Rarely the bolder may appear smooth, indicating underlying erosion rather than invasion. If bone involvement is extensive, the periphery appears to have fingerlike extensions preceding a zone of impressive osseous destruction. If pathologic fracture occurs, the borders show sharpened thinned bone ends with displacement of segments and an adjacent soft tissue mass. Surface carcinomas are capable of producing sclerosis in underlying osseous structures without frank invasion. The internal structure of squamous cell carcinoma in jaw lesions is totally radiolucent; the original osseous structure can be completely lost. Occasionally small islands of residual normal trabecular bone are visible within this central radiolucency.
Squamous cell carcinoma is discernible from other malignancies by its clinical and histologic features. Occasionally it is difficult to differentiate inflammatory lesions such as osteomyelitis from squamous cell carcinoma, especially when oral bacteria secondarily infect the tumor. Both osteomyelitis and squamous cell carcinoma are destructive, leaving islands of osseous structure that may appear to be consistent with sequestra. Evidence of profound bone destruction or invasive characteristics helps to identify the presence of a malignancy when a mixture of inflammatory changes and carcinoma exists. Osteomyelitis usually produces some periosteal reaction, whereas squamous cell carcinoma does not. In cases of osteoradionecrosis, the differentiation of this condition from squamous cell carcinoma requires advanced imaging or surgical exploration.
Treatment and prognosis. Oral squamous cell carcinoma is usually managed using a combination of surgery and radiation therapy. The choice of which modality to use depends on the location and severity of the tumor. Generally, if an adequate margin of normal tissue can be obtained, surgery is the usual treatment, followed by radiation treatment. Alternately, radiation may be used as the primary treatment followed by surgical intervention. Currently, the trend is to add concomitant chemotherapy as an adjunct to either radiation or surgical treatment.
Squamous cell carcinoma originating in bone
Squamous cell carcinomas that are encountered in the jaws, lack any continuity with the oral or antral mucosa, and occur in the absence of a primary carcinoma located elsewhere are termed primary intraosseous squamous cell carcinomas. These cases are assumed to arise from odontogenic epithelium.
They typically occur in elderly patients and tend to occur in the mandibular body region. Squamous cell carcinomas may also arise from the linings of odontogenic cysts. These neoplasms are rare and may remain silent until they have reached a fairly large size. Pain, pathologic fracture, and sensory nerve abnormalities such as lip paresthesia and lymphadenopathy may occur with this tumor. It is more common in men and in patients in their fourth to eighth decade of life. The surface epithelium is invariably normal in appearance.
The mandible is far more commonly involved than the maxilla, with most cases being present in the molar region and less frequently in the anterior aspect of the jaws. Because the lesion is by definition associated with remnants of the dental lamina, it originates only in tooth-bearing parts of the jaw. The periphery of the majority of lesions is ill-defined. They are most often rounded or irregular in shape and have a border that demonstrates osseous destruction and varying degrees of extension at the periphery. The degree of raggedness of the border may reflect the aggressiveness of the lesion. If sufficient in size, pathologic fracture occurs, with its associated step defects, thinned cortical borders, and subsequent soft tissue mass. The internal structure is wholly radiolucent with no evidence of bone production and very little residual bone left within the center of the lesion. If the lesion is small, overlying buccal or lingual plates may cast a shadow that may mimic the appearance of internal trabecular bone. These lesions are capable of causing destruction of the antral or nasal floors, loss of the cortical outline of the mandibular neurovascular canal, and effacement of the lamina dura. Root resorption is unusual. Teeth that lose both lamina dura and supporting bone appear to be floating in space.
Treatment and Prognosis.
Primary squamous cell carcinomas are excised with their surrounding osseous structure in an en bloc resection. Radiation and chemotherapy may be used as adjunctive therapies. The 5-year survival rate is 30 to 40 %.
Malignant odontogenic tumors
Malignant odontogenic tumors are very rare. They arise from the epithelial components of the odontogenic apparatus: the rests of Malassez, the reduced enamel epithelium surrounding the crown of an impacted tooth, the rests of Serres in the gingiva, and the linings of odontogenic cysts. In general, all of these tumors exhibit typical microscopic features of malignancy and have the potential for either regional nodal or distant metastases.
Malignant ameloblastoma AND Ameloblastic Carcinoma
Malignant ameloblastomas have the histologic features of benign ameloblastoma but with signs of metastatic dissemination. The most common sites of metastatic disease are the lungs, followed by the cervical lymph nodes and visceral organs. Ameloblastic carcinomas are malignant epithelial odontogenic tumors that exist in the background of benign ameloblastomas. Hystologically ameloblastic carcinomas represents the signs of malignant lesions with hyperchromatism, pleomorphism, and high mitotic activity. The tumour is variable in its aggressiveness and spreads by local destruction of bone. If untreated, it will eventually spread into soft tissues and this may make it very difficult to eradicate surgically. Gradual swelling of the jaw is the usual initial symptom of this tumour, although it may be diagnosed through a radiograph before this becomes apparent. Loosening and displacement of teeth can occur, as well as pain or altered sensation. Malignant ameloblastoma is rare and in early stages radiologicaly and clinically resembles to benign ameloblastoma. The correct diagnosis therefore demands histological verification.
Metastatic Tumors of the jaws
Metastatic tumors represent the establishment of new foci of malignant disease from a distant malignant tumor. Metastatic lesions of the jaws usu ally occur when the distant primary lesion is already known, although on occasion a jaw metastatic tumor may reveal the presence of a silent primary lesion. Jaw involvement accounts for less than 1 % of metastatic malignancies found elsewhere, with most affecting the spine, pelvis, skull, ribs, and humerus. Most frequently the tumor is a type of carcinoma, the most common primary sites being the breast, kidney, lung, colon and rectum, prostate, thyroid, stomach, melanoma, testes, bladder, ovary, and cervix. Metastatic carcinoma must be differentiated from the more common locally invading squamous carcinoma. Metastatic disease is more common in patients in their fifth to seventh decade of life. Patients may complain of dental pain, numbness or paresthesia of the third branch of the trigeminal nerve, pathologic fracture of the jaw, or hemorrhage from the tumor site. The posterior areas of the jaws are more commonly affected. The maxillary sinus may be the next most common site, followed by the anterior hard palate and mandibular condyle. Frequently metastalic lesions of the mandible are bilateral. Metastatic lesions may be moderately well demarcated but have no cortication or encapsulation at their tumor margins; they may also have ill-defined invasive margins. The lesions are not round but polymorphous in shape. Both prostate and breast lesions may stimulate bone formation of the adjacent bone, which will be sclerotic. The tumor may begin as a few zones of osseous destruction separated by normal bone. After a time these small areas coalesce into a larger, ill-defined mass and the jaw may become enlarged. Lesions are generally radiolucent, in which case the internal structure is a combination of residual normal trabecular bone in association with areas of bone lysis. If the tumor is seeded in multiple regions of the jaw, the result is a multifoeal appearance (multiple small radiolucent lesions). In most cases a known primary malignancy is present, and the diagnosis of metastasis is straightforward. Multiple myeloma may be confused with metastatic tumors; however, the border of multiple myeloma is usually better circumscribed than in metastatic disease. When a lesion starts within the periodontal ligament space of a tooth, the appearance may be identical to that of a periapical inflammatory lesion. Odontogenic cysts, if secondarily infected, may have an ill-defined border giving a similar appearance to a metastatic lesion.
Treatment and Prognosis
The presence of a metastatic tumor in the jaw indicates a poor prognosis. If metastatic disease is present, the patient will usually die within 1 to 2 years. If the radiographic appearance is suspicious, an opinion from a dental radiologist should be sought and tissue submitted for histologic analysis. Nuclear medicine may be employed to detect other metastatic lesions. Isolated malignant deposits, if symptomatic, may be treated with localized high-dose radiation treatment. In the rare occasion that the jaw is the first diagnosed site of malignant spread, it is imperative that the patient be referred quickly to an oncologist so that anticancer treatment can be delivered promptly. This treatment may take the form of chemotherapy, radiation therapy, surgery, immunotherapy, and hormone treatment.
Multiple myeloma
Multiple myeloma is a malignant neoplasm of plasma cells. It is the most common malignancy of bone in adults. Single lesions are called plasmacytoma, and multiple lesions arc termed multiple myeloma.
Multiple myeloma is a fatal systemic malignancy. A patient with multiple myeloma is usually lacks any sign of bone reaction. The lesions have been described as appearing “punched out”. However, many appear ragged and even infiltrative. Some lesions have an oval or cystic shape. Untreated or aggressive areas of destruction may become confluent, giving the appearance of multilocularity. If the lesion is located in the periapical periodontal ligament space, it may have a border similar to that seen in inflammatory or infectious periapical disease. Soft tissue lesions have been reported in the jaws and nasopharynx. When visible on radiographs, they appear as smooth – bordered soft tissue masses, possibly with underlying bone destruction.
No internal structure is radiographically visible. Occasionally islands of residual bone, yet unaffected by tumor, give the appearance of the presence of new trabecular bone within the mass. Very rarely the lesions appear radiopaque internally.
Differential diagnosis
The most likely disease to be mistaken for multiple myeloma is the radiolucent form of metastatic carcinoma. Knowledge of a prior malignancy in a patient may help differentiate multiple myeloma from metastatic carcinoma. Osteomyelitis, if severe, may yield a radiologic picture similar to that of multiple myeloma; however, a visible cause for it usually exists. In addition, inflammatory lesions and infections in general cause sclerosis in adjacent bone, which multiple myeloma does not. Simple bone cysts may be bilateral in the mandible and therefore may be mistaken for multiple myeloma. They are usually corticated in part and characteristically interdigitate between the roots of the teeth in a much younger population. Generalized radiolucency of the jaws may be caused by hyperparathyroidism but is differentiated based on abnormal blood chemistry.
Management
The management of multiple myeloma is usually chemotherapeutic with or without autologous or allogeneic bone marrow transplantation. Radiation therapy may be used for treatment of symptomatic osseous lesions when palliation is required.
Surgical management of the jaw cancer
Maxillectomy
The maxilla can be resected by three distinct methods. These include a direct standard approach through an extended lateral rhinotomy incision, a lateral approach, and a transoral transpalatal facial degloving approach. The first (Weber – Ferguson) is the most common approach and utilizes a lateral rhinotomy incision with a limb of the incision extended inferior to the lower lid and then two centimeters beyond the lateral canthus of the eye. Making the incision three millimeters below the tarsal plate prevents postoperative epiphora. By rounding the incision near the medial canthus a persistent nasal cutaneous fistula is avoided. An upward extension in the medial canthal region is made if a maxilloethmoidectomy will be required.
The soft tissue flap is elevated allowing muscle attachment to remain to the maxilla, especially if a previous Caldwell – Luc has been performed. The orbital periosteum is then elevated and the orbital floor inspected for invasion by malignancy. If none is found the infraorbital fissure serves as the lateral margin of resection.
Lateral bony resection can occur through the malar eminence utilizing an oscillating saw. Another approach is to use a Gigli saw, separating the frontal maxillary process. A second osteotomy is then required through the zygoma. The decision on placement of this incision is based on the lateral extent of the tumor. Preserving the malar eminence allows a better cosmetic appearance.
Medially, the plane of the resection has been determined by the preoperative assessment of the extent of ethmoid involvement. When a combined craniofacial approach is not planned this osteotomy is made by a chisel approximately one centimeter below the frontal ethmoid suture. A chisel is used to continue the lateral rhinotomy incision through the nasal bone, and if necessary the entire nasal bone and skin complex can be swung to the contralateral side.
Preoperative assessment of the intranasal extent of tumor determines whether the incision is made on the ipsilateral or contralateral side of the septum. The hard palate incision is made close to the midline on the ipsilateral side when there is no evidence of tumor extension into the hard palate. The soft palate is preserved and remains attached. When posterior tumor extension toward the nasopharynx necessitates excision of a portion of the soft palate, the remaining palate should be re-approximated to any remaining buttress of bone or soft tissue in this area to avoid problems in swallowing and speaking.
The hard palate incision can be modified to allow for preservation of the premaxilla, thereby retaining the medial and lateral incisors. It is seldom possible to retain the canine tooth without compromising the resection. Preserving this small segment of premaxilla allows the prosthodontist to make an obturator which stays in position more easily.
By extending the skin incision laterally, and separating the coronoid process with the attached temporalis muscle from the ascending ramus of the mandible, it is possible to preserve a temporalis muscle flap for reconstructing the orbital floor. Because the coronoid bone remains attached to the temporalis muscle, it allows more secure placement of sutures into the muscle as it is pulled to the remaining ethmoid area, septum, or contralateral nose. Without this small portion of bone, sutures tend to tear through the temporalis muscle.
This lateral approach allows inspection of the pterygopalatine space and permits chisel placement under direct vision when separating the pterygoid plates from the skull base. Final chisel placement is determined by whether the posterior wall of the maxilla or pterygoid plates appear intact.
Complete separation of the specimen requires excising remaining soft tissue attachments and rocking the specimen so that the posterior orbital floor fractures between the inferior orbital fissure and the incision made in the ethmoids. Tumors confined to the maxilla or with early maxilloethmoid extension are removed en bloc by this method and rarely should there be positive margins.
The pathologist comes to the operating room to evaluate the surgical specimen. We have found that even then it is still difficult to evaluate the adequacy of margins. Thus a new set of margins is taken directly from the patient from the following areas: the remaining hard palate, ethmoid and posterior ethmoid, the base of the skull near the foramen ovale, the base of the skull and adjacent mucosal lining of the nasopharynx, and the nasal vault. Frozen sections are obtained and further resection is performed if required. It has been noted by other authors that if any of this tissue is unexpectedly found to be positive the prognosis is poor even though further resection is immediately performed.
A second approach is used for large tumors with lateral or posterior extension. This begins with a more limited lateral rhinotomy incision without extension of the infraorbital incision beyond the lateral canthus of the eye. A second skin incision is made down through the chin and then directly laterally. A midline stepped mandibulotomy is performed after drill holes are placed for reapproximation. In young patients with excellent dentition it is possible to split the mandible in the midline without a dental extraction. If dental viability is in question one of the incisors should be extracted. The mandible is swung laterally and the lingual nerve, hypoglossal nerve, and submandibular duct preserved. The soft tissues of the floor of the mouth are dissected laterally and the tongue medially. If required, a temporalis muscle coronoid process flap can also be preserved in this lateral approach.
Tumors with infratemporal fossa extension particularly require this approach. The lateral approach is also required when there is definite invasion of the pterygoid plates or when resection is planned for tumors which extend primarily into the pterygomaxillary or pterygopalatine fossa. The approach can also be used for select tumors with limited extension onto the lateral wall of the nasopharynx anterior to the region of the eustachian tube.
Main advantages of this approach are control of the blood supply to these regions and direct visualization of this area early, as opposed to the direct anterior approach where the full extent of the tumor is not appreciated until late in the procedure. Ligation of the internal maxillary artery can be performed through this lateral approach. Tracheotomy is necessary. This method is preferred to the lateral mandibulotomy approach to the infratemporal fossa, as it provides nearly equal visualization and has less associated morbidity. The midline mandibulotomy is repaired with Wurtzburg or Luer miniplates. The temporary maxillary prosthesis is placed in the patient, who is permitted to eat after a few days, when the swelling of the soft palate and pharynx has resolved.
A third approach, which involves a degloving of the central face, is used for more limited tumors of the inferior maxilla. Tumors ideally suited for this type of resection include those of the nasal septum, inverting papillomas, and tumors of low grade malignancy, particularly when located medially. The obvious advantage is that no skin incision is required. Combined craniofacial resections have been performed for some tumors using this approach.
Combined craniofacial resection is used when there is extension into the superior ethmoid and cribriform plate area. Tumors which arise primarily in the ethmoid or nasal vault area will develop early extension through the cribriform plate. Cribriform plate involvement is difficult to ascertain by either CT scan or polytomography, and impossible to ascertain by a routine sinus X-ray. The MRI scan is valuable in determining the extent of tumor to this area.
In most cases, better survival rates are reported when orbital exoneration is included as part of this procedure. The extension into the orbit is usually from the posterior ethmoid area and can be appreciated on the CT scan. Preservation of orbital contents when this occurs is occasionally possible, but the prognosis is poor because of recurrence with extension into the middle cranial fossa.
Prior to surgery a lumbar subarachnoid drain is placed and 50 to 75 cubic centimeters of cerebrospinal fluid is removed. A Foley urethral catheter is inserted, especially if mannitol may be necessary. The neurosurgical approach begins with a standard frontal craniotomy with a free bone flap and preservation of the galea or periosteum for the reconstructive procedure. The dura is inspected for invasion. If extension of the tumor through the dura into the frontal lobe is found the procedure is terminated at this point. The posterior walls of the frontal sinuses are identified and removed, as well as all frontal mucosa, and the contralateral frontal duct is plugged with muscle. Dural extensions into the cribriform plate area are elevated and tearing of the dura can be expected in this region as well as over the fovea ethmoidalis. These tears are later repaired by either primary suturing or using fascia lata or temporalis fascia.
Once established that the tumor is resectable, the head and neck surgeon commences his portion of the operative procedure. A lateral rhinotomy incision is made and the Weber – Ferguson extension of this incision made if needed. If there is known tumor extension into the orbit an orbital exoneration will be required. This simplifies the en bloc procedure. Should the tumor extend across the midline, the superior portion of the nasal septum and the cribriform plate on both sides and the extension into the opposite ethmoid cells can be included.
Together, the neurosurgeon and head and neck surgeon outline the area for the cranial fossa floor incisions. A small mastoid burr is useful for outlining these incisions; they are completed using a chisel. Incisions can extend back as far as the anterior wall of the sphenoid sinus. Additional traction on the brain at this point is usually difficult and may compromise the optic nerves. The incision on the contralateral side is placed to avoid entering the preserved orbit. Maxilloethmoidectomy is now completed from below in the standard manner.
The previously created galeal flap is now sutured to the remaining lateral and posterior dura. Only in cases of very large defects is cartilage or iliac crest bone interposed between the galeal flap and a split thickness skin graft placed from below. Generally the galeal periosteal flap is sufficient, but a temporalis muscle flap can also be swung to close this defect when orbital exoneration has been performed. Every effort is made to avoid placing artificial or nonvascularized material in this region to close the defect. The frontal bone is replaced and maintained by wire sutures. A split thickness skin graft is placed from below and packed into position with one inch iodoform gauze soaked heavily in an antibiotic ointment. It is further held in position by the previously made palatal splint. The remaining portion of the wound closure is similar to a standard maxillectomy.
This procedure is particularly effective for patients with tumors confined to the ethmoid or nasal vault superior to the region of the middle turbinate. By mobilizing the nasal bones to the contralateral side in resecting the medial portion of the maxilla, orbital floor, and orbital exoneration, the anterior portion of the posterior ethmoids can be removed en bloc.
Fortunately, much of what appears to be tumor in the posterior ethmoids and sphenoid sinus by CT scan turns out to be chronic hyperplastic sinus mucosa without tumor extension. If there is obvious invasion and involvement of the sphenoid sinus, adequate tumor resection is seldom feasible.
Mandible resection and reconstruction in mandibular cancer
When tumor approaches or only superficially involves the mandible, a marginal resection may be carried out. The resection can be beveled so that the mucosal reflections of both the cheek and the floor of mouth are included, while the inferior alveolar nerve is spared. No bony reconstruction would be required in such a case.
More deeply invasive tumors may be treated with a more radical marginal resection, leaving only a strut of the lower or posterior border to maintain the continuity of the mandible. In such a resection, the entire inferior alveolar nerve may be removed. If the remaining strut of bone is thin, a bone graft may be needed to prevent pathologic fracture. This is technically far simpler than grafting a discontinuity defect.
When mandibulectomy is necessary, the remaining mandibular fragments are subject to displacement into the area of discontinuity by scar contracture and by the unopposed pull of the muscles of mastication. Appropriate management of these fragments will prevent much of the disability that results from such surgery and will facilitate later reconstruction.
In lateral mandibulectomy, it is usually possible to retain a portion of the ascending ramus, including the condyle. The posterior line of resection should be oriented vertically, from sigmoid notch to angle, rather than horizontally across the ramus in these cases. When the mandible is divided horizontally, the insertion of the temporalis muscle is retained. The unopposed pull of this muscle displaces the fragment superomedially beneath the zygomatic arch. This makes it technically difficult to retrieve later during reconstruction. When the mandible is divided vertically, the fragment remains almost in its natural anatomic position.
Immediate reconstruction of the resected oral mucous membranes with a soft tissue flap helps to maintain the separation of the mandibular fragments, prevents scar contracture, and replaces much of bulk that is lost when the mandible is removed.
In many cases, some form of internal, external, or dental fixation is very helpful in stabilizing the residual mandibular fragments. This is especially true in patients who retain a complement of useful teeth, which would otherwise be drawn out of occlusion. Internal fixation ranges from simple Kirschner wires or braided stainless steel wire to more elaborate bone plates. These should be used only as temporary spacers, as they will often loosen or fracture over time. External fixation consists of two bone screws in each fragment that are connected either by universal joints and connecting rods or by a bar of self-curing methyl methacrylate. Such devices are surprisingly trouble-free and can be maintained for years if necessary. The fact that they may be placed prior to the resection, and that they do not interfere with pedicle flaps, makes them extremely useful in certain cases. Dental fixation can range from simply wiring the remaining teeth together to utilizing appliances with flanges and guidance ramps to help prevent deviation of the remaining fragments.
The deformities and dysfunction that traditionally have been associated with oral cancer surgery result more from the resection of large areas of the mucous membrane than from mandibular resection. The problem is compounded by the practice of closing the surgical defect by drawing its edges together, thus approximating structures (for example, midline of the tongue and buccal mucosa) that are normally quite separate from one another. When bony reconstruction is to be carried out, adequate soft tissue lining and coverage are a necessary prerequisite. Satisfactory soft tissue reconstruction alone will, in many instances, provide patients with a very acceptable functional and cosmetic result after a major head and neck resection.
Numerous random flaps of oral mucosa, neck skin, and shoulder skin may be used to reconstruct surgical defects resulting from oral cancer resection. These flaps are thin. The blood supply may be unreliable, especially in irradiated patients. Multiple stages may be needed for their safe construction, transfer, and insetting. While these flaps largely have been replaced in practice by more versatile, reliable techniques, they retain their usefulness in certain individual situations.
Mucosal flaps have the advantage of providing the same sort of tissue as that which was resected. Their major drawback is the limited quantity of tissue available. Tongue and buccal mucosa are the most common donor sites. Tongue flaps are by far the most versatile mucosal flaps. Their excellent blood supply allows them to be elevated from the dorsal, ventral, or lateral surfaces. They may be based either anteriorly or posteriorly to reach small defects anywhere in the oral cavity. Their major drawback is the speech impediment that results from the use of moderately large-sized flaps.
Neck flaps are usually oriented vertically, with the base along the lower border of the mandible. If possible, platysma is included on the deep surface to increase the blood supply. The donor site may be closed primarily. The flap is turned under to provide oral lining. This leaves a controlled fistula, which is closed after three weeks when the base of the flap is divided.
Shoulder flaps are based on the nape of the neck. They have a limited arc of rotation, including the lateral face, neck, and posterior oral cavity. They should be delayed if extended beyond the mid-clavicle. The donor site cannot be closed, and requires a split-thickness skin graft.
Skin flaps that have a reliable vascular supply extending along their axis may be safely constructed with a large length-to-base ratio and thus have a wide arc of rotation. Such axial pattern flaps have found wide use in oral cancer reconstruction for many years. They generally lie well away from fields of radiation, are thin, well-vascularized, and versatile. Their major disadvantages are that a secondary procedure is usually required to divide the vascular pedicle, and that the donor site defect may be esthetically unpleasant. While they are no longer used as frequently as are newer techniques, they remain quite useful in certain specific clinical situations.
Recent advances in our understanding of the vascular anatomy of muscles have led to the development of techniques whereby a muscle may be detached from its origin and/or insertion and transferred into a defect. Since a significant part of the vascular supply of the skin overlying a muscle is derived from muscular perforators, composite flaps of muscle and skin may be transferred in a similar fashion. Such flaps have revolutionized soft tissue reconstruction of the head and neck because of their reliability and versatility. The muscle provides a highly vascular bulk of tissue to fill a defect. If skin is transferred as well, the entire surface overlying the muscle may be raised, or merely an island of skin, precisely tailored to fit a defect, may be safely used.
The transfer of tissue by microvascular anastomosis has achieved increasing success and popularity in recent years. Free flaps were initially directly derived from known axial pattern flaps. The newer free flaps have utilized larger vascular pedicles for more reliable anastomoses. The advantages of free flaps are that thin, pliable, nonirradiated tissues may be transferred in a single stage. The disadvantages include vastly increased operating time, potential donor site morbidity (especially for lower extremity or intra-abdominal donor sites), the need for specialized instrumentation, the requirement for personnel experienced in micro vascular surgery, and the fact that problems generally result in necrosis of the entire flap, whereas problems with pedicle flaps generally result in necrosis of superficial or distal portions of the flap.
In all cases of the mandibular resections osseous reconstruction of the mandible remains necessary for optimal functional and esthetic restoration of the face and the occlusion. A variety of implants, ranging from braided steel wires or mesh to metal plates and screws, to plastic or metalloplastic composites have been used to restore mandibular continuity. The advantage of these devices is that they do not require further surgery for a donor site. Their disadvantages are the possibility of soft tissue dehiscence, of fatigue and fracture of the implant, of loosening, and of pathologic fracture of the site of attachment to the host bone. Such devices are best used as temporary spacers prior to definitive osseous reconstruction. They may also be used in cases where medical considerations limit the length of the surgical procedure. Perhaps the best long-term results have been obtained with properly contoured plates and tapped, bicortical bone screws.
Bone derived from the patient himself is the preferred material for osseous reconstruction. In the process of autogeneic bone grafting, the graft assumes both an active and a passive role. Some cells with osteogenic potential survive the procedure and act with cells from the recipient site to produce new bone. The remainder of the bone dies, but acts as a template which is eventually resorbed and replaced by viable new bone.
Cortical bone grafts are resorbed and revascularized very slowly. Only a few surface cells survive the surgery, and there are few open spaces through which tissues of the recipient site may enter the graft. Large interior areas of these grafts may remain nonviable for years, making them subject to stress fracture, irregular remodeling, and clinical failure. Solid cortical grafts of rib or iliac crest are best avoided.
Cortico-cancellous bone grafts are split in such a way that one surface contains a mechanically sound cortical plate, while the opposite surface contains cancellous bone that presents a large surface area which favors survival of osteogenic cells, rapid revascularization, and remodeling. Corticocancellous grafts can be placed with the usual techniques used for fracture fixation; however, they may be stabilized most conveniently with bone plates that obviate the need for intermaxillary fixation. Split ribs, partialthickness blocks of ileum, and inner table strips of calvarium make excellent cortico-cancellous bone grafts.
Cancellous bone grafts present a very large surface area which is rapidly revascularized from the recipient site. Grafted marrow contains many cells with osteogenic potential that survive the surgery. Thus the individual spicules of grafted bone are rapidly resorbed and replaced with viable new bone. Unfortunately, the spicules of grafted bone seek a dependent position in a large mandibulectomy wound. For this reason, they have been used most frequently in conjunction with a prosthetic trough that assumes the shape of the mandible. The trough is firmly affixed to the ends of the defect, and then packed with cancellous bone.
Composite flaps containing bone, either transferred on a vascular pedicle or transferred via microvascular anastomosis, generally present more risks than benefits. Contouring of the bone is not safely possible, and so they are appropriate to reconstruct only relatively short, straight segments of mandible. The blood supply to the bony segment is primarily periosteal, permitting little stripping for the purposes of fixation. Despite survival of periosteal blood vessels, portions of the bone undergo avascular necrosis and require slow remodeling and replacement. Donor site morbidity can be high. Despite the attractiveness of performing the entire reconstruction at a single operative session, superior results can still be reliably obtained by bringing in healthy soft tissues at an initial surgery followed by a bone graft at a second stage.
Successful reconstruction of the hard and soft tissues following oral cancer resection frequently leaves the patient with residual defects of both form and function. A number of secondary surgical procedures can be considered for those patients who desire further improvement.
In terms of the extraoral tissue, procedures such as defatting of flaps, revision of scars, nerve grafts, or muscle transfers to reanimate portions of the face, and many others are useful.
Intraorally, there may be a number of problems. If there are remaining teeth, but they are not in perfect occlusion, specialized dental prostheses may greatly improve function. Bone grafts are rarely covered by tight, immobile tissues, and are thus unable to support dental prostheses. Such grafts require ridge extension procedures, such as skin grafts, to enable dentures to be fitted. Often portions of the tongue, floor of mouth, cheeks, and alveolar ridge are reconstructed using insensate flaps or grafts. This renders the patient only minimally capable of supporting and functioning with a denture. Such patients, after several surgeries, may be able to wear dentures only for cosmetic purposes. One solution to this problem is the placement of osseointegrated implants to help stabilize the denture.
Chapter 15. Maxillofacial trauma
General characteristics, clinical peculiarities, diagnostics and treatment of soft tissue injuries
Types of injuries
Abrasions
Abrasions are a type of injury caused by shear forces that remove a superficial layer of the skin. These superficial injuries usually heal without scarring. It is important to determine whether foreign bodies which have been embedded in the wound can cause permanent “tattooing” of the soft tissue. Treatment consists in wound cleaning and covering with a thin layer of topical antibiotic ointment to minimize desiccation and secondary crusting of the wound. Reepithelialization as usual is complete in 7 to 10 days if the epidermal pegs have not been completely removed. If the laceration significantly extends into the reticular dermal layer, significant scarring is likely.
Contusions
Contusions are caused by blunt trauma that causes edema and hematoma formation in the subcutaneous tissues. The associated soft tissue swelling and ecchymosis can be extensive. Small hematomas usually resolve without treatment; hypopigmentation or hyperpigmentation of the involved tissue can occur, but is rarely permanent. Large hematomas should be drained to prevent permanent pigmentary changes and secondary subcutaneous atrophy. In case of infection formed abscess has to be drained and treated in a usual way.
Wounds
Wound is a type of injury when consistency of the skin or mucosa is impaired (cut, stabbed, lacerated).
Classification and clinical picture according to injure pattern and traumatizing object:
- Cut wound
A sharp object causes these wounds. The surrounding tissues damage is not substantial. But the sharp object can go through covering tissues and affect internal organs and tissues. Damage of blood vessels and nerve trunks can lead to faint pain syndrome and massive bleeding.
- Stab wound
Stab wound is caused by sharp pointed object and has the large depth and small area of the injured skin and mucosa.
The pain syndrome is slight, hiatus is absent, the external bleeding is absent, but hematoma can develop.
- Contused wound
These wound caused with a blunt object. Before the skin rupture, the blunt object damages the deeper soft tissues or organs (muscles, bones).
A wide zone of smashed tissues around wound is peculiar. Contused wound causes pain syndrome, but there is no obvious external bleeding and can be infected easily. According to these complications contused woundsmore often heal by secondary tension.
- Lacerated wound (Fig. 15.1)
A blunt object causes these wounds but this object is directed under the acute angle to the skin. We can observe a big separation and sometimes to scalp of the skin. According to this separation skin can necrotize. Sometimes this kind of wounds can be caused by fractured parts of bones.

Fig. 15.1. Lacerated wound
- Crushed wound
The mechanism of this damage is equal to contused and lacerated wounds, but the degree of injury is maximal. Crushed wounds can be infected heal worse.
- Slash wound
Slash wound caused by big and sharp object (like axe, saber). It has signs of incised and contused wound simultaneously. In this type of injury the internal organs and bones can be damaged very often. Necrosis of affected tissues can be observed. Pain syndrome is very strong. Bleeding not severe, but massive diapedesis hemorrhages are present.
- Bite wound
Injury caused by animal or human bite. Bite wounds can be primarily infected with special infection. So, thorough wound irrigation and debridement are important in reducing infection and further complications.Animal and human bites are most often polymicrobial, containing aerobicand anaerobic organisms.
- Mixed wound
These wounds may connect two and more kinds of wounds.
Principles of management
The initial examination involves evaluating and stabilizing the trauma patient. Any life-threatening conditions should be identified and managed immediately. The conditions of the airway, breathing, and circulation are еxamined, followed by a general neurologic assessment with particular attention to cervical spine and cranial injuries. Radiographs are used to diagnose fractures of the face, because, facial fractures are ideally treated prior to soft tissue repair. If repair of the facial bones is delayed, it is optimal to close the lacerations initially (Fig. 15.2). The wounds can be reentered and revised if needed to access the fracture site.

Fig. 15.2. Management of the lacerated wound (chain saw):
a, b – before treatment,
c – after wound closure and suturing,
d – a week postoperative
It is important to achieve hemostasis when stabilizing and evaluating the patient who has sustained trauma. Most bleeding will respond to application of apressure dressing. Occasionally surgical exploration and packing of the wound under general anesthesia may be indicated. In rare instances vessels in the neck may need to be ligated. Indiscriminate clamping inside the wound should be avoided because damage to important structures such as the facial nerve or parotid duct may result. It is unusual for bleeding from soft tissue injuries to the face to result in a shock state.
Lacerations involving the scalp can occasionally be difficult to control with pressure and may require clamping, ligation, or electrocautery. In soft tissue injuries not involving the face the length of time from initial injury to treatment is important. Secondary risk of infection increases with the lapse of time. Because of the rich vascularity of the face there is no “golden period” for suture repair of facial wounds. In fact healing of facial wounds is unaffected by the interval between injury and repair. Patients who are immunized and have received a booster injection within the last 10 years do not require tetanus prophylaxis if the wound is not tetanus prone. Tetanus-prone wounds are those with heavy contamination from soil or manure, devitalized tissue, or deep puncture wounds. If the wound is tetanus prone and the patient has not received a booster injection within 5 years prior to the injury, a 0.5 Ml tetanus toxoid boost injection should be given. If the patient has not received a booster within 10 years prior, they should receive a booster injection for any wound. Patients who are not immunized should receive both a booster injection and 250 units of tetanus immunoglobulin, followed by a full course of immunization.Treatment of soft tissue injuries involves early reconstructive procedures addressing both the soft tissue and the underlying bony injury in a minimum number of stages 6, 7. Occasionally it is better to delay soft tissue repair until the facial fractures have been addressed. In patients with large avulsion of tissue, definitive early reconstruction of the tissue loss with regional or microvascular flaps may be required. After adequate anesthesia has been obtained, the wound is thoroughly debrided. Nonvital tissue is conservatively excised in an attempt to salvage most ofthe tissue. Devitalized tissue potentiates infection, which inhibits phagocytosis. Repair of facial soft.
Tissue injuries can be performed under local anesthetic with dosage 0.5 To 2 %. It is usually administered with epinephrine 1:100,000. Lidocaine has a rapid onset of action, a wide margin of safety, and a low incidence of allergic sensitivity. One should avoid injecting directly into the wound when important landmarks could be dislocated and distorted. Regional nerve blocks are beneficial in minimizingthe amount of local anesthesia required and also prevent distortion of the tissues. Proper cleaning and good surgical technique are imperative in minimizing infection. Infections are rare when wound is closed so that no dead space, devitalized tissue, or foreign bodies remain beneath the sutured skin. Hydrogen peroxideis minimally bactericidal and toxic tofibroblasts even when diluted to 1:100. Diluted hydrogen peroxide is useful in the postoperative period in cleaning crusts away from incision lines in order to minimizes carring. Common methods for closing wounds include suturing, applying adhesives, and stapling. It is preferable to suture complex facial lacerations secondary to esthetic considerations. A layered closure is almost always necessary and eliminates dead space beneath the wound. If the deadspace is not obliterated, accumulation of inflammatory exudates may occur. This leads to infection, which in turn may cause tension across the epidermis. Tension can cause necrosis of the skin edges due to impairment of the vascular supply and may cause an increase in scarring. Injuries involving anatomic borders such as the vermilion of the lip must be reapproximated precisely. Examples of these landmarks include eyebrows, lipmargins, and eyelids. Lacerations should be closed by placing a suture in the centerof the laceration to avoid creating excessive tissue on the end of the laceration (dog-ear). Deep layers should be reapproximated with 3–0 or 4–0 buried resorbable sutures. The superficial skin isclosed with 5–0 or 6–0 suture. It is important to avoid causing puncture marks when grasping the wound edges. Margins should be undermined to allow slighteversion of the wound margin. Skin sutures should be removed 4 to 6 days after placement. Delayed primary closure may be necessary in some instances. Patients who may benefit from a delayed procedure include those with extensive facial edema, a subcutaneous hematoma, or those with woundsthat are severely contused and contain devitalized tissue. Secondary revision procedures are usually undertaken months later to allow for scar maturation.
Mandibular fractures. Etiology, pathogenesis, diagnostics and treatment. Complications of the mandibular fractures
Epidemiology
Mandibular fractures and dentoalveolar injuries are most commonly (80 %) the result of motor vehicle accidents, interpersonal violence and assault, other causes are sporting and industrial accidents, or falls. Most fractures occur in the mandibular body, angle, or condyle regions, with lower percentages in the mandibular ramus, coronoid and symphysis regions. The literature demonstrates that many patients with mandible fractures have more than one fracture location. This may be due to a number of variables such as direction and force of the blow, mechanism of injury, teeth present or not, among others.
Classification
The first step in the development of an appropriate treatment plan is to establish a clear understanding of the type of injury the patient has suffered, in order to provide an adequate surgical solution. A number of classification schemes have been presented to describe mandible fractures. Mandibular fractures are classified according to various parameters. The most useful is classification by the pattern of fracture present and by anatomic location.
Anatomic location (Fig. 15.3):
- Dentoalveolar fracture: any fracture that is limited to the tooth-bearing area of the mandible without disruption of continuity of the underlying osseous structure.
- Symphysis fracture: any fracture in the region of the incisors that runs from the alveolar process through the inferior border of the mandible in a vertical or almost vertical direction.
- Parasymphysis fracture: a fracture that occurs between the mental foramen and the distal aspect of the lateral mandibular incisor extending from the alveolar process through the inferior border.
- Body fracture: any fracture that occurs in the region between the mental foramen and the distal portion of the second molar and extends from the alveolar process through the inferior border.
- Angle fracture: any fracture distal to the second molar, extending from any point on the curve formed by the junction of the body and ramus in the retromolar area to any point on the curve formed by the inferior border of the body and posterior border of the ramus of the mandible.
- Ascending ramus fracture: a fracture in which the fracture line extends horizontally through both the anterior and posterior borders of the ramus or that runs vertically from the sigmoid notch to the inferior border of the mandible.
- Condylar process fracture: a fracture that runs from the sigmoid notch to the posterior border of the ramus of the mandible along the superior.
- Aspect of the ramus; fractures involving the condylar area can be classified as extracapsular or intracapsular, depending on the relation of the fracture to the capsular attachment.

Fig. 15.3. Percentage of mandible fracture site distribution. by V. A. Malanchuk, M. A. Gordijchuk, 2010
Pattern of fracture:
- Simple fracture: a simple fracture consists of a single fracture line that does not communicate with the exterior. Inmandibular fractures this implies a fracture of the ramus or condyle or afracture in an edentulous portion with no tears in the periosteum.
- Compound fracture: these fractures have a communication with the external environment, usually by the periodontal ligament of a tooth, and involve all fractures of the tooth-bearing portions of the jaws. In addition, if there is a breach of the mucosa leading to an intraoral communication or a laceration of the skin communicating with the fracturesite, edentulous portions of the mandible may be involved.
- Greenstick fracture: this type of fracture frequently occurs in children and involves incomplete loss of continuity of the bone. Usually one cortex is fractured and the other is bent, leading to distortion without complete section. There is no mobility between the proximal and distal fragments.
- Comminuted fractures: these are fractures that exhibit multiple fragmentation of the bone at one fracture site. These are usually the result of greater forces than would normally be encountered in simple fractures.
- Complex or complicated fracture: this type of injury implies damage to structures adjacent to the bone such as major vessels, nerves, or joint structures. This usually implies damage to the inferioralveolar artery, vein, and nerve in mandibular fractures proximal to the mental foramen and distal to the mandibular foramen. On rare occasions a peripheral branch of the facial nerve may be damaged or the inferior alveolar nerve injured in subcondylar fractures.
- Telescoped or impacted fracture: this type of injury is rarely seen in the mandible, but it implies that one bony fragment is forcibly driven into the other. This type of injury must be disimpacted before clinical movement between the fragments is detectable.
- Indirect fracture: direct fractures arise immediately adjacent to the point of contact of the trauma, whereas indirect fractures arise at a point distant from the site of the fracturing force. An example of this is a subcondylar fracture occurring in combination with a symphysis fracture.
- Pathologic fracture: a pathologic fracturis said to occur when a fracture results from normal function or minimal trauma in a bone weakened by pathology. The pathology involved may be localized to the fracture site, such as the result of a cyst or metastatic tumor, or as part of a generalized skeletal disorder, such as osteopetrosis.
- Displaced fracture: fractures may be nondisplaced, deviated, or displaced.
- A nondisplaced fracture is a linear fracture with the proximal fragment retaining its usual anatomic relationship with the distal fragment. In adeviated fracture, a simple angulation of the condylar process exists in relation to the remaining mandibular fragment, without development of a gap or overlap between the two segments.
- Displacement is defined as movement of the condylar fragment in relation to the mandibular segment with movement at the fracture site.The fragment can be displaced in a lateral, medial, or anteroposterior direction. In displaced fractures the articular surface of the condyle remains within the glenoid fossa and does notherniate through the joint capsule.
- Dislocated fracture: a dislocation occurs when the head of the condyle moves in such a way that it no longer articulates with the glenoid fossa. When this is associated with a fracture of the condyle, it is termed a fracture dislocation. Fracture dislocations are discussed more completely later in this chapter. The mandibular condyle may also be dislocated as a result of trauma without an associated condylar fracture. Dislocations can occur anteriorly, posteriorly, laterally, and superiorly.
- Special situations: other types of fractures that do not readily fit the above classification include grossly comminuted fractures or fractures.
Involving adjacent bony structures, such as the glenoid fossa or tympanic plate; open or compound fractures; and fractures in which a combination of several different types of fractures exist. Open fractures of the condyle are usually caused by missiles such as bullets.
Diagnosis
The diagosis of mandibular fractures must begin with careful history and clinical examination. Immediate attention should be given to problems associated with bleeding and airway compromise, which may threaten patient’s life.
In the diagnostic work-up phase, the lack of standardized ways to assess and characterize the nature and severity of the orofacial injury engenders variation in practice patterns. Symptoms of mandibular fractures include pain, malocclusion, numbness of the chin or lower lip, and abnormal lower jaw movement.
A careful history should be taken from the patient. What was the mechanism of the injury: fist, shod foot, baseball bat, fall, motor vehicle accident? Was the injury witnessed? Was there any loss of consciousness? Is there a previous history of facial trauma or fractures, either treated or untreated? Were there any pre-existing dental conditions such as deviated or limited opening of the mouth.
Clinical examination
The clinical examination should consist of inspection and palpation. It is best to proceed in an orderly fashion and to perform this evaluation as a component part of the entire head and neck examination of the trauma patient. The skin of the face and, in particular, the area around the mandible should be inspected for swelling, hematomas, and lacerations. Examination should first seek out intraoral and extraoral lacerations, abrasions, and ecchymoses. Common signs include sublingual hematoma; loose, avulsed, or fractured teeth; steps in the occlusal plane; or lack of complete intercuspation. The external auditory canal should be examined because displaced condylar fragments occasionally pierce the canal, causing it to fill with blood while the tympanicmembrane remains intact. Inability to open the mouth due to trismus (spasm of the masticatory muscles) or deviation of the chin to one side are also seen. Palpation anterior to the tragus will produce pain and reveal abnormal condyle motion in condylar neck fractures. Steps in the mandibular borders or mobile segments of the tooth-bearing alveolus suggest body fractures.
Patients often complain of the following:
- Pain or tenderness is often present at the site of impact with the possibility of a direct fracture, or at a distant site in the case of an indirect fracture.
- Difficulty chewing. Pain could be limiting mandibular function or there may be a malocclusion or mobility at the fracture site.
- Malocclusion. The patient may be able to tell the clinician about an alteration in the bite from normal; however, patients are not always reliable and may claim that the bite feels normal when it is not and vice versa.
- Numbness in the distribution of the inferior alveolar nerve. This usually indicates a displaced fracture in the region of the body or angle of the mandible on the affected side. A nondisplaced fracture often does not give rise to numbness in the distribution of the inferior alveolar nerve.
A common site for a laceration is under the chin, and this should alert the clinician to the possibility of an associated subcondylar or symphysis fracture. Typically, the patient who has suffered a fracture of the mandibular’s condyle will present with facial asymmetry. This is owing to the loss of the vertical height of the ramus on the side with the fracture, resulting in a shift of the mandible to the ipsilateral side.The best routine to evaluate facial fractures is to start at the top and work down, assessing the stability of the anatomic structures in a mediolateral fashion. It is best to begin the examination from behind the seated or supine patient. The clinician should palpate the movement of the condyle both over the lateral aspect of the joint and through the external acoustic meatus and observe the movement of the mandibule itself. If a unilateral condylar fracture is present, a subjective assessment can then be made between the palpable movement of one side compared with the other. Failure to detect the translation of the condyle.
Especially when associated with pain on palpation, is highly indicative of a fracture in this area. Palpation will frequently confirm tenderness over the lateral pole of the injured condyle with associated crepitation. However, in the case of fracture dislocations, the condyle may not be palpable. Any significant deviation on opening may be indicative of subcondylar fracture on the side to which the mandible deviates.To better evaluate this area, the fifth finger is placed in each acoustic meatus and the patient is asked to open and close the mouth. On opening, the mandible frequently shifts even more toward the side of the fracture as a result of decreased translation of the condyle on the injured side. As mentioned before, in unilateral fractures, there is deviation of the occlusion toward the fractured side, with prematureocclusal contact in the posterior region on that side. This results because the lateral pterygoid muscle on the fractured side pulls on the fractured segment and does not have any protruding influence on the mandible. The lateral pterygoid muscle on the contra lateral side is unopposed and thus causes deviation to the fractured side. The midlines no longer coincide, and there is an open bite in the body region on the contralateral side. This is often accompanied by fracture of the posterior dentition on the same side as the condylar fracture. If bilateral condylar fractures are present, the occlusion may not be deviated. The midlines are often coincident, and premature contact is present bilaterally on the posterior dentition with an anterioropen bite. The posterior dentition may be fractured on both sides in these situations. Often the patient with a fracture of the condylar process also has a limited range of motion. This limitation, however, is primarily caused by voluntary restriction as a result of pain. One has to keep in mind that any limitation of mandibular movement may also be a result of reflex musclespasm, temporomandibular effusion, or mechanical obstruction to the coronoid process resulting from depression of the zygomatic arch. Other less common findings include blood within the external auditory canal and, in the case of fracture dislocation, development of a prominent preauricular depression. Careful otoscopic evaluation of the external auditory canal is of particular importance in patients suspected to have suffered an injury at this level. Occasionally a fracture of the condylar process will produce a tear in thee pithelial lining of the anterior wall of the canal, which produces bleeding from the acoustic meatus. It is important to determine that this
Bleeding is not coming from behind a ruptured tympanic membrane, which may signify a basilar skull fracture. A detailed intraoral examination should be undertaken with good lighting and immediate availability of suction. The most common intraoral findings are malocclusion, fracture of the dentition, and decreased interincisal opening. Continuing with the systematic evaluationof the patient, it is suggested that examination of the soft tissues be undertakennext. The gingival tissue should be inspected for tears or lacerations. With the aid of a tongue blade, the floor of the mouth is examined; sublingual ecchymosisis almost pathognomonic of a fracture of the mandible. Next the dentition is examined for the evidence of broken teeth and forsteps or irregularities in the dental arch. The patient is asked to lightly bite the teeth together and to say whether the bite feels different from normal, following which the occlusion is inspected. Premature occlusal contacts are noted. The three causes of analtered occlusion in the trauma patient are a displaced fracture, a dental injury such as a displaced tooth, and a temporomandibularjoint effusion or dislocation. Ifthe patient is edentulous and hasintact dentures with him, these can be replaced in the mouth and the occlusion inspected. The mandibles hould then be grasped on each side of any suspected fracture and gently manipulated to assess mobility. If no fracture can be found but clinical suspicion remains high, the mandible may be compressed by applying pressure over both angles. This nearly always gives rise to pain at a fracture site. In the case of subcondylar fractures, firm posterior pressure on the chin will cause pain in the preauricular region.
Radiographic evaluation
To adequately screen for the presence of a mandibular fracture, at least two views at right angles to each other are necessary. The initial screening of patients could be effectively undertaken with a panoramic radiograph alone. 92 % Of fractures were seen on apanoramic radiograph alone, compared with only 66 % on a routine radiographic series without a panoramic view. However, in order to accurately visualize displacement it is recommened that the standard mandibular views consist of a panoramic radiograph, a posteroanterior mandibular view (Fig. 15.4), and reverse towne’s view. The latter view allows for visualization of the degree of medial or lateral displacement of the fracture and unveils injuries in which only subtle deviation is present, such as is seen in greenstick fractures, which are not readily evident on panoramic view. The panoramic radiograph usually requires the patient to be able to stand upright and also requires accurate patient positioning for good-quality films. In the severely traumatized patient, this may be difficult to achieve with some machines.

Fig. 15.4. Posteroanterior mandibular view of a 36-year-old male with parasymphysis (left) and angle (right) fracture
Further, mesiolateral displacement in the ramus and body and anteroposterior displacement in the symphyseal regions may also be difficult to visualize. The traditional lateral oblique views of the mandible can be used when panoramic films are not possible.They require accurate positioning of the patient and film to obtain useful views, particularly in the condylar area. A transcranial temporomandibular view may be a good addition in these circumstances. Accurate assessment of symphyseal fractures may be problematic with the standard views. A mandibular occlusal view is particularly useful in this scenario. It also aids in the assessment of the fracture of the lingual plate, particularly in very oblique fractures. Periapical views may also be necessary for evaluation of the teeth on either side of the fracture line to assess root fractures, periapical and periodontal pathology, and the relationship
Of the fracture line to the periodontal ligament of each tooth. If only one view is used, fractures can easily be missed.In the multiple-trauma patient for whom panoramic radiographs are not possible, lateral oblique views may be substituted. Other radiographic views that may be useful depending on the circumstances are posteroanterior mandibular, mandibular occlusal, and periapical. Linear tomographies of the temporomandibular joints can also be useful in the evaluation of fractures at the level of the condylar process. However, intracapsular fractures of the condylar head are often difficult to visualize accurately on plain films.The typical radiographic findings when a condylar fracture is present are the following: a shortened condylar-ramus length; the presence of a radiolucent fracture line or, in the case of overlapped segments, the presence of a radiopaque double density; and evidence of premature contact on the side of the fracture if the radiograph was taken with the patient in occlusion. If more accurate information of the involvement of the temporomandibular joint is required, axial and coronal computed tomography (CT) scans offer an excellent opportunity to study the fracture details.
Indications for CT scans are the following:
- Significant displacement or dislocation, particularly if open reduction is contemplated.
- Limited range of motion with a suspicion of mechanical obstruction caused by the position of the condylar segment.
- Alteration of the surrounding osseous anatomy by other processes, such as previous internal derangement or temporomandibular joint surgery, to the degree that a pretreatment baselineis necessary.
- Inability to position the multipletrauma patient for conventional radiographs.
(Ct scans may be the only useful radiograph that can be obtained).
Treatment
Mandibular fractures, once properly diagnosed, should be treated in a timely fashion. Coordination of treatment of the multiply injured patient by all involved services (general or trauma surgery, oral and maxillofacial surgery, otolaryngology, neurosurgery, etc.). Is critical to ensure optimal patient care. Most fractures can and should generally be treated within 48 h of initial presentation. Because many mandible fractures involve gingival tears extending to the teeth and alveolus, they are by definition compound into the oral cavity and prone to invasion by saliva and oral bacteria. Early immobilization of segments has been shown to reduce the risk of wound infections. Because of the high risk of bacterial contamination in mandible fractures, antibiotic treatment is a necessity in all compound mandible fractures both pre- and postoperatively. Teeth adjacent to fracture sites should be evaluated and assessed for their relative value for retention vs. Risk to treatment. Teeth in the line of the fracture that are periodontally compromised, mobile, or fractured beyond restorability should be removed prior to definitive treatment. These pose the risk of infection (and nonunion) as well as recuperative-phase pain to the patient. Partially fractured teeth in a patient with limited dentition may be useful to aid in closed reduction. In this situation, the tooth could be retained until the fracture treatment is complete before a final decision is made to remove or restore the tooth. Wisdom teeth (third molars) in the line of mandibular angle fractures can pose a significant infection risk. The decision to retain or remove these teeth is not simple, and should be made considering such factors: patient’s compliance and hygiene, interference with proper bony segment reduction, difficulty and risk of removal, relative bone available at the fracture site, open vs. closed reduction, and favorable vs. unfavorable fracture. Maintenance of proper oral hygiene, both pre- and postoperatively, is an important treatment adjunct in the management of mandible fractures. Loss of tissue barriers to bacterial invasion due to compound fractures in the line of teeth, gingival tears, hematomas, edema, and interference with natural cleaning mechanisms all increase infection risk. Proper oral hygiene using saline, peroxide, or medicated (chlorhexidine gluconate) rinses should be encouraged. Increased frequency of tooth brushing should be encouraged and the use of pulsatile irrigating devices is helpful in selected patients.
A proper diet and maintenance of nutritional status are additional requirement during postoperative care. Enduring 3–4 weeks of mandibular immobilization with maxillomandibular fixation (MMF) makes nutritional intake.
More difficult and weight loss is inevitable. However, a large selection of nutritional supplements is available to patients in liquid form that will minimize weight loss and malnutrition. Pre- and postoperative patient positioning and bedside suction devices can simplify the ability of patients to manage oral secretions and bleeding in the immediate postinjury or postsurgery period. Elevating the head of the bed to a 45 degree angle allows patients to clear secretions effectively. Postoperative steroids and the use of ice compresses can be effective at reduction of edema.
Closed reduction
Accurate reproduction of the pre-existing occlusal state of the patient is the cardinal rule in treatment of mandible fractures. Mandible fractures can be treated with a variety of techniques (open reduction, closed reduction, pin fixation, etc.) And with a wide variety of materials (wires, alloy plates, resorbable plates, lag screws, splints, etc.). However, proper treatment should be guided by using the simplest method to achieve the most predictable favorable result. If the principle of using the simplest method to achieve optimal results is to be followed, the use of closed reduction for mandibular fractures should be widely used. Therefore, the indications for closed reduction may simply be stated as all cases in which an open reduction is either not indicated or is contraindicated. Several conditions deserve specific mention. Grossly comminuted fractures are, as a general rule, best treated by closed reduction, because using open reduction techniques would jeopardize the blood supply to the small bone fragments and lead to an increased likelihood of infection. This category also includes gunshot wounds, which are particularly prone to infection. Fractures in the severely atrophic edentulous mandible represent a difficult clinical situation. On the one hand, there is limited osteogenic potential; the majority of the blood supply comes from the periosteum, so an open reduction further disrupts the blood supply. On the other hand, a stable, nonmobile reduction and fixation of these fractures is difficult with closed reduction techniques. Open reduction with limited dissection of the soft tissue and rigid fixation may be the preferred technique.
In situations where there is a lack of soft tissue overlying the fracture site, soft tissue flaps have to be transposed to cover a fracture site (particularly if a through communication exists between the skin and oral cavity). The presence of bone plates, screws, and wires may increase the likelihood of infection under these circumstances. Fractures in children involving the developing dentition are difficult to manage by open reduction because of the possibility of damage to the tooth buds or partially erupted teeth. Indications for closed reduction:
- Minimally to moderately displaced simple or compound fractures.
- Most condyle fractures.
- Fractures in children.
- Severely comminuted fractures or fractures in which overlying blood supply has been compromised.
Closed reduction of fractures of the mandible together with indirect fixation can be achieved by either the application of imf or by applying a technique to the mandible only. Simple, time-tested, and predictable closed reduction techniques for use in the four aforementioned categories are ivy loops and circumdentally affixed arch bars (Fig. 15.5).

Fig. 15.5. Arch bars application
Ivy loops, named for their proponent dr. Robert ivy, can be a simple and effective means of reducing and immobilizing minimally displaced favorable fractures in compliant patients with a stable occlusion (Fig. 15.6).

Fig. 15.6. Ivy loops application
A 24-gauge wire can be used to fabricate a loop on itself, and is affixed to teeth utilizing a needle driver, local anesthetic, and a wire cutter. Pigtails can be left on the wire ends to affix elastic or wire traction, elastics
Being preferred for patient safety. Ivy loops can be fixed to each dental quadrant singly or in pairs. Arch bar fixation is a time-tested and reliable technique that results in more stable fixation than ivy loops alone. Arch bars come in a variety of styles. The two force ends of the wire are tightened in a pigtail fashion over the bar under continuous apical pressure. Arch bar ligatures should typically run from the first or second molars to the canines. Anterior teeth can be utilized, when necessary, but caution should be used because wires have been known to orthodontically move incisors labially or rotationally. A smaller wire is recommended if anterior tooth ligation is needed. Reduction of segments should be with elastic or box wire traction of arch bars into an acceptable occlusion before definitive tightening of circumdental wires, proximal to the fracture site. Arch bars should be affixed tightly without evidence of vertical or horizontal mobility. Tooth-bearing fractures (symphysis, body) should, as a general rule, be reduced prior to non-tooth-bearing fractures (angle, ramus). Arch bars also provide a stable point of fixation for luxated mobile teeth and dentoalveolar segment fractures. Following closed reduction of fractures, it may be determined that a previously nondisplaced fracture, for example, in the angle, is now significantly displaced and nonreducible. In such cases, the practitioner will need to weigh the indications for open reduction and at times change the initial treatment plan. Closed reduction techniques demand patient compliance with maxillomandibular elastic traction (immobilization) for 3–4 weeks prior to release. Thus, patients with behavioral difficulties or those at risk for significant aspiration (alcoholics, patients with alzheimer’s disease) may require more predictable, definitive treatment or overtreatment to effect a more predictable outcome. Mobility at the fracture site has been shown to lead to malunion, nonunion, and osteomyelitis. Persistent trismus often results from prolonged maxillomandibular fixation; physical therapy is often useful to obtain a return to normal range of motion.
Principles of applying the arch bar and intermaxillary fixation:
- Adapt the arch bar closely.
- Use a cuspid wrap wire where indicated.
- Avoid placing the wire across the intermaxillary stabilization lugs.
- Use circumferential wires when single teeth stand alone, and intraosseous suspension or circummandibular wires in edentulous areas.
- In the area of the fracture, reduction should be accomplished prior to stabilization of the arch bar on both sides of the fracture.
- Tighten the wires with a continuous tension.
- Direct the force apically when tightening the wires.
- Tighten all wires in a clockwise direction.
- At the end of tightening, turn only half a turn at a time.
- Turn the end of the wire into the interproximal embrasure.
When imf is used it may be applied with either elastics or wires (Fig. 15.7). Elastics can be used for fracture reduction and for imf; however, they apply a constant pressure, which can lead to muscle spasm and pain, particularly in the masseter muscle, and they are difficult to keep clean. Wires, on the other hand, are easier to keep clean and are passive. However, they do loosen over time and may need to be tightened or replaced over the period of fixation.

Fig. 15.7. Intermaxillary fixation with elastics
Two other techniques categorized as closed reduction methods for treating mandible fractures apply to situations in which a dentate mandible opposes an edentulous maxilla, or vice verse. In the first case, the patient’s pre-existing denture can be modified with acrylic to fix an arch. This is then affixed to the maxilla by screw fixation at the pyriform rims, zygomatic buttresses, or palate. Pyriform rim wires or perialveolar wires can also be used. An arch bar is then affixed to the dentate mandible and a standard closed reduction is then performed using the maxillary denture as the occlusal basis for proper alignment followed by elastic traction fixation. Wires and /or screws are removed when the time treatment is completed. If a dentate maxilla opposes a fractured mandible with a limited number of teeth, a modification of the patient’s mandibular partial denture or fabrication of an acceptable splint can be performed in a similar way. This can then be affixed to the mandible via circummandibular wires, with care being taken to avoid wire proximity to the fracture site. Care should also be taken to avoid injury to the mental nerve as it exits the mandible and to the submandibular duct and contents of the floor of the mouth. A standard closed reduction can then be created via elastic traction fixation.
Open reduction
Indications for the open reduction:
- Moderate to severely displaced simple or compound fractures.
- Fractures nonreducible by closed means.
- Fractures opposing an edentulous maxilla or nonoccluding maxilla.
- Unfavorable fractures.
Excluded from these indications for special consideration are edentulous mandible fractures, mandible fractures in conjunction with panfacial fractures, and avulsive or pathological fractures. Open reduction techniques for treating mandible fractures are numerous, ranging from both intra- and extraoral approaches, with variations in materials such as wires, wire mesh, plates and screws, lag screws, eccentric dynamic compression plates (Fig. 15.8; 15.9).

Fig. 15.8. Fixation of fractured mandible with miniplate

Fig. 15.9. Postoperative view of fracture fixation by a miniplate on the superior border of the mandibular angle
Resorbable plates, and others. However, the basis for treatment by open reduction or closed reduction should be the same: reestablishment of an acceptable occlusal relationship for the patient in a predictable and safe fashion. In most cases requiring open reduction, a closed reduction is performed initially to approximate an occlusal relationship. A closed reduction serves to guide the practitioner in a functional as well as anatomical alignment of mandibular segments. With the occlusal relationship established, open reduction techniques then provide a means of rigidly or semirigidly immobilizing and maintaining bony segments in an acceptable position with or without compression. Bone edges approximated under compression are thought to undergo more rapid osseous healing. Extraoral approaches to the mandible include the submandibular or risdon approach, the retromandibular approach, the submental approach, the preauricular approach, and through existing lacerations. Each approach has its particular strengths and weaknesses. Intraoral access can be gained to most anatomical regions of the mandible via a vestibular incision in the mucosa or by a traditional Obwegesser is approach to the ramus and low condylar neck and coronoid regions. Extraoral approaches lend themselves well to the use of bone screws and rigid plating systems of all types, allowing wide visualization and the ability to place bicortical screws safely. Intraoral approaches are useful to access oblique fractures of the anterior mandible when lag screw fixation is desired and for placement of plates and screws (low condyle fractures) or border wires.
Wire osteosynthesis is a time-honored method for the treatment of mandible fractures. However, with the advent of rigid fixation techniques many practitioners now have limited experience in the use of direct transosseous wiring. In the case of a dentate mandibular fracture opposing a limited maxillary dentition, dental models can be utilized to fabricate acrylic splints with arch bars to establish a stable occlusal relationship. Long-term intermaxillary fixation is required when wire osteosynthesis is used as a treatment option due to the wire’s inability to limit multidimensional mobility at the fracture site during typical mandibular function. Wires can also be useful adjuncts to manipulate segments in conjunction with extraoral open reduction techniques. Rigidfixation techniques (or semirigid techniques) differ from wire fixation techniques in several important ways. Rigid fixation techniques maintain stability across a fracture site with an increased surface area (of device) to bone interface compared to wires and these techniques generally do not require prolonged intermaxillary fixation. However, there is a wide variety of alternatives to consider within this particular technique category: plate material and thickness, screw size and thread pitch, mono- or bicortical crews, tension band plates, neutral zone plates, compression plates, lag screws, reconstruction plates, wire meshes, and resorbable plates. Lag screws generate substantial cross-fragment compression and load sharing. The concepts of tension band plates, neutral zone (static plates), and compression plates are well documented in the literature. Compression plates (thicker bicortical-fixed plates) compress bony segments when placed across a fracture via eccentrically placed holes. This compression is believed to promote enhanced bony healing with no intervening callus formation. Tension band plates (smaller monocortical-affixed plates) resist tensile forces along the superior aspect of the mandible. Arch bars have been described as effective tension bands. Neutral or static bone plates (bicortical-fixed) do not offer compression across fracture lines. Wire mesh does offer some three-dimensional stability depending again on size and material. These meshes generally are indicated in avulsed or severely comminuted fractures requiring bone grafting. Resorbable plates and screws, currently under close scrutiny regarding biodegradation issues, still have considerable mechanical limitations over equivalent alloy plates and screws.
Fractures of the edentulous mandible are categorized unto themselves. The appropriate management option selected to treat the edentulous mandible fracture should take into consideration the age of the patient, the degree of functional disability postoperatively, the severity and type of fracture, and, most importantly, whether the mandible is edentulous and atrophic (pencil thin). Closed reduction technique using the patient’s existing dentures is indicated when MMF with splints will offer adequate segment control and reduction. Circummandibular wires are used to fix the denture or splint with an arch bar to the maxilla. The dentures or splints should be modified by placement of arch bars (or sections thereof) along the labial flanges and interocclusal keys should be developed occlusally to serve as occlusal stops to prevent sliding displacement. Since the blood supply to the atrophic mandible is nearly entirely supplied by the periosteum, open reduction techniques on these fractures should only done if closed reduction techniques (or biphasic pins) are unsuccessful.
Midfacial fractures. Etiology, pathogenesis, diagnostics and treatment. Complications of midfacial fractures. Management of complex craniofacial injuries and polytrauma
The maxillary bones are paired pyramidal bones that in many ways serve as the cornerstones of the facial skeleton. Each individual maxilla can be conceptualized as a 5-sided structure, the base of which makes up the lateral nasal wall. The remaining 4 sides of the pyramid are composed of the orbital floor superiorly, the alveolar ridge inferiorly, the front wall of the maxillary sinus anteriorly, and the anterior face of the pterygopalatine fossa posterolaterally. The maxilla forms the largest component of the middle third of the facial skeleton. It is closely associated with adjacent bones providing structural support for for occlusion and protection for the globes and brain. The whole midface represents the bridge between the cranial base superiorly and the dental occlusal plane inferiorly. In a transverse plane, it bridges the 2 zygomaticoorbital complexes. Midfacial skeleton contributes to form and function by establishing vertical facial height, providing anterior facial projection, and anchoring the maxillary dentition in establishing a functional occlusal relationship. It makes the maxilla a functionally and cosmetically very important structure. It consists of alternating thick and thin sections of bone that are capable of resisting significant force.
Midfacial fractures account for approximately 10–25 % of all facial fractures. They often result from high-energy blunt force injury to the facial skeleton. Typical mechanisms of trauma include motor vehicle accidents, altercations, industrial accidents and falls. Fracture of these bones is potentially life-threatening as well as disfiguring. Timely and systematic repair of these fractures provides the best chance to correct deformity and prevent unfavorable sequelae. Reestablishing continuity of the midfacial buttresses is the foundation on which maxillary fracture treatment is based.
There are horizontal and vertical buttresses or pillars of the midface that establish a relationship between the palate and alveolar process and the superior cranium and skull base region.
The major vertical buttresses of the midface include the zygomaticomaxillary, nasomaxillary and the posterior buttress. Zygomaticomaxillary buttress connects the lateral maxillary alveolus to the zygomatic process of the temporal bone. It transmits forces from the zygomatico-alveolar crest through the zygoma to the posterior aspect of the superior orbital rim and temporal bone. The nasomaxillary buttress reaches from the anterior maxillary alveolus to the frontal cranial attachment. It transmits force from the maxillary canine area through the lateral pyriform rim and frontal process of the maxilla and to the superior orbital rim. Posterior buttress involving the pterygoid plates connects the maxilla posteriorly to the sphenoid bone. It conducts force through the palatine bone to the pterygoid plates and sphenoid base. An additional unpaired midline support is the frontoethmoid-vomerine buttress. These pillars serve to diffuse the vertical forces of mastication over the broad cranial base. They are also effective shock absorbers for a vertically oriented impact to the facial skeleton.
The superior and inferior orbital rims and alveolar ridge constitute a group of weaker horizontal buttresses. While these structures provide some protection against horizontal forces, they can withstand much less force than the vertical buttresses. Therefore, vertical impact tends to be better absorbed within the facial skeleton, which resists fracture, while horizontal impact tends to overcome the weaker horizontal buttresses and shear through the vertical pillars. In a surgical approach to maxillary fractures, attempts should be made to restore the continuity of these support buttresses.
Between these structurally reinforced buttresses, the bone of the maxilla is usually thin. It covers the pneumatized maxillary sinus and forms the orbital floor. Due to this fact fractures of the midface in majority of cases result in orbital fractures.
The unique situation of the midface is its complexity of interaction of hard with soft tissue. Six cranial nerves are localized in the orbital area. Furthermore, in the midface, form, function, and esthetics are interdependent; even minor dislocations may be obvious to everyone. The complexity or simplicity of a fracture in the midface is not only based on the fracture morphology (ie, fragment size, number, dislocation) but on the degree of injury to the soft-tissue envelope.
Classification
Much of the understanding of patterns of fracture propagation in midface trauma originates from the experimental work of rené Le Fort. In 1901, he reported his work on cadaver skulls that were subjected to blunt forces of various magnitudes and directions. Le Fort considered several factors: the vectorof force overcoming the inertia of the face; the thickness of the bone and buttresses counteracting the mass, velocity, and point of application. He concluded that predictable patterns of fractures follow certain types of injuries. The recurring fracture patterns he described are still commonly utilized.
Three predominant types were described.
Le Fort I Fractures (Fig. 15.10A)
Le Fort I is also known as a horizontal maxillary fracture. It may result from a force of injury directed low on the maxillary alveolar rim in a downward direction. The fracture extends from the lower third of the nasal septum to the lateral pyriform rims, travels horizontally above the teeth apices through the base of the maxillary sinuses, crosses below the zygomaticomaxillary junction, and traverses the pterygomaxillary junction to interrupt the pterygoid plates. It separates the alveolar processes, palate, and pterygoid processes from the facial structures above. The superior two-thirds of the maxilla remain associated with the face. Fracture dislocations of segments of the alveolus may be associated with this fracture. The fracture lines of a Le Fort I fracture may be linear (simple) or comminuted (complex). With high-energy injuries, the palate may be split in the midline in addition to the Le Fort I fracture.
Le Fort II Fractures (Fig. 15.10B)
Le Fort II is also known as a pyramidal maxillary fracture. It may result from a blow to the lower or mid maxilla. Such a fracture has a pyramidal shape and extends from the dorsum of the nose at or below the nasofrontal suture through the frontal processes of the maxilla, inferolaterally through the lacrimal bones and inferior orbital floor and rim through or near the inferior orbital foramen, and inferiorly through the anterior wall of the maxillary sinus; it then travels underneath the zygomaticomaxillary buttress, across the pterygomaxillary fissure, and through the pterygoid plates. Various amounts of the pterygoid plates usually remain attached to the posterior maxilla. Thus, maxillary fractures at the Le Fort II level involve most of the nasal bones, the maxillary bones, the palatine bones, the lower two-thirds of the nasal septum, the dentoalveolus, and the pterygoid plates. The segments may be intact below this line of fracture, but they are most often comminuted.
Le Fort IІІ Fractures (Fig. 15.10C)
Le Fort III is also known as a craniofacial dysjunction because the entire mass of facial bones is separated from the cranial base. These represent the most superior pattern of the maxillary fractures. It may follow impact to the nasal bridge or upper maxilla. The fracture line begins at the frontozygomatic suture along the lateral aspect of the internal orbit along the sphenozygomatic suture line to the inferior orbital fissure, extends medially across the floor of the orbit up the medial wall of the orbit towards the dorsum of the nose where it crosses and proceeds to the opposite side in the same manner. Intranasally, a branch of the fracture extends through the base of the perpendicular plate of the ethmoid, through the vomer, and through the interface of the pterygoid plates to the base of the sphenoid. Various amounts of the pterygoid plates usually remain attached to the posterior maxilla. Le Fort III fractures are often associated with head injuries, dural tears with associated cerebrospinal fluid (csf) leaks, significant orbital trauma, and other fractures of the craniofacial skeleton.
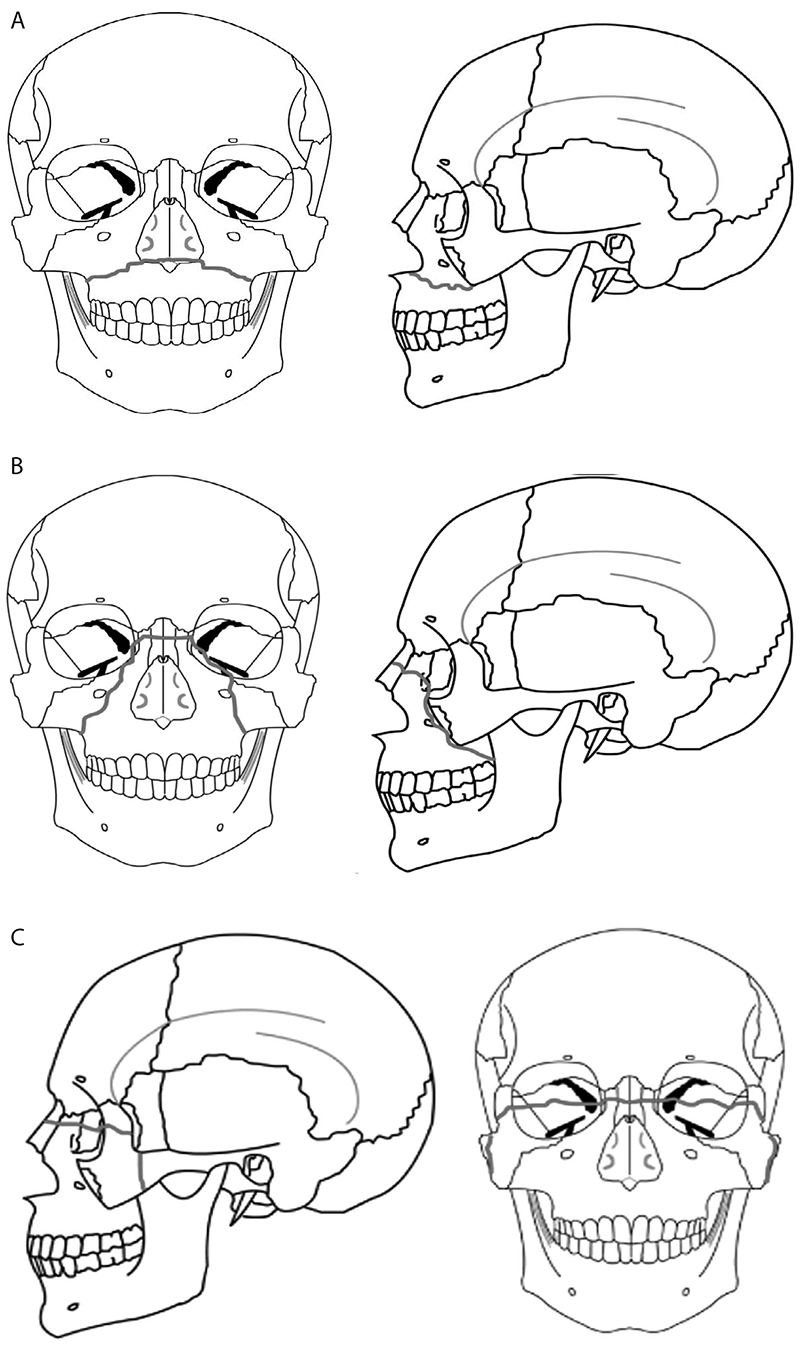
Fig. 15.10. Anteroposterior and lateral views of the skull showing the Le Fort classification system of maxillary fractures:
A – Le Fort I fracture; B – Le Fort II fracture; C – Le Fort III fracture
In reality, the Le Fort classification is an oversimplification of maxillary fractures. It described the typical lines of weakness in the face using low-velocity impact forces directed against cadaver skulls. The amount of force impacted during a motor vehicle accident is much greater than Le Fort took into consideration during his work in the late XIX century. Pure Le Fort I, II, and III fractures are rare. In most cases, maxillary fractures are a combination of the various Le Fort types. Fracture lines often diverge from the described pathways and may result in mixed-type fractures, unilateral fractures, or other atypical fractures. Segmental alveolar fractures of the tooth-bearing region can occur without a Le Fort I. Fractures of the thin maxillary wall without buttress involvement are also common. Parasagittal fractures of the palate also occur, often in combination with typical midface fractures.
The range of combined midfacial/panfacial fractures is enormous. This is due to the variety in possible mechanisms which occur during impact leading to the midfacial injury. In general, low velocity trauma less often leads to severe midfacial fractures than high velocity trauma.
Unlike with fractures in other bones, maxilla is practically unaffected by muscle pull, muscle forces do not play a significant role in the final position of the broken bony segments. Instead, the basis for the patterns of maxillary fractures depends on location, direction, and energy of the impact result in different injuries. Second factor is the anatomy of the mid face which provides strength and support to protect against injury.
Clinical evaluation and diagnosis
Evaluation of the maxilla and facial bones should be undertaken only after the patient has been fully stabilized and life-threatening injuries have been managed.
After initial stabilization of the trauma patient, evaluation of the facial injuries should commence with reassessment of the patient’s airway neurological, visual, and cervical spine status. Oral bleeding, loose teeth, edema, or associated mandible fractures may lead to airway problems. Head injuries are often associated with midface fractures and csf leaks should
Be suspected in patients with Le Fort II or III type fractures. The presence and extent of other injuries in patients with multiple trauma may influence the timing of fracture repair and patient outcomes. Information regarding the mechanism of the injury may assist in determining a diagnosis. In particular, knowing the magnitude, location, and direction of the impact is helpful. High-energy trauma is oftern associated with concomitant injuries. A history of mental status changes or loss of consciousness should cause concern regarding intracranial injury.
A careful and thorough evaluation of the eye and orbit is paramount. Every patient with orbital fractures should have an examination that includes visual acuity testing, visual field testing, ocular motility, binocular vision, globe position, pupillary reaction, intraocular pressure testing. In some cases preexisting optical correction by glasses or contact lenses or ocular disorders such as cataract, glaucoma, and retinal disorders can compromise basic visual acuity testing.
During examination of the eyes and orbit, the integrity of the orbital rims, orbital floor and intercanthal distance are also examined. Unlike Le Fort II fractures, Le Fort III fractures are associated with lateral rim and zygomatic breaks. Visual changes may signify a disturbance of the optic canal, problems within the globe or retina, or other neurologic lesions. An increased intercanthal distance implies displacement of the frontomaxillary or lacrimal bones or avulsion of the medial canthal ligament. For extensive involvement of the orbit or globe, consultation with an ophthalmologist is necessary. The standard assessment of visual status can be performed in the conscious patient. In the unconscious patient only regular light reflex testing is performed.
Associated soft tissue injuries of the face need to be cleansed and evaluated regarding the need for early repair. Focal areas of swelling or hematoma may overlie an isolated fracture. Periorbital swelling may indicate Le Fort II or III fractures.
Intraoral assessment of the patient’s dentition and occlusion should begin with the examination of the palate and maxillary alveolus for loose or missing teeth, lacerations, bleeding, and abnormal mobility. The maxillary segment is displaced posteriorly and inferiorly. This may cause premature contact of the molar teeth, resulting in an anterior open bite deformity.
The maxilla and palate will often be unstable and mobile on bimanual examination with Le Fort fractures and the midface may have a characteristic retrusion with loss of projection.
Asymmetry of the nose, traumatic telecanthus, a flatnasal bridge, and a dish-shaped face can be noted. A global posterior retrusion of the midface creates a flattened appearance of the face in Le Fort II or Le Fort III fracture. Intraorally the examiner may see fractured teeth, vestibular ecchymosis and edema, palatal ecchymosis, mucosal lacerations and bleeding, steps or diastema in the maxillary teeth, and malocclusion. Finger palpation of the maxillary contour intraorally may provide additional information about the integrity of the nasomaxillary buttress, anterior maxillary sinus wall, and zygomaticomaxillary buttress.
The skeletal framework of the faceshould be carefully palpated to detect for bony irregularities, step-offs, crepitus, and sensory disturbances. In many patients with facial fractures the bone injury may be obscured with soft tissue swelling, ecchymoses, wounds, and hematomas. With respect to the maxilla, the alveolus should be palpated and any fractures or mobility noted. Mobility of the midface may be tested by grasping the anterior alveolar arch and pulling forward while stabilizing the patient with the other hand. The size and location of the mobile segment may identify which type of Le Fort fracture is present.
Nasal fractures and associated epistaxis are common inpatients with midface fractures. Examination of the nose starts with inspection for swelling or asymmetry, followed by palpation. Characteristic signs for nasal fractures are:
- Pain.
- Bleeding.
- Swelling.
- Compromised nasal airway.
- Crepitation.
- Palpable bony dislocation.
If the nasal airway passage is compromised the reason has to be investigated.
Nasal inspection using a speculum with appropriate light (headlights are recommended) allows for examination of the nasal cavity. If further clinical examination of more posterior or cranial parts have to be performed, additional nasal endoscopy may be indicated.
The nasal bones are typically quite mobile in Le Fort II fractures, along with the rest of the pyramidal free-floating segment. Intranasal examination may reveal fresh or old blood, septal hematoma, or cerebrospinal fluid rhinorrhea.
Clinical signs for midfacial fractures:
- Facial swelling (edema, hematoma, emphysema), and deformity.
- Subconjunctival bleeding (hyposphagma).
- Oronasal bleeding.
- Palpable and crepitating dislocated bony contour in the periorbital region.
- Displacement of the globe (hyper-, hypo-, eno-, exophthalmos).
- Displacement of the medial canthal tendon (depending on the degree of noe fracture).
- Compromised ocular motility.
- Double vision.
- Sensory deficit (hypoesthesia, anesthesia, paresthesia) of the trigeminal nerve.
- Localized pain.
- Occlusal disturbance.
- Csf leakage (in case of anterior skull base involvement).
Clinical signs of Le Fort I
In a recent injury there may be slight swelling of the upper lip, but there is none of the massive oedema of the face which characterizes Le Fort II and III fractures. Typically ecchymosis is present in the buccal sulcus beneath each zygomatic arch. The occlusion is disturbed and a variable amount of mobility may be found in the tooth-bearing segment of the maxilla. Some Le Fort I fractures are so mobile that the whole fragment drops and the patient.
May have to keep the mouth slightly open to accommodate the increased vertical dimension of the bite. This situation may result from a direct blow from a sharp object in the front of the mouth above the apices of the teeth. When this happens a soft-tissue laceration is often present, and in extreme cases the resulting down-fracture of the maxilla may be so gross that it may be possible to see directly into the nares and the maxillary antra through the upper lip.
Most Le Fort I fractures are not as mobile as this. Indeed, the impacted type fracture may be almost immobile and it is only by grasping the maxillary teeth and applying slight but firm movement, that a characteristic grate can be felt which is diagnostic of the fracture. The maxillary cheek teeth should be moved apart in the same way to make sure there is no associated midline split in the palate.
In the impacted type of fracture there may be damage to the cusps of individual teeth, usually in the premolar region, caused by the impaction of the mandibular teeth against them. Percussion of the upper teeth results in a distinctive “cracked-pot” sound, similar to that produced when cracked china is tapped with a spoon. This sign is present whenever there is a fracture of the central mid-face, but is particularly valuable in the diagnosis of Le Fort I fractures.
All possible variations of open and closed type fractures may occur and it is possible to see the condition unilaterally when it involves only one maxilla, the tooth-bearing portion being split along the median palatal suture. The complete Le Fort I fracture is often associated with a split in the palate, sometimes along more than one line so that each of two or more fragments may be mobile. Multiple alveolar fractures of this nature are frequently complicated by damaged or subluxed teeth.
Clinical signs of Le Fort II
The most obvious difference between the Le Fort II and III fractures, from the clinical point of view, is the detection of a step deformity in the bone of the infra-orbital margin. This is made more apparent when the zygomatic complex on each side is intact.
As the fracture line passes across the inferior orbital rim, there is likely to be associated injury to the infra-orbital nerve resulting in anaesthesia or paraesthesia of the cheek.
Similarly the fracture line in the orbital floor may result in limitation of orbital movement in an upward direction with diplopia and possibly enophthalmos.
Because the line of fracture is below the lateral attachment of the suspensory ligament of lockwood, alteration of the pupil level does not occur unless there is an associated fracture of the zygomatic complex.
Gagging of the occlusion and retropositioning of the maxilla as a whole will be noted on intra-oral examination, but when the maxillary teeth are grasped, it will be noted that the mid-facial skeleton moves as a pyramid, the movement being detected at the infraorbital margins and nasal bridge.
The Le Fort II fracture may be impacted in the same manner as the Le Fort I, in which case little or no mobility can be detected. There is frequently a midline or paramedian split in the pyramidal block. The passage of the fracture line across the zygomatic buttress gives rise to haematoma formation in the upper buccal sulcus on each side, opposite the first and second molar teeth.
Unless the fracturing force was applied directly to the nasal region, the comminution of this part of the pyramidal block is usually minimal. In the same way there is less danger of extensive associated fracture of the anterior cranial fossa in the region of the cribriform plate, and cerebrospinal fluid rhinorrhoea is therefore not a constant clinical finding. However, when a Le Fort II fracture is present, it must be assumed that a breach of the dura mater has occurred, even if overt leakage of cerebrospinal fluid is not detected.
Clinical signs of Le Fort III
Superficially the Le Fort III fracture appears very similar to the Le Fort II fracture, but it is usually obvious that the injury is very much more severe. It is, however, very unusual to find a Le Fort III fracture occurring in isolation:
- There is tenderness and often separation at the frontozygomatic sutures. The amount of separation may not be symmetrical in which case the facial skeleton will be tilted to the side opposite to the direction of the fracturing force.
- Separation of both frontozygomatic sutures produces lengthening of the face and lowering of the ocular level, due to the fracture passing above whitnall’s tubercle, removing the support given to the eye by lockwood’s suspensory ligament. As one or both eyes drop, the upper lid follows the globe down, producing unilateral or bilateral pseudoptosis described as “hooding” of the eyes.
- A complete fracture at the Le Fort III level cannot occur without fracture of each zygomatic arch. Coincident independent fracture of one or other zygomatic complex occurs almost invariably. The displacement of the zygomatic complex will be detectable by palpation, which will reveal flattening and a step deformity at the infra-orbital margin. The arch of the zygoma will exhibit tenderness and some deformity in a pure Le Fort III fracture.
- If a finger and thumb are placed over the frontonasal suture region, and the dento-alveolar portion of the upper jaw is grasped with the other hand, movement of the entire face can be demonstrated. As mentioned previously the zygomatic bones may often be independently mobile.
- Intra-orally there is gagging of the occlusion in the molar area, as in other fractures of the mid-face. When lateral displacement has taken place, the molar teeth will be found to be gagged on one side only with a posterior open bite on the opposite side, and deviation of the upper midline. The entire occlusal plane may have dropped, holding the mandible open, a dramatic but rather unusual finding.
- A very loose Le Fort III fracture is usually associated with disruption of the cribriform plate area, and this type of fracture may therefore produce a profuse cerebrospinal fluid rhinorrhoea. In this situation the possibility of an intracranial aerocele must be considered seriously, and serial radiographs of the skull should be taken during the first few days after injury.
Clinical signs of nasal complex fractures:
- Bruising of skin over nasal bones.
- Laceration of skin of bridge of nose.
- Bilateral medial orbital ecchymosis.
- Epistaxis.
- Deformity of nose.
- Crepitus of bones of nasal complex.
- Unilateral or bilateral telecanthus.
- Airway obstruction.
- Septal deviation.
- Septal laceration or haematoma.
- Cerebrospinal rhinorrhoea.
Imaging
Fractures are identified clinically and confirmed radiographically. In the past the waters’ view and lateral facial radiographs were used in identifying maxillary fractures and may still be used today in remoteareas without access to a computedtomography (CT) scanner.
Fine details of the fracture sites are difficult to visualize. Axial and coronal CT scans of the midface should be obtained if a scanner is available. If clinical evidence strongly indicates maxillary fracture (midface mobility and malocclusion with intact mandible), then CT imaging is a confirmatory test for maxillaryfractures. Important indications forct scanning are suspected orbital floor fractures (best diagnosed in the coronalview) and surgical planning. CT scans can also demonstrate the soft tissue differences of hematoma or edema of the subcutaneous tissue, muscle, and fat. For severe midface trauma or maxillary displacement the three-dimensional CT scan is available.
Radiological assessment with plain films has limited value and should be reserved for situations in which computed tomography (CT) is not readily available. CT scans have dramatically changed the evaluation of midface fractures and all patients with suspected midface fractures should be scanned. Besides axial CT scans, coronal imaging (true coronals when feasible or coronal reformats of axial scans) is frequently useful in better evaluating the extent of orbital fractures. Although the Le Fort classification system is still widely employed and useful for describing fracturepatterns, CT scans are better able to evaluate and delineate precisely the exact location and extent of fractures. Most fractures in this region are comminuted
And usually involve different components of pure Le Fort-type fractures. CT scans provide superior guidance for treatment planning.
Imaging in patients with midfacial fractures
To assess the individual extent and type of fracture, CT or cone-beam based radiological examination should be performed. It is strongly advised to obtain postoperative CT scans to assess the surgical result.
By obtaining CT axial fine slices, the surgeon can obtain excellent reformatted coronal, oblique parasagittal views. The surgeon can also obtain 3D views. Examination of the craniofacial skeleton vastly benefits from 3D imaging and interactive image analysis. The modern surgeon should be trained to use the dicom voxel data set for multiplanar and 3D image analysis. The modern surgeon should be able to use full radiological information and not a limited selection of print outs or digitized views.
The surgeon thus changes his or her former role as a consumer of radiological information to interpreter of this data set. Having implemented computer assisted fracture assessment, much more detailed preoperative information is available to the surgical team. Radiological information acquired intraoperatively can be compared with different data sets (obtained pre- and postoperatively) via image fusion.
If no adequate visualization software for the dicom data sets is available, then CT axial, coronal, and oblique parasagittal views of the midface for simple fractures, with 3D views for more complex fractures are recommended.
Cone-beam technology allows adequate determination of the hard tissue problems, but is not equivalent to ct technology in terms of soft-tissue assessment (eg. Retrobulbar hematoma). Further limitations of cone-beam technology are given by a more limited scanning region. Cone-beam technology is becoming more important for pre-, intra- (3D C-arm), and postoperative imaging. Because there is less exposure to radiation, cone-beam scan may be more suitable for follow-up.
Prior to ct imaging, 2D X-rays had been considered adequate for pre- and postoperative diagnostics in orbital floor fractures. One of the great weaknesses of 2D imaging is that in many cases the modality may reveal a fracture, but not the degree of fracture displacement. With the availability
Of CT imaging, the surgeon can better define fractures, as well the degree of fracture displacement and the need for reduction. Plain X-rays therefore should only be considered appropriate if ct is unavailable or if distinct information for hard-tissue structures involved such as dentition (dental X-ray, orthopantomogram) is required.
2D imaging can include:
- Water’s view (this was a plain X-ray used for visualizing sinus fractures before CT was available. This offers poor visualization of fractures and does not provide the surgeon with adequate information about fracture displacement).
- Orthopantomogram (opg) this is a standard view normally used for the mandible, but can also provide information regarding midface:
- Lateral view (cephalic).
- Submentovertex view (for zygomatic arch injuries).
MRI or ultrasound can be helpful in some specific questions related to soft tissues but is in most cases not included in standard diagnostic workup (one exception is optic nerve sheath hematoma detection).
2D imaging particularly lacks precision for the sagittal extent of the injury. Treatment for midfacial fractures based on 2D imaging risks underestimating the severity of the injury. This might result in later deformities such as enophthalmos or hypophthalmos which could have been avoided by 3D preoperative radiological examination.
Special scanning procedures might be necessary if the anterior or lateral skull base is involved and, particularly, for detection or control of CSF-fistula or aneurysms. Special fine slices may be considered for the petrous portion of the temporal bone, particularly in cases where there is paralysis of the facial nerve.
In the event of accompanying dental trauma with missing tooth parts or empty alveolar sockets, it is important to determine the location of the missing elements. For dislocations of teeth into the jaws, standard orthopantomogram (OPG) is helpful. If the missing tooth or tooth parts cannot be localized, additional radiographs of the upper and lower airways (including frontal and/ or lateral cervical X-ray, frontal and/or lateral chest X-ray) and/or upper and
Lower gastrointestinal pathway should be considered. Additional endoscopic measures may be considered in retrieving dislocated dental fragments.
Management of the maxillary fractures
Definitive surgery should not be undertaken until the patient has been stabilized regarding other life-threatening injuries.
Initial attention should be directed at establishing an airway and controlling hemorrhage as the patient may die of concomitant injury or failure to manage the sequelae of maxillary fractures. The most frequent cause of hemorrhage in Le Fort level fractures is a fractured septum. This bleeding may be managed by placing nasal packs including gauze packing. Bleeding from sites of laceration or abrasion may be controlled by tamponade.
In case of severe bleeding the following options should be considered:
- Compression: either by nasal packing, balloon tamponade, or direct compression.
- Electrocautery: if a clear bleeding source can be evaluated.
- Control and adjustment of blood pressure.
- Assessment of current medical treatment for anticoagulation.
- Interventional embolization when other methods fail.
- In some cases fracture reduction may be required to reduce bleeding.
There are also a variety of possible injuries affecting the globe that may require immediate treatment. Pressure increase in the periorbital region due to retrobulbar hematoma can cause significant injury of the neurovascular structures with eventual loss of vision. If a retrobulbar hematoma leads to a tense, proptotic globe, emergency decompression should be considered. Transcutaneous transseptal incisions may help evacuate the hematoma and release the periorbital pressure. Alternative methods such as transconjunctival pressure release and/or lateral canthotomy and inferior cantholysis should be considered according to patient condition. Special attention has to be paid to the posterior third of the orbit and the bony optic canal. Bony dislocations in these anatomical areas are more likely to be associated with traumatic optic nerve lesions.
Careful coordination with the anesthesiologist regarding airway management using nasal or oral intubation. In many cases nasal intubation may interfere with reduction of nasal and midface fractures, while oral intubation may hamper evaluation and restoration of occlusal relationships. In this cases submental/submandibular intubation and/or tracheostomy should be considered.
In midfacial fracture repair the time frame regarded appropriate for primary fracture treatment is limited to 2 weeks (not including accompanying complications requiring immediate treatment, such as dentoalveolar trauma or post-traumatic visual loss). As soon as the general condition of the patient allows, definitive treatment should be undertaken. After 2 weeks, the treatment is regarded as delayed and thus has to follow the protocol of secondary post-traumatic reconstruction.
Extensive maxillary fractures are usually associated with significant cosmetic and functional sequelae. Expeditious definitive therapy is needed to best correct these problems.
Treatment of midface fractures aims to restore preinjury facial appearance and occlusion by restoring anterior facial projection and vertical facial height. Fracture treatment should be customized to the extent and location of the fractures based on clinical evaluation and CT scan findings. Dental occlusion is the most important parameter in reestablishing facial contour, reduction of fracture, and obtaining postoperative chewing function. The most common means of placing the patient into maxillomandibular fixation is the application of arch bars. A second surgical principle is to achieve anatomical correct repositioning of all midfacial bones. The height, width, and projection must be reestablished. Successful reconstruction of midfacial fractures is obtained by reestablishing the midfacial buttresses. If available, dental casts, stereolithographic models, and/or premorbid photographs may be useful guides for treatment.
Nondisplaced fractures may require minimal treatment. Maxillary fractures isolated to the dentoalveolar process and involving bone should be manually reduced and rigidly fixated with arch bars and ligature wires.
Rigid fixation techniques in the dentate patient begin with fixation of the occlusion. This ensures that the patients maintain their preoperative occlusal status.
There are several techniques to providing mandibulo-maxillary fixation. The gold standard in mandibulo-maxillary fixation is the use of arch bars. However, there are various methods of mandibulo-maxillary fixation to be used in specific clinical situations. Strong consideration should be given to the repair of any mandible fracture before the maxilla is stabilized.
Common mandibulo-maxillary fixation methods are:
- Arch bars.
- Ernst ligatures.
- Ivy loops.
- Gilmer wiring.
- Stout wiring.
- Kazanjian buttons.
- Bone supported devices including intermaxillary fixation screws, hanger plates and interarch miniplates.
Arch bars are preferred for temporary fragment stabilization in emergency cases before definitive treatment. They are used as a tension band in combination with rigid internal fixation or for long-term fixation in conservative treatment. The method is also used for fixation of avulsed teeth and alveolar crest fractures.
Before placing the arch bars the occlusion must be checked. Determine if the patient has a normal occlusion or a preexisting malocclusion before taking the patient to the operating room. In the case ofjaw malformations, such as a deep bite deformity, it may be impossible to use arch bars.
The prefabricated arch bar must be adjusted in shape and length according to the individual situation. The arch bar should not damage the gingiva. Firstly, the bar is adapted closely to the dental arch. It should be placed between the dental equator and the gingiva.
The hooks should be symmetrically positioned in the upper and lower jaw, because the symmetry is essential for right placing of the elastics. The bar should not extend past the most distal tooth or protrude into the gingiva.
One pitfall when using arch bars is the risk of contamination of blood-borne infection from patients. Passing the wires to secure the arch bar can.
Result in a puncture or tear in the surgeon’s glove and the possibility of disease transmission to the surgeon.
To fix the arch bar in place, a ligature is prepared in the premolar region of each side. The wire ends should not damage the surrounding soft tissues. After positioning the arch bar it is fixed with ligature using the wire twister. One end of the wire is above the arch bar and the other end below it. The wire is then cut with the cutter and its ends are turned away from the gingiva to prevent damage.
Mandibulomaxillary fixation can be used either intraoperatively to establish the correct occlusion or as part of postoperative management of the patient’s injury. Mandibulomaxillary fixation may be accomplished with wires or training elastics depending on the overall treatment plan for this patient. The wire loop is placed over the maxillary and mandibular lugs of the arch bar and the wire loop is tightened. Mandibulomaxillary fixation completed with wire fixation. At least three wires or elastics, a posterior wire loop in each side, and an anterior wire loop will provide stable fixation.
In cases of gross comminution, periodontal disease, or inadequate partial dentition (less than three occluding teeth per sextant), occlusal wafers or palatal splints are useful. These splints are fabricated after impressions have been taken. The gunning’s splint has been used to establish intermaxillary fixation for edentulous patients; this splint is essentially a denture base plate fabricated to the existingedentulous or partially edentulous ridgewith arch bars or suspension brackets. Dentures can also be secured to the jaws with bone screws before intermaxillary fixation is attempted.
Temporary mandibulomaxillary fixation during reduction serves to address the posterior height of the facial skeleton by utilizing the height of the ramus of the mandible, since the posterior maxillary buttress is not directly opened. Additional use of mandibulomaxillary fixation in the postoperative period for 2–4 weeks may be necessary depending on the fracture pattern and stability achievable in individual situations.
However, in many cases techniques of closed reduction alone led to complications including lack of midface projection and loss of vertical height. As a result, extended open reduction techniques were developed initially using wire and subsequently miniplate fixation of the maxillary buttress
System, along with concurrent treatment of associated fractures in order to avoid or minimize such complications.
As a general principle, all fractures should be exposed and reduced before plating.
Open reduction and internal fixation of midfacial fractures are usually accomplished via an intraoral sublabial approach with gingivobuccal incisions placed unilaterally or bilaterally, depending on the extent of fractures requiring subperiosteal exposure and reduction. This approach can be combined with various other methods including a transconjunctival approach to the orbital floor and rim, depending on fracture extent. Other approaches used to give access to the inferior, lower medial, and lateral aspects of the orbital cavity are subciliary, subtarsal, and infraorbital approaches.
Le Fort III fractures will often require an additional coronal approach for adequate exposure and reduction of the fracture. The coronal or bitemporal incision is also used to approach the anterior cranial vault, the forehead, and the upper and middle regions of the facial skeleton.
In some cases the glabellar approach can be used to expose nasoethmoidal fracture. It is particularly advantageous in elderly patients who have developed horizontal glabellar furrows. Facial fractures are often associated with lacerations. These existing soft-tissue injuries can be used to access directly the facial bones for management of the fractures.
The maxilla should be stabilized to the next highest stable facial structure, which varies with Le Fort fracture level. At the Le Fort I level, fixation is placed along the vertical buttresses of the maxilla at the piriform and zygomatic buttresses. The reconstruction sequence to reestablish midfacial pillars and dimensions begins with establishing the most reliable reference structures. This can be occlusion, an outside-to-inside or an up-to-down procedure as a first step. At higher Le Fort levels it may be necessary to use fixation to the nasalbones, the orbital rims, or the zygomaticofrontal sutures. The importance of achieving accurate three-dimensional reduction of the fractures along with accurate alignment of the occlusion prior to applying internal fixation cannot be overemphasized. Accurate reduction and titanium miniplate fixation of the fractured nasomaxillary and zygomaticomaxillary buttresses are key elements in stabilizing Le Fort I and II fractures. This should be accomplished after associated fractures are addressed, especially.
In patients with Le Fort II and III fractures, and the patient is placed in maxillomandibular fixation for occlusal alignment. Perioperative prophylactic antibiotics are prescribed in patients with midfacial fractures.
The introduction and acceptance of low profile titanium miniplates (1.5–2.0 mm screws) have improved the ability to stabilize the majorload-bearing midface buttresses. Even smaller microplates (1.0–1.3 mm screws) assist in stabilizing multiple comminuted segments in non-load-bearing regions after fixation of the major buttresses.
Complexity of fracture fixation is not only determined by fracture morphology, including the number of fracture lines, but also depends on the necessary approach, accessibility, visibility of the area of interest and the stability of the fracture reduction.
Every under- or overcontouring of the bony midface in primary fracture repair results very likely in unfavorable projection of the soft-tissue mask and this again results in an esthetic compromise. In addition, functional disorders may follow such as malocclusion or orbital dysfunction.
The number, size, and position of plates and screws might vary according to the biomechanical needs and individual fracture situation.
In cases of comminution with small fragments, surgical exposure may require these fragments be removed, resulting in a defect fracture. Immediate bone grafting has been advocated for the severely comminuted maxillary antrum. This treatment prevents prolapse of the facial soft tissue into the maxillary sinus and the facial deformation that results. Titanium mesh works well for this procedure. The use of plate fixation should be kept to the minimum required to achieve fracture stabilization. Multiple facial fractures should be treated as separate units.
Complications:
- Infraorbital nerve paresthesia.
- Enophthalmos.
- Infection.
- Exposed hardware.
- Deviated septum.
- Nasal obstruction.
- Altered vision.
- Nonunion.
- Malunion or malocclusion.
- Epiphora.
- Foreign body reactions.
- Scarring.
- Sinusitis.
Some of it may not be readily apparent untilweeks or months after injury, but the potential for their occurrence should be in mind during evaluation and treatment of the patient. Perioperative and postoperative airway obstructions are unusual in cases of maxillary fracture alone. However, these conditions may occur in association with extubation while the patient is obtunded,with a septal hematoma or nasal packing, and with excessively edematous soft tissues that do not allow breathing through the nasal airways. Patients with intermaxillary fixation and complete dentition may have difficulty breathing during this time. Reintubation, opening nasopharyngeal airways, or merely removing the intermaxillary fixation may be effective. Uncorrected nasal septal fractures can lead to postoperative airway obstruction that remains afterall soft tissue swelling has resolved. Acute sinusitis can result from prolonged nasotracheal intubation. Acute or chronic sinusitis may also occur in the ethmoid, sphenoid, frontal, and maxillary sinuses because fractures may obliterate or obstruct the sinus ducts or ostia. Postoperative hemorrhage occurs if arterioles and veins are not ligated when lacerations are repaired, if inadequate bone reduction allows continued oozing of blood. Lacerations should be reexplored so that hemorrhage can be controlled. Hematomas should be drained. Oozing of blood from bone requires re-reduction or the use of bonewax. Hemorrhage from a major artery requires emergency tamponade; if the source cannot be identified, then arteriography and embolization are indicated. Aneurysms and pseudoaneurysms are complications of maxillofacial trauma but rarely occur as the result of isolated maxillary fractures.
They can also result in postoperative bleeding and are indications for angiography and embolization. Because of the proximity of the maxillato the orbits, complications associated with vision can occur. Blindness is rarely associated with midface fractures and is most often seen in fracture
Patterns involving the orbit, often with a more severe mechanism of injury. Immediate postoperative blindness can be a complication of the reduction of high Le Fort fractures (Le Fort III or fractures involving the orbits) and occurs because of increased intraorbital hemorrhage or pressure, a retinal artery spasm, retrobulbar hemorrhage, or the impingement of bone fragments on the optic nerve. An undiagnosed or inadequately treated orbital floor fracture (alone or in combination with a zygomatic omponent) can lead to enophthalmos and diplopia.The most obvious postoperative complication sare misplaced bone segments or fixation devices. These complications are readily identified by clinical examination (eg., Alocclusion) or postoperative radiographic examinations. A second surgical procedure will correct such complications. Other complications related to rigid internal fixation include palpability, infection, extrusion or exposure, translocation, stress shielding, cortical osteopenia, and nonunion. Nonunion of the fractured segments can occur as the result of inadequate blood supply, inaccurate position, movement of segments, infection, or nutritional deficiencies. 50 Infections may be caused by contaminated soft tissue lacerations or foreign bodies, hematomas, or odontogenic infections from previously diseased or fractured teeth. Infection round bone plates and screws can occur years after their placement. Malunion of maxillary fractures can obstruct the nasolacrimal ducts. This obstruction causes epiphora and may lead to episodes of dacryocystitis. Bone segments from fractured or improperly reduced maxillary fractures can also impinge on the infraorbital nerve, causing numbness of the distribution of the second division of the trigeminal nerve. Although the reduction and fixation of maxillary fractures may at times seem straightforward, the proximity of complicated anatomic structures and the consequences of inaccurate repair make it incumbent on the surgeon to follow sound surgical principles in the management of these fractures.
Fractures of the zygomatic complex. Classification, etiology, pathogenesis, diagnostics and treatment. Complications of the zygomatic fractures
The zygomatic bone occupies a prominent position in the facial skeleton. It plays a key role in determining facial width as well as acting as a major buttress of the midface. Its anterior projection forms the malar eminence and is often referred to as the malar bone. The zygoma has several important articulations in the midface. From a frontal view, the zygoma can be seen to articulate with 3 bones: medially by the maxilla, superiorly by the frontal bone, and posteriorly by the greater wing of the sphenoid bone within the orbit. From a lateral view, one clearly can see the temporal process of the zygoma join the zygomatic process of the temporal bone to form the zygomatic arch. The zygoma is the main buttress between the maxilla and the skull; but in spite of its sturdiness, its prominent location makes it prone to fracture. The mechanism of injury usually involves a blow to the side of the face from a fist, object, or secondary to motor vehicle accidents. Moderate force may result in minimally or nondisplaced fractures at the suture lines. More severe blows frequently result in inferior, medial, and posterior displacement of the zygoma. Comminuted fractures of the body with separation at the suture lines are most often the result of high-velocity motor vehicle accidents. In general, displaced fractures will involve the inferior orbital rim and orbital floor, the zygomaticofrontal suture, the zygomaticomaxillary buttress,and the zygomatic arch. Occasionally, however, a direct blow to the arch will result in an isolated depressed fracture of the arch only. Attached to the zygoma anteriorly are the zygomaticus minor and major muscles, as well as part of the orbicularis oculi muscle. Laterally, the masseter muscle from below attaches to the zygomatic arch and produces displacing forces on the zygoma. Lastly, the branches of the fifth and seventh cranial nerves lie within the bounds of the midface. Particularly, the temporal and zygomatic branches of the seventh nerve and the zygomaticotemporal and zygomaticofacial branches of the fifth nerve must be identified carefully upon surgical dissection of the area to prevent complications of paresis and paresthesias, respectively.
The integrity of the zygoma is critical in maintaining normal facial width and prominence of the cheek.
Fracture lines usually run through the infraorbital rim, involve the posterolateral orbit, and extend to the inferior orbital fissure. The fracture line then continues to the zygomatic sphenoid suture area and on to the frontozygomatic suture line. Most zygomatic complex fractures involve the orbit, making visual complications a frequent occurrence.
A modern classification of zygomatic fractures is based on CT scan data. CT provides information about facial structures, including both bone segmentation and displacement, allowing for complete repair of the fractures. This system divides fractures into low-energy, medium-energy, and high-energy injuries.
Low-energy zygoma fractures result in minimal or no displacement. These types of fractures often are seen at the zygomaticofrontal suture, and inherent stability usually obviates reduction.
Middle-energy zygoma fractures result in fractures of all buttresses, mild-to-moderate displacement, and comminution. Often, an eyelid and intraoral exposure is necessary for adequate reduction and fixation (Fig. 15.11).
Fig. 15.11. Buttresses of the midface
High-energy zygoma fractures frequently occur with Le Fort or panfacial fractures. The zygomatic fractures often extend through the glenoid fossa and permit extensive posterior dislocation of the arch and malar eminence. A coronal exposure, in addition to the oral and eyelid incisions, usually is necessary to properly reposition the malar eminence (Fig. 15.12).

Fig. 15.12. Le Fort classification of the midfacial fractures
Although isolated zygomatic complex fractures occur, fractures of this nature are usually associated with other facial skeletal and soft-tissue injury.
Initially, assessment of a zygomatic fracture in an emergent setting should be directed at prevention of life-threatening complications including major bleeding, airway compromise, aspiration, and identification of other fractures. Cervical spine injury should always be considered if the injury is the result of a high velocity event or if the patient has altered mental status. Intracranial, thoracic, extremity, and pelvic injuries require proper evaluation and management.
Once other more pressing injuries have been dealt with and the patient is stable, a thorough preoperative assessment of facial skeletal architecture can be performed. Symptoms include paresthesias in the distribution of the maxillary branch of the trigeminal nerve, trismus, diplopia, and flattening of the zygoma.
Signs classically include subconjunctival and periorbital hemorrhage (Fig. 15.13) and hypesthesias in the distribution of the maxillary branch of the trigeminal nerve. Flattening of the malar eminence, lateral canthal dystopia, and reduction in mandibular movement may be present. Ipsilateral epistaxis and buccal sulcus hematomas may occur. Reduced extraocular muscle function, diplopia, and enophthalmos can occur secondary to orbital floor fractures, resulting in entrapment of orbital contents.

Fig. 15.13. Le Fort III Fracture
A thorough ophthalmologic examination is required to evaluate and document ocular status. If a ruptured globe, retinal detachment, or traumatic optic neuropathy exists, treatment of these supersedes repair of a zygomatic fracture.
Radiographic evaluation of the fracture is mandatory and may include both plain films and a computed tomographic (CT) scan. Computed tomography imaging (CT scan) with three-dimensional reconstruction is most commonly used to confirm the presence of a fracture and optimize pre-surgical planning (fig. 15.14, 15.15). If physical findings and plain films are not suggestive of a zygomatic fracture, the evaluation may end here. However, if they do suggest fracture, a coronal and axial CT scan should be obtained. The CT scan will accurately reveal the extent of orbital involvement, as well as degree of displacement of the fractures. This study is vital for planning the operative approach.

Fig. 15.14. CT-3D of the midfacial fracture

Fig. 15.15. CT scans of the Le Fort III fractures
Surgical treatment
Historically, closed reduction was the method of choice for nearly all zygomatic fractures. Multiple methods were employed, but most involved simply exerting pressure underneath the malar eminence and popping the fragments back into alignment. Closed reductions yield unpredictable results with significant chance of relapse. It was also frequently associated with complications including persistent diplopia, orbital dystopia, malunion, and significant residual deformity.
If a zygomatic fracture (Fig. 15.16–15.19, 15.21) is displaced , an open reduction and rigid stabilization with mini- and microplates is used. The floor of the orbit is routinely explored and reconstructed, if needed, to restore orbital volume. The complications of an inadequately or unreduced zygomatic fracture are very difficult to correct secondarily and usually avoidable.

Fig. 15.16. Fractures of zygomatic complex

Fig. 15.17. CT scans of zygoma fracture

Fig. 15.18. Treatment of maxillary fracture by external devices

Fig. 15.19. Temporary immobilization in midfacial fractures
While 2-point fixation of zygomatic fractures may be used commonly, it often leaves an axis of rotation for the zygoma following an adequate reduction. Forces such as the masseter muscle often displace the zygoma postoperatively. Thus, making the diagnosis and then choosing the correct approach to establish 3-point fixation and ultimate stability is essential for obtaining a successful outcome. Since biomechanical properties are of primary importance underlying the treatment of zygoma fractures, a brief discussion is warranted. In terms of postoperative stability of a reduced zygoma fracture, 3-point fixation is undoubtedly best. However, at times, 2-point stabilization is perfectly adequate.
Rigid fixation with plates and screws restores 3-dimensional stability and allows for the least amount of motion between ends of fragments, the main cause of bone resorption and instability.
Presently, several types of microplating systems made of titanium and biodegradable materials are available to choose from when rigid fixation is needed for stabilization.
In many situations, resorbable plates and screws are adequate. Such situations may include the presence of primarily compressive forces of relapse and sturdy bone fragments that can be fixed in direct contact, since forces of relapse are absorbed by bone fragments and not the fixation system.
Arch fractures resulting in decreased mandibular motility can be dealt with via a gillies temporal approach or by a limberg hook, incerted via a small infrazygomatic incision. The temporal approach allows for surgical reduction of a depressed zygomatic arch while leaving a well-camouflaged scar within the hairline. Dissection exposes the deep temporalis fascia followed by creation of a plane between the fascia and temporalis muscle. The lateral eyebrow incision of the supraorbital approach allows for additional access to the frontozygomatic suture line. A supraperiosteal dissection plane allows for access to the arch. Both approaches provide safe and direct access to the zygomatic arch, since the seventh cranial nerve lies above the dissection planes.
An instrument such a zygomatic elevator or hook is placed beneath the arch. Once the instrument is properly positioned, the arch is elevated in a superolateral vector taking care to not use surrounding facial bones as a fulcrum. Proper placement of the instrument can be confirmed with palpation by the surgeon’s free hand placed within the intraoral, posterior buccal sulcus. A cracking sound is heard when the convexity of the arch is restored with full reduction. The surgeon should be cognizant of the normal flattening of the middle of the arch. A persistent protuberance will occur if care is not taken not to avoid fracture overcorrection. The wounds are closed, and the patient is advised to avoid direct contact to the area for several weeks (Fig. 15.20).

Fig. 15.20. Reposition of the zygoma by Limberg hook

Fig. 15.21. Surgical approaches to the midfacial zone
Zygomatic complex fractures are usually repaired with open reduction and internal fixation. Plating systems are used to fixate the zygomaticomaxillary buttresses, zygomaticofrontal suture, and zygomatic arch. Osteotomies are indicated for fractures older than 1 month with onlay bone grafting for fractures present for 4 months or longer (Fig. 15.22; 15.23).
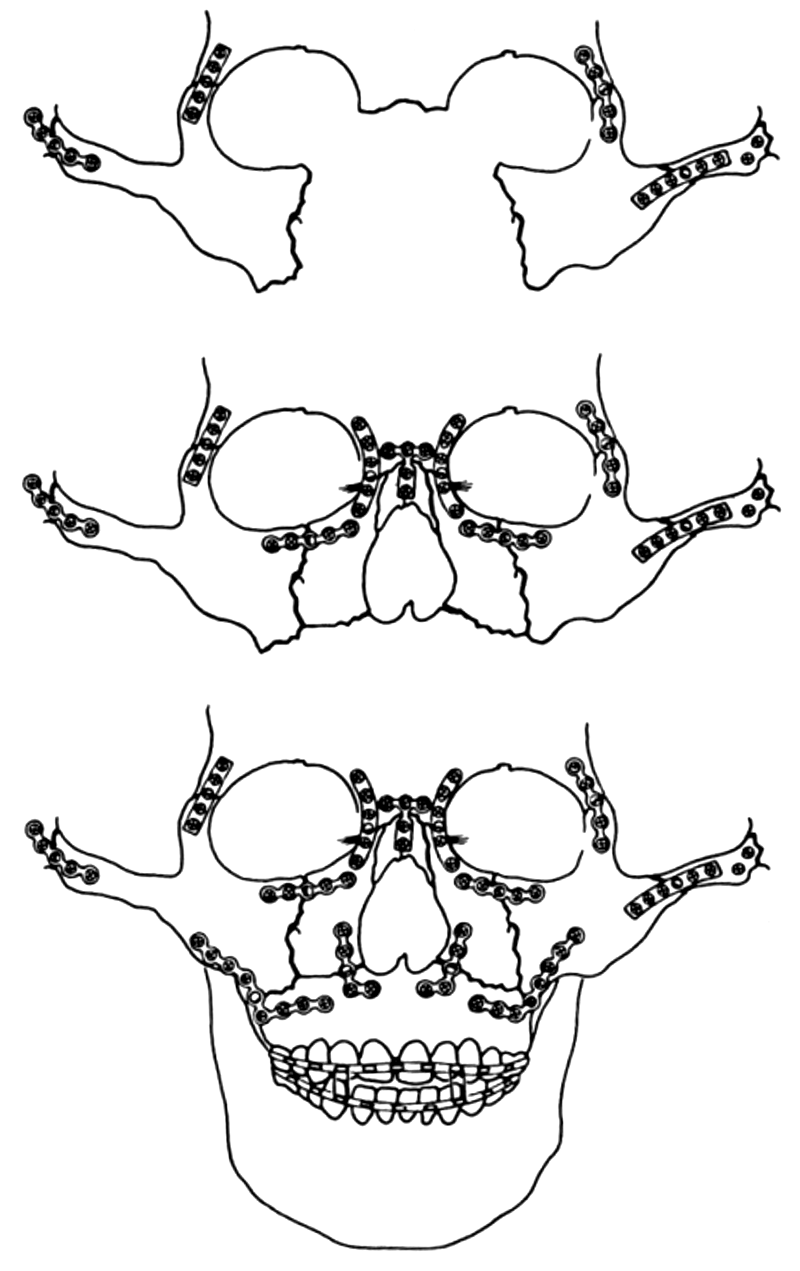
Fig. 15.22. Algorithm of the midfacial reconstruction

Fig. 15.23. Reconstruction of the zigomatic complex via coronal
approach
Various approaches to zygomatic complex fractures include coronal, eyebrow, upper eyelid, transconjunctival and infraciliary lower eyelid, and maxillary vestibular approaches. The approach to the zygomatic complex is dictated by the degree of injury and need for exposure for open reduction and internal fixation. In most instances, 2 areas of internal fixation are necessary to provide rigidity and satisfactory malar contour and eminence. The frontozygomatic suture and maxillary buttresses are the usual fixation points, with plating of the inferior orbital rim when reconstruction of the orbital floor is necessary.
Fractures of the zygomatic complex frequently result in sensory disturbances in the infraorbital nerve distribution. These symptoms include dysesthesia of the skin of the nose, cheek, lower eyelid, upper lip, gingiva, and teeth of the affected side. These arise because fractures generally occur in the vicinity of the infraorbital foramen and canal.
Trismus is also a common finding (45 %), particularly after a fracture involving the zygomatic arch. It results from impingement upon the coronoid process of the mandible by a depressed zygomatic arch. This may indicate a need for elevation of the depressed arch, accurate reduction, and fixation. If new bone has formed in the space below the zygomatic arch and restricts the movement of the mandible, an intraoral approach for coronoidectomy may be required to permit mandibular movement.
Diplopia may occur after zygoma fractures for numerous reasons. These include, but are not limited to, hematoma, muscle injury, motor nerve injury to the extraocular muscles, entrapment of extraocular muscles, or damage to the fine connective tissue system. Diplopia that occurs after zygoma fractures not associated with significant orbital floor fractures and entrapment is usually transitory and is probably associated with hematomas.
A symptomatic diplopia associated with a positive forced duction test and CT evidence of entrapped muscle or soft tissue with no improvement over 1–2 weeks may be an indication for surgery. When diplopia is associated with enophthalmos, an improvement in vision can be predicted after correction of the enophthalmos. Diplopia associated with zygomatico-orbital fractures may persist longer, and young patients may recover more slowly than adults.
Enophthalmos
A frequency of this complication is 3–4 %. The displacement of orbital contents into an enlarged bony orbit with subsequent change to a more spherical orbital soft-tissue shape is thought to be the principal underlying mechanism behind the development of enophthalmos.
The most common causes of enophthalmos include the failure to properly reduce displaced zygoma fractures and malunited zygoma fractures. Blowout fractures of the orbit, especially those of the medial wall and those.
Of floor fractures behind the axis of the globe, and high-velocity comminuted fractures involving combinations of lateral wall, posterior floor, and medial wall fractures are other causes of enophthalmos. Other theories of possible causes of enophthalmos include fat atrophy, soft-tissue contracture, and fibrosis.
Before surgical correction of enophthalmos, examine the patient to assess visual function, extraocular eye movement, and the sensory function of the infraorbital nerve. Both thin coronal and axial slices on ct scans are helpful in determining the extent of orbital damage.
Infection
While an infrequent occurrence, infection is a problem that threatens all postoperative patients. Sinusitis has been found to be the most common type of infection seen in postoperative patients; preseptal cellulitis and dacryocystitis also can occur.
Complications with plates and/or screws
The usual cause is a palpable plate, although a pain syndrome may occur. More rarely, infections may occur. Very rarely, screws can fracture into bone and create problems for removal.
These problems may be limited by a broad availability of drill sizes for use in thin or dense bone.
Regeneration of the bone tissue bone tissue
Bone is a rather unique tissue with many functions. All bones have a mechanical function providing attachment to various muscle groups. In addition, is some parts of the body, bones provide a protective function to vital structures – skull (brain), ribs (lungs, heart) and pelvis (bladder, pelvic viscera). Some bones retain their haemotopoetic function in adults – vertebrae, iliac crests, proximal parts of femur and humerus. All bones serve as a reservoir of calcium and actively participate in calcium homeostasis of the body.
Macroscopically, bones are two types:
- Cortical (compact) bone. With a dense outer layer – the cortex.
- Cancellous (spongy or trabecular) bone. Present in the interior of mature bones. This structure resists compression.
Bone as a tissue consists of two main types:
- Primary bone tissue (non-lamellar bone). This bone is also known as “coarse fibred” or “woven” bone or immature bone. It is characterized by the presence of randomly oriented coarse collagen fibres clearly visible by polarization microscopy. Non-lamellar (woven) bone is seen in the bone of fetuses and young children. It is the osseus tissue first deposited on the cartilage matrix in endochondral ossification. It is also the first tissue to appear in the repair of bone (facture healing).
- Secondary bone (lamellar bone). This bone is also known as mature bone. It is characterized by the presence of collagen fibres arranged in parallel layers or sheets (lamellae) readily apparent when viewed by polarization microscopy. Lamellar bone is present in both structured types of adult bone, cortical (compact) bone and cancellous (spongy or trabecular) bone.
Bone is a very specialized type of connective tissue consisting of cells and an intercellular matrix.
There are three cell types:
- Osteoblasts – the bone forming cells, located on the surfaces of bone lying side by side like a simple cuboidal epithelium. These cells are responsible for the synthesis of organic components of the bone matrix. When active, they show high alkaline phosphatase activity.
- Osteocytes – the cells occupying the lacunae in the bone matrix. They possess long thin cytoplasmic processes – the filopodia locsted in thin cylindrical spaces or canals in the bone matrix – the canaliculi. Nutrients and oxygen pass between the blood vessels and distant osteocytes by the arrangement of the canaliculi. Osteocytes also break down the bone matrix by osteocytic osteolysis to release calcium for calcium homeostasis.
- Osteoclasts – the large, multi-nucleated cells formed by fusion of monocytes. They lie in shallow depressions on the bone surface called the howship’s lacunae.
The bone matrix is composed of:
- Organic matter. Consisting of type I collagen fibres embedded in the ground substance containing proteoglycans and glycoproteins. The collagen fibres are made up of bundles of fibrils to resist pulling forces.
- Inorganic matter. Made up of stiffening substances to resist bending and compression. The bone mineral is an analogue of crystals of calcium phosphate – hydroxyapatite a substance that can only be seen under electron microscopy. It is this association of hydroxyapatite with collagen fibres which is responsible for the hardness of bone.
There are two type of histogenesis of bone namely intra-membranous ossification and endochondral ossification.
Intra-membranous ossification – this occurs in flat bones such us the skull and clavicle. In this process, the bone is developed from a condensation of mesenchymal tissue – the ossification centre. This tissue differentiates directly into osteoblasts which synthesise osteoid which then undergoes calcification.
Endochondral ossification – this type histogenesis occurs in long bones and short bones. The primary ossificution centre appears in the middle of the long bone and produced chondrocytes. The chondrocytes then undergo hypertrophy and the cartilage matrix undergoes calcification. The chondrocytes are then invaded by primitive mesenchymal cells and blood vessels to differentiate into osteoblasts and blood-forming cells and bone marrow.
Bone has 3 basic types of constrictors:
- Osteogenesis, the synthesis of new bone by the cells of the graft or cells of host origin, is primary. Graft bone cells usually survive initial transplantation if properly handled and have been shown to synthesize a new bone. The cancellous bone, with its surface area, has a greater potential for forming a new bone than does the cortical bone.
- Osteinduction is a second way in which a bone graft may function as a source of osteogenesis. Osteoinduction is the recruitment of mesenchymal stem cells that differentiate into osteoblasts from the surrounding bed. The recruitment and differentiation of these cells are modulated by low-molecular-weight peptides such as the glycoprotein, bone morphogenetic protein. Bone morphogenetic protein is a hydrophobic, nonspecies-specific protein extracted from the diaphysis of the cortical bone, dentin, and various bone-forming tumors.
- Osteoconduction is a term referring to the three-dimensional process of growth of capillaries, perivascular tissue, and osteoprogenitor cells of the host into the graft. The graft functions as a trellis or scaffold for the ingrowths of a new host bone.
Phases of fracture healing:
- Phase of inflammation.
- Phase of osteogenic repair tissue.
- Phase of remodeling.
Phase of inflammation. In this phase, also sometimes called the immediate reaction or the phase haematoma formation, bleeding occurring from the damaged bone ends adjacent soft tissue forms a haematoma between the bone fragments. This haematoma is essential for fracture healing to occur. The fibrin of the clot serves as a scaffold for fibrocellular invasion.
Phase of osteogenic repair tissue. The next phase consists of organization of the fracture haematoma. The haematoma becomes invaded by fibrovascular tissue replacing the clot laying down collagen fibres and matrix which later becomes mineralized to from the woven bone of provisional or primary callus.
In some cases, cartilage may form in the periphery of the callus.
There are two theories: osteoprogenitors cells and osteogenic induction.
Osteoprogenitors cells – repair tissue arises specialized cells with predetermined commitment to bone formation. Osteoprogenitor cells occur in close association with bone surface (cambial layer of periosteum) or with bone marrow.
Osteogenic induction – repair is due to activity of previously uncommitted fibroblasts (mesenchymal stem cells) which could develop the power of osteogenesis given the appropriate environmental stimulation by the phenomenon of osteogenic induction. There cells do not arise from the bone itself but from the adjacent surrounding soft tissue. Indeed, soft tissues play a key role in the healing of fractures. The fibroblasts in the soft tissue cannot be distinguished morphologically from osteoprogenitor cells of bone.
Phase of remodeling – once the fracture is bridged by bony callus of osteoid the newly formed bone must adapt to its new function. Remodeling occurs just as the process of replacement and repair goes on continuously in normal uninjured bone.
There is the modeling process occurring in the cortical bone which is quite different from that occurring in the cancellous bone. In remodeling the normal haversian system of osteons is developed from the initial less organized woven bone tissue. Remodeling is governed by wolff s law of functional adaptation of bone. The trabeculae realign themselves along directions of principal stress or strain to best protect them from bending. The end result is maximum structural support for minimum osseous structure.
In the cancellous bone, the cells are never very far away from the blood vessels. The whole process of bone apposition takes place on the surface of the trabeculae by the phenomenon of “creeping substitution”.
In compact bone, the presence of more deeply placed cells require the presence of haversian systems which must be replaced. Remodelling occurs in a more orderly sequence. First, the osteoclasts ream out a tunnel in the dead bone down which a blood vessel follows, bringing osteblasts which lay down the lamellar bone of a new osteon – osteoblastic “cutter head”.
Factors controlling fracture healing
Mobility. The amount of external callus formed is related to the amount of movement present, more mobility being associated with a larger amount of external callus producer. With such plating, the appearance of external callus reflects technical failure of fracture stabilization or fixation.
Cellular contact therapy. After two weeks, in the collars formed made no contact with each other, they undergo involution. It is the phenomenon limited in duration, is the primary callus response. With intact periosteum, the two collars readily establish contact. If the periosteum is disrupted, the two advancing collars may reach each other to from a purposeful bridge. Alternatively, if the developing collars are excessively separated by distraction of by interposition of soft tissue, cellular contact cannot occur and nonunion is produced. There is a subsequent stage in the process following the primary callus response – phase of external bridging callus with participation of induction mechanisms.
Mechanical influences. The “bioelectric phenomenon” described in 1957. It is whereby mechanical deformation of bone gave rise to electrical potential – “piezo-electric effect”. When a bone was fractured, the bone ends became more electronegative – associated with increased osteogenesis and advocated the non-invasive use of electromagnetic fields to promote fracture healing.
Humoral theory. Mechanical factors are not only stimulus in callus formation. Such factors cannot explain two points:
- The response to bridge fractures by external callus is not prolonged indefinitely.
- Continued mobility of the fracture does not cause continued callus response.
It is therefore postulates that there is a humoral inducing agent which plays a role in fracture healing – being present for only a limited period of time at the fracture site to induce osteogenesis.
At present, we are still unable to isolate the “wound hormone” that is released from the fracture ends. The exclusion of bone ends by silastic caps did not impair callus formation. The hormone is released most likely not from the injured bone itself but rather from the products of the primary response.
The humoral inducing agent is present only for a limited period of time at the fracture site to induce osteogenesis.
The formation of external callus can be considered to occur in two stages:
- An initial primary callus response, largely independent of environmental changes, arising from predetermined cells in bone tissue itself.
- A subsequent phase of bridging callus formation, the speed being dependent on the recruitment of cells from the surrounding tissues by the process of induction.
Medullary callus. It is distinguished from callus only by its location. Often cartilage formation is much less prominent in medullary callus. The second stage appears rather late in this healing process and the controlling factors involved appear to be quite different. Medullary callus is unaffected by effect of mechanical stability and often flourishes under these conditions.
Skeletal defects have been replaced by bony grafts for that 300 years. Autologous bone grafts remain the gold standard in bone transplantation. Autologous cancellous bone grafts contain hydroxyapatite and collagen as an osteoconductive scaffold while stromal cells have osteogenic potential.
Autograft:
- Healthy bone is harvested from the patient’s own body.
Advantage:
- No chance for rejection.
- Perfect biocompatibility, osteoinduction.
- Have stromal cells.
Disadvantage:
- Two surgeries are necessary.
- There is little “extra” bone to harvest.
- Works for small defect size in non-load bearing areas only.
One of the most challenging problems in surgery is the reconstruction of massive bone defects caused by resection of bone tumours, “gap nonunions” resulting from trauma and resection of genital pseudoarthroses. Options include the use of non-vascularised autologous bone transplant, free vascularised autologous bone transplant, allograft, bioceramics or prostheses. Non-vascularised autologous bone transplant are limited as to its availability in size, shape and amount and is therefore seldom used. Free vascularised autologous bone transplant is technically demanding and requires specialized expertise and facilities, incurring large costs and taking up long operating hours. Bioceramics is a simpler option but integration with the host bone is less ideal. A bigger disadvantage is that it is expensive. Allograft on the other hand is readily available, shows good osseo integration with the host bone and is relatively inexpensive. Allografts are therefore an attractive option provided they can be provided by a good tissue bank processing high quality bone allografts.
Allografts:
- Healthy bone is harvested from another source, either a donor or cadaver.
Advantage:
- Perfect biocompatibility, osteoinduction.
Disadvantage:
- Donors have little “extra” bone to harvest.
- Disease transmission is possible.
- High probability that the implant will be rejected.
Metals:
Advantage:
- Extremely high mechanical properties.
- Easily crafted and available in large quantities.
- Inert, thus no biological reaction to worry about.
Disadvantage:
- Poor implant-bone interface, leads to migration of failure.
- Mechanical attachment often destructive to patient.
- So strong they often erode surrounding “healthy” bone.
- Heavier than natural bone.
Ceramics:
Advantage:
- Extremely durable.
- Easily crafted and available in large quantities.
- Good implant-bone interface, osteoinduction.
- Many have similar chemical structure to actual bone.
Disadvantage:
- So durable they often erode surrounding healthy bone.
- Insufficient mechanical properties for load-bearing applications.
Chapter 16. Basics of craniomaxillofacial and plastic surgery
Surgical treatment of deformations
of maxilla and mandibule
The term orthognathic surgery refers to the surgical alignment of the jaws to achieve a functional skeletal base occlusal relationship and an optimum soft tissue balance of the lower half of the face.
Whereas orthodontics is used to correct the position of the teeth relative to the dental arch, orthognathic surgery aims to correct the position of the jaws relative to the cranial base. It is uncommon for orthognathic surgery to be performed without concomitant orthodontic treatment, because the surgical movement of the jaws relies to a great extent on the alignment and position of the teeth.
The most important role of orthognathic surgery lies in the management of malocclusions that harbor a gross jaw discrepancy between the mandible and maxilla. Therefore, the dentofacial deformity that orthognathic surgery aims to correct is often described in terms of the jaw size and position as opposed to simply in terms of the dental malocclusion.
Orofacial development
Orofacial development is genetically predetermined, so discrepancies in the size, shape, and morphology of teeth and jaws will readily reflect the orofacial form and pattern of the parents. Occasionally dentofacial deformities such as cleft lip and palate may be the result of environmental insults to the developing embryo that occur during crucial stages or periods of gestation. Generally speaking, fewer than 10 % of a given population will have dento-facial deformities that may benefit significantly from orthognathic surgery.
Orthognathic surgery must be tailored to the growth pattern of each individual. Most important, it must consider the growth potential of the patient and target those regions where growth is undesirable.
There are two phases in which orthognathic surgery may be undertaken:
- During the growth phase: This is considered interceptive surgery, whereby surgery is used to restrict unfavorable growth to minimize the degree of the subsequent dentofacial deformity. Unfavorable growth is defined as growth that is detrimental to the child’s health, psychosocial well-being, and development. Usually, but not always, a second surgical procedure is required at the end of the growth phase.
- After growth has ceased: In adulthood, orthognathic surgery may be considered definitive surgery.
Controversy exists as to whether some deformities can be treated early and others only after growth is complete. For example, it is not uncommon for mandibular horizontal deficiency to be treated during early adolescence, while mandibul ar horizontal excess will not be treated until well after growth is complete.
- Maxillary anteroposterior deficiency: Inadequate growth of the maxilla in an anterior direction in combination with a Class III malocclusion.
- Vertical maxillary excess: Overgrowth of the maxillary alveolus in the inferior direction, creating excess display of the teeth and gingivae and often associated with an incompetent lip seal without mentalis muscle strain.
- Vertical maxillary deficiency: Vertically short maxilla resulting in an edentulous appearance and a short lower face, often combined with mandibular deep bite and a prominent chin.
- Alveolar cleft: Usually associated with maxillary constriction in the anteroposterior and transverse dimensions.
Common dentofacial deformities
In the classification of dentofacial deformities, it is preferable to describe the skeletal relationship rather than simply the dental relationships, because orthognathic surgery is fundamentally used to correct the underlying skeletal base discrepancies.
Maxillary deformities:
- Maxillary anteroposterior excess: Protrusive maxilla in which there is an overgrowth in an anterior horizontal direction.
Mandibular deformities:
- Mandibular anteroposterior excess (hyperplasia): Prognathism combined with Class III malocclusion (Fig. 16.1).
- Mandibular anteroposterior deficiency (hypoplasia): Deficient anterior growth of the mandible combined with Class II malocclusion.
- Mandibular asymmetry: Usually related to unbalanced excess or lack of growth on one side of the mandible, often the condylar process, but sometimes involving the ramus and body. Malocclusion may be present, depending on the compensatory growth in the maxilla that may have occurred. It appears clinically as a chin and mandibular midline shift (lower facial asymmetry) (Fig. 16.4).

Fig. 16.1. Macrogenia in the vertical dimension, exacerbated by Class III mandibular prognathism
Chin deformities
Chin deformities are often associated with other mandibular deformities:
- Macrogenia: Overgrowth of the chin in the vertical or anterior direction.
- Microgenia: Chin deficiency in the vertical and/or anterior direction (Fig. 16.2).

Fig. 16.2. Chin deficiency in both the vertical and horizontal dimensions, exacerbated by Class II mandibular deficiency
Combined maxillary and mandibular deformitie
Short-face syndrome (brachyfacial pattern): Deficient lower facial growth in the vertical dimension, resulting in low mandibular and occlusal plane angles. It is usually the result of Class II malocclusion combined with mandibular anteroposterior deficiency but sometimes is caused by Class II malocclusion combined with vertical maxillary deficiency.
Long-face syndrome (dolichofacial pattern): Excess lower facial height, usually associated with increased occlusal and mandibular plane angles. It is often the result of a combination of vertical maxillary excess and mandibular hypoplasia. Apertognathia: Anterior open bite, often associated with long-face syndrome or simply increased posterior facial height. Lower facial asymmetry: Usually caused by unbalanced aberrant growth in the mandible (e.g., condylar hyperplasia). Alteration in the maxillary cant will only arise if problem emerges during early facial growth, whereby compensatory growth of the maxilla will occur in relation to the aberrant mandibular growth pattern (Fig. 16.3).
- Correction of underlying skeletal jaw disharmony.
- Development of a functional occlusion in which the teeth are in the most ideal position to aid stability and esthetics.
- Formation of a surgical plan with the best esthetic result that does not compromise occlusal or skeletal stability.
- Development of an optimal balance among esthetics, function, and stability. Esthetics should not be sacrificed at the expense of function, and, in most instances, an improvement in function will bring about an improvement in esthetics.

Fig. 16.3. Long-face (dolichofacial) appearance with anterior open bite and incompetent lip seal

Fig. 16.4. Lower facial asymmetry in which the maxilla is also canted to the right
Patient evaluation and diagnosis
Patient concerns
Determine the patient’s feelings about the existing problems and his or her expectations for treatment results.
Clinical evaluation:
- Facial form (frontal and profile): Long, short, convex, concave, flat.
- Relationship of facial thirds (Fig. 16.5, 16.6): The face can be divided into equal thirds (only approximately), from the hairline to the eyebrows; from the eyebrows to the base of the nose; and from the base of the nose to the chin point. Facial proportionality can be assessed by comparing the middle and lower thirds of the face to determine where the face may be long or short.

Fig. 16.5. Facial proportions in a – profile and b – frontal views. The lower third of the face can be further subdivided into thirds from the base of the nose to the chin point

Fig. 16.6. Smile line, occlusal cant, and dental midlines in relation to the facial midlines
Relationship of soft tissues to dentition: Smile line, occlusal cant, and dental midlines versus soft tissues.
Vertical and horizontal radiographic measurements (Fig. 16.7, 16.8):
- Vertical dimensions: Essential to assessing vertical jaw dimensions in relation to the upper face which, in turn, will determine whether maxillary surgery or genioplasty is warranted.
- Horizontal angles: The horizontal lines that run through key radiographic landmarks are measured as angles with respect to the Frankfort horizontal line, which forms the main reference mark. High or low occlusal and mandibular plane angles will often determine whether maxillary surgery is warranted.
- Transverse dimensions: Important in determining whether segmental jaw surgery is required.
- Intra-arch dimensions: Important in determining if dental extractions will be required prior to presurgical orthodontics.

Fig. 16.7. Vertical measurements of facial height and proportion: (ADH) anterior dental height; (ULL) upper lip length; (LLL) lower lip length; (UF) upper facial height; (LF) lower facial height

Fig. 16.8. Horizontal plane angles: (CB) cranial base; (FH) Frankfort horizontal; (Pal) palatal plane; (Occ) occlusal plane angle; (MPA) mandibular plane angle. All angles are measured with respect to the FH plane, which is the main reference mark
Radiographic analysis
Cephalometric analysis: Lateral and anteroposterior cephalograms are used to undertake cephalometric analysis of the jaw positions and dimensions with respect to the upper face and cranial base. These measurements provide the reference base for determining whether the jaws are malpositioned, too large, or too small. The patient’s lips must be in repose and the teeth should be only lightly touching and in centric relation when the cephalogram is taken.
Panoramic radiograph: This is used to check for the position of the inferior alveolar canal and screen for gross pathology and impacted teeth.
Dental study casts:
- Accurate bite registration: Use of a facebow is indicated in two-jaw surgery.
- Two-jaw surgery requires duplicate casts.
- Trimmed or mounted casts should match the degree of discrepancy observed in the lateral cephalogram.
Other issues
Speech, audiometry (especially for cleft patients), psychological conditions, medical conditions (e.g., diabetes and bleeding disorders).
Sequence of treatment
- Dental and periodontal treatment:
- Maintain as many of the teeth as possible.
- Stabilize the periodontium prior to orthodontic and surgical intervention.
- Extractions:
- Facilitate orthodontics (e.g., premolar extractions).
- Facilitate subsequent surgery: Mandibular third molars must extracted 9 to 12 months prior to sagittal split osteotomy, or the lingual cortex will be weakened.
- Presurgical orthodontics:
- Position the teeth over their respective basal bone.
- Align and level the teeth.
- Adjust for tooth size discrepancies.
- Correct rotated teeth.
- Ensure divergence of roots adjacent to surgical sites, especially with segmental maxillary osteotomies.
- Coordinate maxillary and mandibular arch widths: Correct transverse discrepancies without compromising stability and dental health, or further surgical options must be considered.
Different dentofacial patterns respond very differently to treatment:
- Brachyfacial (short-face) pattern: Flat mandibular plane in which growth tends to proceed horizontally. Best to use a nonextraction technique.
- Dolichofacial (long-face) pattern: Steep mandibular plane angle in which growth tends to proceed vertically. More likely to use an extraction technique.
Where skeletal form is unfavorable, dentoalveolar segments will compensate. Therefore, most of these dental compensations must be corrected prior to surgery, by positioning teeth in their ideal axial relationship to their respective skeletal bases.
- Orthognathic surgery:
- Reposition the basal bone and/or dentoalveolar segments into more normal interrelationships.
- Provide the best functional and esthetic results and provide stability of the achieved results.
- Surgical preparation involves:
- Final STO tracing.
- Model surgery and construction of the surgical occlusal wafers.
- Postsurgical orthodontics:
- Finalize tooth alignment and root parallelism.
- Ensure maximal interdigitation.
- Create ideal overbite and overjet.
- Ensure that centric occlusion is the same as centric relation.
It may take up to 10 months to fine tune the final occlusion while the bones and muscles continue to heal and adapt to the repositioning, depending on the accuracy of the preoperative setup of the occlusion.
Where rigid internal fixation is used, orthodontics can resume anywhere between 2 and 6 weeks postsurgery. The teeth and osseous segments can move very rapidly during the first few months postoperatively; therefore the orthodontist should initially examine the patient on a frequent basis (every 1 to 2 weeks) for adjustments so that rapid changes can be closely monitored. A good presurgical orthodontic setup will help to simplify the surgery, improve the stability and occlusion, and decrease the amount of postsurgical orthodontics required.
Mandibular surgery
Orthognathic surgical procedures of the mandible are classified according to the design of the osteotomy and the region where the surgery is undertaken: body or ramus. An osteotomy is a bone cut, whereas an ostectomy involves the removal of bone.
Classification
Ramus procedures:
- Condylotomy (subcondylar osteotomy).
- Condylectomy.
- Sagittal split ramus osteotomy.
- Vertical subsigmoid osteotomy.
- Inverted L-osteotomy.
- C or arcing osteotomy.
Body procedures:
- Anterior to mental foramen:
- Step osteotomy/ostectomy.
- Midline symphyseal osteotomy.
- Posterior to mental foramen:
- Y ostectomy.
- Rectangular ostectomy.
- Trapezoid ostectomy.
- Inverted V-ostectomy.
Subapical body procedures:
- Anterior:
- Kole osteotomy.
- Combined with midline symphyseal osteotomy.
- Posterior.
- Total.
- Mandibuloplasty.
Genioplasty:
- Genioplasty is described in detail in a later section.
Sagittal split ramus osteotomy
The techniques most commonly performed to move the mandible are the sagittal split ramus osteotomy and the vertical subsigmoid osteotomy. The vertical subsigmoid osteotomy only allows for setback of the mandible, while the sagittal split osteotomy allows anterior repositioning (advancement) and posterior repositioning (setback).
The sagittal split ramus osteotomy continues to be the most versatile and most commonly used technique of all mandibular osteotomies. The direct bone contact between the sliding fragments ensures stability and good healing between the bone segments in advancement, setback, and even rotational procedures.
Trauner and Obwegeser (1957)
They described a horizontal cut just above the mandibular foramen on the medial side of ramus, a vertical cut down the anterior border of the ramus, and an oblique cut made through the lateral cortex toward the angle of the jaw. It was a good technique for mandibular setback but provided poor bone contact with mandibular advancement. Aseptic necrosis of the angle of the mandible was a problem because of extensive stripping of the pterygomasseteric sling.
Dal Pont (1961)
Dal Pont modified the sagittal split by advancing the oblique cut toward the molar region and making the vertical cut through the lateral cortex. The main problem with setbacks was interference between the main retropositioned proximal fragment and the mastoid process, where occasional pressure on the facial nerve could occur as well.
Hunsuck (1968)
Hunsuck shortened the cut through the medial cortex of the ramus by extending it only as far as the mandibular foramen, which prevented the occasional shattering of the ramus in mandibular setbacks.
Bell and Schendel (1977) and Epker et al (1978). In this modification, in the anterior vertical cut, the whole of the lower border is sectioned through and through. The split is kept more laterally by directing fine osteotomes down the inner surface of the lateral cortex to produce easier splitting and greater protection for the inferior dental nerve. Blood supply to the ramus is preserved, because the need to strip the pterygomasseteric sling is eliminated.
Surgical procedures
Incision:
- Commence mucoperiosteal incision at the lateral crest of alveolus.
- Extend the incision up the anterior border of the ramus/ coronoid process and anteriorly along external oblique ridge as far forward as the first molar.
Dissection:
- Create subperiosteal exposure laterally over the body of the mandible to the lower border.
- Dissect medially just beyond the lingula and superiorly to expose the coronoid process.
Osteotomy (Fig. 16.9):
- Lingual cortex of ramus: Make the cut from the anterior border of the ramus, passing backward to just reach superiorly and posteriorly to the lingula.
- External oblique ridge: Make cuts down along the anterior border of the ramus, medial to the external oblique ridge, and then forward to about the second molar.
- Vertical cut: Cut the lateral cortex of the body down to and through the lower border of the mandible.

Fig. 16.9. Sagittal split ramus osteotomy: a – osteotomy sites for the sagittal split shown in grey; b – intraoperative view of the vertical cut in the buccal cortex
Split:
- Begin from the lower border of the vertical cut and then insert fine osteotomes along the alveolar cut to gently pry the two fragments apart.
- The neurovascular bundle must always lie on the medial side in the distal segment; if it does not, reposition it to that side.
Fixation options:
- Upper or lower border transosseous wires: Require a 4- to 6-week period of maxillomandibular fixation.
- Bicortical screws (Fig. 16.10): These are inserted transbuccally in a triangular or linear fashion via the trochar and cannula. The best biomechanical advantage is obtained with three screws placed in a triangular pattern. Disadvantages associated with this fixation technique include the requirement for a facial stab incision, the potential for direct damage to the teeth and inferior alveolar nerve, the torquing of condyles, and the difficulty in removing the fixation screws after healing.
- Monocortical plates and screws (Fig. 16.11): One or two plates may be used and placed transorally. It is much easier to remove hardware at a later date.
- Postoperative care.
- Drain tubes are optional and often unnecessary.
- If wire fixation is used, maxillomandibular fixation is required for 4 weeks.
- If screw fixation is used, maxillomandibular fixation is unnecessary, but training elastics are useful for a few weeks to help guide the occlusion.

Fig. 16.10. (grey shaded area) Exposed marrow space of a mandible that has three bicortical screws placed in a triangular pattern, which is been advanced with a sagittal split ramus osteotomy. One method of fixation of the sagittal split mandibular osteotomy

Fig. 16.11. Placement of miniplates and monocortical screws: a – the most common position of the plate is on the upper border of the osteotomy site, and at least two monocortical screws are placed on each side of the osteotomy; b – miniplates and monocortical screws are easy to place through the transoral approach
Limitations
Relapse is common in cases of:
- Anterior open bite: It is not appropriate to use sagittal split alone, particularly with short ramus height, in which case the inverted L-osteotomy is better suited. The sagittal split osteotomy may be used in conjunction with maxillary osteotomy.
- Mandibular asymmetry: Relapse is more likely to occur if there is rotational movement of the proximal fragment, particularly with setbacks. Rotational movements predispose to poor contact between the fragments; careful trimming minimizes angle flaring.
- Large advancements (more than 8 mm): Occasionally the sphenomanibular ligament prevents large advancements of the mandible and may need to be stripped off the lingula.
- In the presence of a thin or abnormal ramus structure, it is better to use an inverted L-, a C-, or an arcing osteotomy.
- The split is occasionally unpredictable.
Vertical subsigmoid (or ramus) osteotomy (Fig. 16.12)
Indications
Developed by Caldwell and Letterman in 1954, the vertical subsigmoid osteotomy has regained popularity in recent years because of the reduced potential for surgical trauma to the inferior alveolar nerve, particularly with mandibular setback procedures:
The procedure is mainly used for setback procedures and mandibular asymmetries.
It is not recommended for correction of anterior open bites.
It cannot be used for advancements.
It is used mainly for setback procedures when potential damage of the inferior dental nerve has to be minimized because of patient concerns.
- Maxillomandibular fixation is required for 6 weeks postoperatively.

Fig. 16.12. Vertical subsigmoid mandibular ramus osteotomy: a – osteotomy sites shown in red; b – intraoperative view of the proximal fragment of the ramus after the osteotomy and outward repositioning of the proximal segment using a periosteal elevator
Surgical procedures
Extraoral approach (unusual cases only):
- The easiest and safest method is to utilize the Risdon (submandibular) approach.
- Strip the whole lateral surface of the ramus of periosteum and masseter muscle.
- Reflect the medial pterygoid muscle insertion off the deep surface.
- Insert a Rayne subsigmoid retractor with fiber-optic light attachment.
- This approach has some disadvantages:
- External scar.
- Occasional damage to the mandibular branch of the facial nerve.
Transoral approach:
- This has become a more popular approach since the introduction of specially designed retractors, oscillating saws, fiber-optic illumination, irrigation, and suction.
- Submentovertex radiographs may occasionally help to assess the amount of outward flaring of the rami in order to establish feasibility of the transoral approach, because the more parallel the rami, the less direct vision is available to the surgical sites.
Make an extended third molar incision up the anterior border of ascending ramus and forward to the first molar, similar to the sagittal split osteotomy incision. Extensive muscle stripping from ramus may result in aseptic necrosis of the bone fragment and condylar sag. However, if inadequate muscle stripping occurs, there is an increased risk of relapse. Bell et al (1980) recommend that medial pterygoid muscle not be stripped off because it maintains the blood supply to the proximal fragment and helps keep condyle in place, although some (Welch 1989) believe this leads to greater relapse.
Begin the osteotomy halfway, first up and then down from the sigmoid notch to the angle, using an oscillating saw with a 120-degree blade angle. The depth of the cut should be no greater than 6 mm to avoid the risk of damage to medial tissues.
Identify the position of lingula by looking for a small bony thickening on the lateral surface of the ramus. Make a vertical bone cut a few millimeters posterior to this landmark; the cut should have a slight oblique angle anteroposteriorly. Set back the mandible so that the proximal fragment overlaps the distal fragment on the outer aspect. Lateral surface decortication may be required on the distal fragment to establish good bony contact and healing and on the proximal fragment to prevent deformity at the angle. Trimming of the angle from the proximal fragment may also be necessary to prevent flaring.
Transosseous fixation may or may not be used, although Epker and Wolford (1980) advocated wiring to ensure that the condyle is carefully seated in the fossa. Where setbacks are greater than 1 cm, a coronoidectomy may be necessary to prevent excessive tension on the temporalis muscle.
Establish maxillomandibular fixation, which remains for 6 weeks.
Genioplasty
The term genioplasty describes the numerous surgical techniques used to alter the size and morphology of the bony chin with concomitant changes in the surrounding soft tissues. Otherwise known as mentoplasty, chin surgery is commonly combined with other orthognathic surgical procedures. Although about 15 % of all dentofacial deformities primarily involve the chin, 85 % of the clinical changes associated with a maxillomandibular osteotomy and chin surgery are the result of the genioplasty. In other words, the genioplasty contributes more to the overall clinical changes in the facial appearance than does the movement of both jaws.
Historical review
In the past, most surgical chin procedures involved the use of alloplastic implants for augmentation. In 1942, Hofer described the osteotomy of the anterior lower border of the mandible via an extraoral submental incision. In 1957, Trauner and Obwegeser described the intraoral approach, or labial sulcus incision, to the osteotomy of the anterior mandibular lower border.
Applied anatomy
The chin is a region of the lower face that consists of bone and soft tissue elements. The bony chin is basically the mental protuberance, bounded by the mental tubercles superiorly, the mental foramina laterally, and the lower border of the anterior mandible interiorly. In chin surgery, the following are the most important structures:
- Mental nerves (foramen): Provide major sensory innervation of the chin.
- Mentalis muscles: Indirectly provide the major vertical support to the lower lip in addition to chin posture.
- Lingual muscle pedicle: Provides the major blood supply to the osteotomized segment of the chin and hence maintains viability of the bone and prevents resorption.
- Root apices of the mandibular incisors: Root apices must be identified and osteotomy cuts must be designed at least 5 mm below the apices.
Chin deformities
These may be esthetic (e.g., macrogenia) or functional (e.g., chin ptosis). Chin deformities may occur in isolation but are more commonly associated with other dentofacial deformities:
- Functional deformities (commonly iatrogenic):
- Chin ptosis.
- Lower lip incompetence.
- Esthetic deformities:
- Macrogenia (large chin):
- Vertical.
- Horizontal (anteroposterior).
- Combination of vertical and horizontal.
- Microgenia (small chin):
- Vertical.
- Horizontal (anteroposterior).
- Combination of vertical and horizontal.
- Asymmetry.
Transoral genioplasty procedures
Approach. Labial sulcus: Make an incision in the lip, 1 cm forward of the sulcus depth.
Dissection:
- Transect the mentalis muscle.
- Expose, isolate, and protect the mental nerves bilaterally.
- Maintain soft tissue attachment at the inferior border of the mandible.
- Horizontal osteotomy.
- Place the osteotomy at least 5 mm below the root apices of the mandibular incisors.
- There are numerous osteotomy designs:
- Horizontal osteotomy: most commonly used.
- Double horizontal osteotomy: for large advancements.
- Tenon and mortise osseous genioplasty.
- Sagittal osteotomy (Thompson, 1985).
- Horizontal-vertical step osteotomies.
Downfracture and repositioning:
- Always maintain an attached, broad-based lingual muscle pedicle to the osteotomized bony chin segment.
- By virtue of its simple anatomy and surgical versatility, the osteotomized chin may be repositioned in any of the three dimensions or directions: the horizontal, lateral, and vertical planes.
Fixation options:
- Transosseous wires.
- Bone plates and screws.
- Lag screws.
Closure:
- Restore mentalis muscle continuity.
- Close in two layers.
- Apply a light pressure dressing.
- Chin implants are placed in a subperiosteal pocket and often are not fixed by any means apart from the surrounding soft tissue pressure that holds them in place.
Genioplasty types Functional genioplasty. (Fig. 16.13)
First described by Michelet and Jacquet in 1973, it is used to correct abnormal mentalis muscle activity at an early age by surgically altering the underlying chin bone deformity:
- Indications:
- Vertical chin excess requiring vertical reduction genioplasty.
- Horizontal (anteroposterior) chin deficiency requiring advancement genioplasty.
- Timing: usually just after the eruption of the mandibular canines.
Augmentation genioplasty:
- Alloplastic onlay grafts: various materials, including hydroxyapatite.
- Biologic onlay grafting: allogeneic or autogenous bone (prone to resorption).
- Horizontal advancement osteotomy.
- Vertical downgraft osteotomy with interpositional graft.
- Lateral expansion: midline osteotomy with outward rotation of the genial segments.

Fig. 16.13. Various genioplasty procedures involving an osteotomy of the anterior mandible: a – advancement using a horizontal sliding osteotomy; b – setback using a horizontal sliding genioplasty; c – vertical augmentation using an interpositional graft. Fixation is not shown but can involve plates with monocortical screws or lag screws alone
Reduction genioplasty:
- Shave (osteoplasty) of the chin protuberance: high incidence of lower lip ptosis.
- Horizontal sliding osteotomy and setback.
- Vertical reduction osteotomy with wedge ostectomy (bone removal).
- Lateral reduction with midline ostectomy for broad-based chins.
Asymmetric genioplasty.
Asymmetric genioplasty is the vertical shift of the genial segment (propeller-type genioplasty).
Maxillary surgery
The maxilla may be moved as a whole or in segments in any combination of horizontal and vertical directions. This is achieved with a Le Fort I maxillary osteotomy that is approached by a circumvestibular incision in the labial sulcus. The Le Fort I osteotomy is still the most versatile technique for maxillary osteotomies and is the most widely used technique in orthognathic surgery involving the maxilla.
Cheever (1867).
As reported by Maloney et al in 1981, a Boston surgeon performed the first Le Fort I maxillary osteotomy for access to a nasopharyngeal tumor.
Cohn-Stock (1921).
He described the first anterior maxillary osteotomy to correct ananterior open bite.
Wassmund (1927).
Reported in his 1935 textbook, he performed a Le Fort I maxillary osteotomy to correct an anterior open bite. The maxilla was only partially sectioned from its bony attachments but not mobilized at the time of surgery. Maxillomandibular elastic traction was used postoperatively to close the open bite.
Axhausen (1934).
He was the first to advance a maxilla at the Le Fort I level that was incompletely mobilized at the time of operation; postoperative elastics were used.
Schuchardt (1942).
To prevent impairment of the vascular supply to the maxilla, a two-stage procedure was devised. The second stage involved separation of the maxilla at the pterygoid plates. Postoperatively, weights hung from an overhead traction device were used to advance the maxilla.
Gillies and Harrison (1950).
They performed the first Le Fort III osteotomy in 1941; the procedure was later made routine by Tessier in 1971.
Converse etal (1952).
They advanced the maxilla by means of a transverse palatal cut at the junction of the palatine and maxillary bones.
Bell (1969 to 1975).
Experiments on adult rhesus monkeys established the scientific basis for the safety of Le Fort I downfracture osteotomy with full mobilization under direct vision.
Obwegeser (1969).
He described a very high-level Le Fort I osteotomy whereby interpositional bone grafts were placed in the pterygoid plate region to aid stability in large advancements. Obwegeser also advocated the use of simultaneous Le Fort I and Le Fort III procedures.
Kufner (1970); Henderson and Jackson (1973).
These surgeons described various approaches to the Le Fort II osteotomy.
Bennett and Wolford (1985).
They developed the Le Fort I step osteotomy, which allowed bone cuts to be made parallel to the Frankfort horizontal plane.
Classification
Osteotomies of the maxilla may either be segmental, in which case only a segment of the dental arch is mobilized, or total, in which case the whole maxillary arch is mobilized.
Segmental maxillary surgery (Fig. 16.14):
- Single-tooth osteotomy.
- Corticotomy.
- Anterior segmental osteotomy:
- Wassmund (1935).
- Wunderer (1963).
- Epker and Wolford (1980).
- Posterior segmental osteotomy:
- Schuchardt (1959).
- Kufner (1971).
- Horseshoe osteotomy:
- Wolford and Epker (1975).

Fig. 16.14. Posterior segmental osteotomy and ostectomy: a – palatal view of the osteotomy and extraction of the first premolar; b – lateral view showing the extraction of the premolar in order to move the posterior segment forward to improve the occlusal molar relationships; c – posterior maxillary osteotomy used to interiorly reposition the posterior alveolar segment to close a posterior open bite; d – resultant gap above the segment that is usually bone grafted to enhance stability
Total maxillary surgery
There are many osteotomy techniques and designs that involve the movement of the whole maxillary arch in all three dimensions of space relative to the cranial base. They range from low-level Le Fort I osteotomies to subcranial Le Fort III osteotomies and everything between. The following is a list of some of the midfacial osteotomies involving the whole maxillary dental arch that have been described in the literature over the last half century:
Le Fort I osteotomy:
- Classic downfracture: Bell (1969 to 1975).
- Surgically assisted maxillary expansion: Buttress release.
- Quadrangular: Keller and Sather (1990; Fig. 16.15) Le Fort I osteotomy.
- Anterior Le Fort II osteotomy: (Fig. 16.16)
- Pyramidal Le Fort II osteotomy: Henderson and Jackson (1973; Fig. 16.17).
- Quadrangular Le Fort II osteotomy: Kufner (1971).
Le Fort III osteotomy (Fig. 16.18):
- Gillies (1940s).
- Tessier (1971).
Other midfacial osteotomies:
- Zygomatic osteotomies.
- Malar-maxillary osteotomy: Obwegeser (1969); malars attached as wings to maxilla (Fig. 16.19).
Bezrukov V. (1976) proposed method of surgical treatment of upper retrognathia with the modification of Le Fort osteotomia (Fig. 16.21). Malanchuk V. (1995) proposed method of surgical treatment of upper micro- and retrognathia which allows to remove retroposition of maxilla and narrow alveolar arch simultaneously during operation (Fig. 16.20).

Fig. 16.15. Quadrangular or high-level Le Fort I osteotomy

Fig. 16.16. Anterior Le Fort II osteotomy. Technically, this is a segmental maxillary osteotomy involving only the anterior arch, but the procedure is included here as part of the range of Le Fort II osteotomies

Fig. 16.17. Pyramidal Le Fort II
osteotomy

Fig. 16.18. Le Fort III orbital floors osteotomy that involves the nasal bridge and anterior

Fig. 16.19. Malar-maxillary osteotomy, a variation of a high Le Fort I osteotomy in which the malar buttresses are attached as wings

Fig. 16.20. Scheme of osteotomia of maxilla by V. Malanchuk

Fig. 16.21. Scheme of osteotomia of maxilla by V. Bezrukov
Basic principles of segmental maxillary surgery
Surgical repositioning of small dentoalveolar segments is possible, provided that maximal palatal and labiobuccal mucoperiosteal attachments are maintained. The design of bone and soft tissue incisions should aim for the largest possible dento-osseous segment to preserve the greatest amount of soft tissue pedicle. Inadvertent injury to cementum in the midportion of a tooth frequently heals without problem. However, inadvertent apicectomy of teeth may initiate progressive pulpal necrosis and fibrous degeneration resulting in devitalization, despite pulpal and osseous revascularization.
Le Fort I maxillary osteotomy
The Le Fort I maxillary osteotomy is the most versatile and most commonly used orthognathic surgical procedure involving the maxilla and will therefore be described in more detail.
Bell et al (1969 to 1975) laid the biologic foundations for the safety of the Le Fort I downfracture osteotomy. Using 14 adult rhesus monkeys, they undertook microangiographic and histologic studies of healing at various time intervals after total maxillary osteotomy. They found only transient vascular ischemia, minimal osteonecrosis, and early osseous union.
Their results demonstrated:
- As long as the maxilla is pedicled to palatal mucosa and labiobuccal gingivae and mucosa, there are adequate nutrient pedicles required for Le Fort I downfracture and maxillary viability.
- Segmentalization, stretching of vascular pedicles, and transection of the descending palatine vessels have no discernible effect on revascularization or bone healing associated with Le Fort I osteotomies.
The work of Bell and colleagues permitted technical advances in total maxillary surgery, such as allowing full mobilization of the maxilla, hence reducing the risk of relapse, and permitting bone surgery under direct vision.
Surgical procedures (Fig. 16.22–16.27):
- Make a buccal incision a few millimeters beyond the sulcus, into the upper lip, extending from first molar to first molar. Previous palatal surgery may compromise palatal blood supply to the segmented maxilla, in which case vertical incisions and subperiosteal tunneling should be used instead.
Locate a Le Fort I – level osteotomy at least 5 mm above the apices of the:
- Straight-line osteotomies create a ramping effect, so that simple advancements also decrease the vertical height.
- The step osteotomy (Bennett and Wolford, 1985) allows horizontal bone cuts to be made parallel to Frankfort horizontal, permitting horizontal maxillary movements without altering vertical dimensions; hence, ramping effects are minimized:
- Anterior cuts: 4 to 5 mm
above the canine apices
- Vertical cuts: zygomatic buttress region (excellent site for bone grafts)
- Posterior cuts: 4 to 5 mm above the molar apices Perform an osteotomy of the lateral nasal walls and nasal septum.

Fig. 16.22. Exposure of the right maxilla through an incision in the buccal sulcus a few millimeters beyond the attached gingiva: a – illustrated view; b – intraoperative view. Note the periosteal elevator inserted in the lateral nasal wall

Fig. 16.23. Horizontal osteotomies made at the Le Fort I level. The osteotomies should be located at least 5 mm above the apices of the maxillary teeth, in particular the canine teeth, which have the longest roots. Note the slight downward inclination of the bone cuts as they progress posteriorly

Fig. 16.24. Downfracture of the maxilla: a – separation of the maxilla from the midface; b – intraoperative view of the downfractured maxilla

Fig. 16.25. Downfracture of the maxilla using a large bone hook

Fig. 16.26. Use of Rowe disimpaction forceps to help downfracture and fully mobilize the maxilla from its attachments

Fig. 16.27. Miniplate and monocortical screw fixation of a Le Fort I osteotomy:
a – illustrated view; b – intraoperative view
Separate the pterygomaxillary junction:
- First advocated by Axhausen in 1934 by use of the curved osteotome.
Complications of unfavorable dysjunction in this region include:
- Excessive bleeding.
- Cranial nerve injury.
- Carotid artery injury.
- Unfavorable fracture.
Completely mobilize and trim the maxilla:
- Ensure that the maxilla can sit passively in the new position.
- Remove the pyramidal strut of bone surrounding the descending palatine arteries to allow posterior impaction (Johnson and Arnett, 1991).
- Carefully trim the lateral nasal walls and septum.
Provide fixation:
- Use 2-mm adaptational bone plates and monocortical screws to fix the maxilla in the desired position.
- Use two or four plates (Fig 16.28a), although two may be adequate for small movements.
- For advancements greater than 5 mm and downgrafts,stability and healing are greatly facilitated by interpositional bone grafts (Fig 16.28b), especially in the buttress region (placed under direct vision) and pterygomaxillary junction (placed blindly behind the maxilla).

Fig. 16.28. A gap of more than 4 to 5 mm in the osteotomy site requires i the repositioned maxilla an interpositional bone graft to fill the gap and thereby improve the stability
Surgical occlusal wafer/splint:
- In maxillomandibular surgery, two splints are required:
- The intermediate splint helps to guide the final position of the maxilla before it is fixed. The final splint guides the new position of the mandible.
- Wire the final splint to the maxillary teeth only if segmental maxillary surgery is performed.
Applications
With the establishment of the scientific basis for the various orthognathic surgical techniques, it has become possible to apply these procedures to the treatment of the numerous dento-facial deformities. As already mentioned, the most commonly used orthognathic surgical techniques are the Le Fort I down-fracture for the maxilla and the ramus osteotomy techniques for the mandible, in particular the sagittal split and the vertical sub-sigmoid osteotomies. This section will discuss the application of these most commonly used orthognathic surgical techniques for the management of the more common dentofacial deformities.
Common procedures
The most commonly performed orthognathic surgical procedures involve the movement of the jaws in any one or combination of the following directions relative to the cranial base.
Maxillary surgery:
- Vertical:
- Superior repositioning (impaction).
- Inferior repositioning (downgraft).
- Horizontal:
- Anteroposterior (advancement).
- Transverse (expansion).
Mandibular surgery:
- Horizontal (anteroposterior):
- Vertical (autorotation): Vertical changes in the maxilla often give rise to the following vertical movements of the mandible without surgery in the mandible itself:
- Clockwise: results in decreased chin projection.
- Counterclockwise: results in greater chin projection.
Maxillary (Le Fort I downfracture) procedures
Maxillary impaction (superior repositioning)
Indications.
Vertical maxillary excess:
- With open bite.
- Without open bite.
Esthetics:
- Deformity mainly in the vertical facial balance (long-face [dolichofacial] pattern).
- Relatively long lower third of the face.
- Lip incompetence with excessive exposure of the teeth and gingivae.
- With open bite: excessive eversion and exposure of the lower lip at rest.
- Without open bite: excessive tooth display and narrow alar base of the nose.
- Profile:
- Nasal prominence.
- Marked interlabial distance.
- Recessive chin, especially in patients with open bite.
Occlusion:
- Class II malocclusion.
- V-shaped maxillary arches.
- Open bite: maxillary crowding with posterior crossbites.
- Cephalometric features.
- Large lower facial height resulting from long posterior facial height Relative mandibular retrognathia and high mandibular plane angle.
Treatment planning:
- Ideal maxillary incisal exposure is 2 to 3 mm (Burstone, 1967) from stomion to incisal tip.
- With maxillary impaction, the upper lip moves 1 mm (20 %) for every 5 mm of superior repositioning of the anterior teeth.
- With maxillary impaction, the mandible rotates counterclockwise, which:
- Shortens the lower face.
- Makes the chin more prominent.
Surgical procedures:
- Vertical maxillary excess without open bite: One-piece maxillary osteotomy with careful trimming of bony interferences that may prevent the maxilla from seating passively in a superior position (e.g., pyramidal bony release around descending palatine artery).
- Vertical maxillary excess with open bite (see the section on open bite): Differential impaction of the maxilla, which may also require maxillormandibular surgery. Segmental maxillary surgery may be required to correct the transverse maxillary problem. Impaction of greater than 5 mm may require a horseshoe osteotomy to minimize the decrease in the nasal airway.
Maxillary downgraft (inferior repositioning)
Indications:
- Vertical maxillary deficiency: short-face (brachyfacial) pattern.
- Maxillary atrophy resulting from a prolonged edentulous state.
Esthetics:
- Poor incisal display even on smiling with the eversion of the lower lip.
- Diminutive anterior dentoalveolar height in both arches.
- Occlusion.
- Usually Class I but sometimes Class II malocclusion with dental crowding.
- Deep anterior overbite.
- Wide maxilla.
Cephalometric features:
- Negative incisal display with normal anteroposterior positioning of the maxilla.
- Square jaw with low, almost parallel, mandibular and occlusal plane angles.
- Prominent pogonion and labiomental fold.
Surgical procedures:
- Perform interpositional bone grafting for all downgrafting procedures. Bone grafting is essential because of the inherently high relapse rate of downgrafting.
- Aim for overcorrection with greater than 3 mm of incisal display.
- Maxillary downgrafting increases lower facial height and rotates the chin downward and backward as the occlusal and mandibular plane angles are increased.
- Position the maxilla slightly posteriorly to fit the occlusion if mandibular surgery is not planned.
Maxillary advancement Indications.
Anteroposterior maxillary deficiency (maxillary hypoplasia):
- Without cleft palate.
- With cleft palate.
Esthetics:
- The nasolabial angle is reduced.
- If the nasal bridge cannot be seen in profile because the eye (globe) protrudes beyond it, then the maxilla most likely needs an advancement at a higher level osteotomy.
- Maxillary incisal display is inadequate.
- The prominent everted lower lip is indicative of mandibular prognathism or maxillary hypoplasia.
- Nasal balance: Important preoperative measures include the nasal tip, nasolabial folds.
Occlusion:
- Class III malocclusion.
- Severe maxillary dental crowding.
- Constricted maxillary arch with posterior crossbites.
Velopharyngeal function:
Velopharyngeal function is of particular concern in cleft patients with short palates, because maxillary advancement may well accentuate velopharyngeal incompetence. If there is a strong risk of postoperative velopharyngeal incompetence, maxillomandibular surgery should be considered to minimize the amount of maxillary advancement required for esthetics and occlusion.
Surgical procedures:
- Place interpositional bone grafts within osteotomy gaps:
- For maxillary advancements greater than 5 mm.
- In difficult cleft cases.
- Use bone grafts:
- To accelerate bone healing between segments.
- To serve as physical stop for increased stability and to minimize relapse.
- Completely mobilize the maxilla until it can be passively placed in the desired anterior position.
Cleft lip and palate patients. Simultaneous maxillary expansion and grafting of alveolar clefts is readily achieved with properly designed soft tissue flaps.
- For patients with complete clefts, mobilize the greater and lesser segments of the maxilla independently; alternatively, bone graft the alveolar cleft defect at least 6 to 12 months before maxillary advancement if a single-piece maxillary osteotomy is required.
- Mobilization of the maxilla is difficult because of:
- The perpendicular plate of palatine bone.
- Scar tissue between the palate and nasal septum secondary to previous palatal surgery.
- The presence of a pharyngeal flap.
- Indications and features.
- Transverse maxillary deficiency (bilateral or unilateral), either isolated or with a Class III malocclusion.
- Narrow maxilla with dental crowding.
- Few facial or cephalometric features that are of any practical use for diagnosis.
Treatment planning:
- Children: They can be successfully treated with orthopedic rapid maxillary expansion.
- Adults:
- For less than 5 mm of transverse deficiency, orthopedic expansion of maxilla is sufficient.
- For greater than 5 mm of transverse deficiency or buccally inclined posterior teeth, a combined surgical-orthodontic expansion technique is used.
Combined surgical-orthodontic expansion. There are three surgical options:
Segmental posterior alveolar osteotomy, used for unilateral deficiencies.
Le Fort I downfracture with midline palatal split or horseshoe osteotomy.
Surgically assisted rapid maxillary expansion: Complete a Le Fort I osteotomy without the downfracture. Make a midline palatal split between the maxillary central incisors with a fine osteotome. Intraoperatively, activate an orthopedic expansion device that is bonded to the posterior maxillary teeth across the palate.
Mandibular (ramus osteotomy) procedures
Mandibular advancement
Deficiency in the anteroposterior direction:
- The chin and mandible are retruded.
- There is crowding in the mandibular anterior arch, with overangulated incisors and accentuated curve of Spee.
- This is corrected by mandibular advancement with ramus osteotomies, such as sagittal split ramus osteotomy Deficiency in the vertical dimension.
- The mandibular anterior dental height may be less than 40 mm.
- Sometimes the mandible appears clinically short but the actual problem is a deep overbite. This is best corrected by vertical lengthening of the chin by interpositional graft and augmentation.
- Deficient ramus height may be best treated with an inverted L-osteotomy and interpositional bone graft.
- Deficiency in the transverse dimension. This is corrected by body or symphyseal osteotomies or by subapical osteotomies to allow expansion of the arch.
Mandibular setback
Excess in the anteroposterior direction.
Mandibular prognathism is present and mandibular incisors are lingually inclined.
There is a Class III malocclusion with anterior and bilateral posterior crossbites:
- Presurgical orthodontics often worsens the appearance as teeth are uprighted over basal bone prior to surgery.
- This is usually treated with mandibular setback achieved via ramus osteotomies such as the sagittal split or vertical subsigmoid osteotomies.
Excess in the vertical dimension:
- Mandibular anterior dental height is increased.
- Reduction genioplasty is required.
- Excess in the transverse dimension.
- The mandibular dental arch is too wide in comparison to a normal maxillary arch.
- Arch width can be reduced by body and symphyseal ostectomies. Specific deformities.
Orthognathic surgery has a pivotal role in the management of the following common dentofadial deformities:
- Anterior open bite.
- Crossbite.
- Lower facial asymmetry.
Open bite
Clinical presentation.
In open bite, teeth in opposing jaws fail to contact each other.
Etiology:
- Anterior open bite: tongue thrust, thumb sucking, deficient eruption of anterior teeth and/or excessive eruption of the posterior teeth, skeletal base growth discrepancy (e.g., excessive posterior facial height, severe mandibular retrognathia, short ramus height, or long-face syndrome), condylar resorption: idiopathic, avascular necrosis.
- Posterior open bite: deficient eruption of posterior teeth, facial asymmetry that develops after growth is completed (e.g., condylar hyperplasia).
Classification:
- Dentoalveolar, skeletal base, combined dentoalveolar and skeletal base.
Management:
Management depends on the cause of the open bite:
- Discourage adverse habits such as thumbsucking or finger sucking with a variety of oral appliances, which will sometimes lead to spontaneous resolution of the open bite.
- Tongue thrust during swallowing will create forces large enough to result in open bite. The role of surgical reduction of the tongue as an adjunctive measure to the surgical-orthodontic management of anterior open bite is controversial. Assess the tongue size, morphology, and function in terms of:
- True macroglossia: excessively large tongue.
- Relative macroglossia: normal-sized tongue confined within a restricted oral space of relatively small dental arches.
- Functional macroglossia: excessive tongue activity.
- Segmental orthognathic surgery is especially useful in cases of infraeruption or supraeruption of the teeth; the dentoalve segment can be surgically repositioned anywhere in the vertical plane to close the open bite:
- Directly: Use an anterior subapical mandibular osteotomy with superior positioning to close an anterior open bite.
- Indirectly: Use a posterior maxillary osteotomy with impaction, which will bring the anterior segments together and close the anterior open bite.
- Total maxillomandibular orthognathic surgery can be used to surgically correct the problem of open bite caused by a skeletal base discrepancy:
- Mandibular body osteotomies and ostectomies are especially useful in the correction of a mandibular occlusal.
- Mandibular ramus osteotomies usually involve a counterclockwise rotation to close the open bite; this is often quite an unstable procedure with significant potential for relapse. The technique is mainly used for patients with mandibular retrognathia in whom maxillary surgery is also planned.
- Le Fort I maxillary osteotomy: Differential impaction of the whole maxilla yields a stable result and directly addresses the problem of increased posterior facial height. This is probably the most favored treatment option.
Crossbite
Clinical presentation
Crossbite is a reverse buccal overjet relationship of the teeth in opposing jaws:
- It may occur unilaterally or bilaterally.
- It can occur anteriorly or posteriorly.
- It is commonly related to a hypoplastic maxilla in patients with a Class III skeletal base malocclusion.
- It is also found in patients with lower facial asymmetry.
Etiology:
Crossbites are most frequently related to a transverse deficiency of the palatal vault or maxillary alveolar arch.
Treatment:
- Orthodontics: Tip or torque the teeth buccally. The results may be unstable if the transverse discrepancy is greater than 5 mm.
- Skeletal: Increase the width of the of the palate via:
- Palatal expansion devices during the growth phase.
- Surgically assisted rapid maxillary expansion: Use a combination of surgical relief of maxillary bony abutments and palatal expansion devices to rapidly open the midpalatine suture in a space of a few weeks.
- Segmental maxillary surgery: Make a midpalatal osteotomy at the time of the Le Fort I maxillary down-fracture to immediately expand the palate to the desired dimension in one step.
- Segmental posterior maxillary osteotomy may be used for unilateral deficiencies or crossbites.
Lower facial asymmetry
Clinical presentation
Lower facial asymmetry is usually related to unbalanced, aberrant growth of one side of the face; the aberrant growth often occurs in the condylar process of the mandible, but sometimes the ramus and body may be involved:
- Malocclusion may be present, depending on the compensatory growth in the maxilla.
- Alteration in the maxillary cant will only arise if the problem emerges during early periods of facial growth, whereby compensatory growth of the maxilla will occur in relation to the aberrant mandibular growth pattern.
- Clinical asymmetry results in a chin and mandibular midline shift (lower facial asymmetry) (Fig. 16.29).

Fig. 16.29. a – Lower facial asymmetry, b – corrected with maxillomandibular surgery and genioplasty
Etiology:
- Aberrant condylar growth:
- Condylar hyperplasia.
- Condylar hypoplasia.
- Condylar aplasia.
- Aberrant mandibular growth:
- Hemimandibular elongation.
- Hemimandibular hypertrophy/hyperplasia.
- Hemifacial atrophy (Parry – Romberg syndrome).
- Hemifacial microsomia (Goldenhar syndrome).
- Hemifacial hypertrophy.
- Traumatic deformities:
- Condylar fractures.
- Mandibular fractures (particularly of the ascending ramus).
- Neoplastic and other diseases of the facial skeleton:
- Neurofibromatosis (von Recklinghausen disease).
- Bone neoplasms (eg, osteoma, osteosarcoma, or osteochondroma of the condyle).
- Fibrous dysplasia.
- Odontogenic tumors.
- Large cystic lesions of bone (eg, odontogenic keratocyst).
- Temporomandibular joint (TMJ) ankylosis (unilateral, arising during growth).
This section will discuss facial asymmetry caused by growth aberration rather than by disease, because orthognathic surgery does not address the disease process but only the consequences of the growth anomaly.
Clinical examination:
All normal individuals have a certain degree of facial asymmetry. Assess mainly the frontal view and start from the top, looking for obvious differences between left and right sides:
- Cranial vault (eg, plagiocephaly).
- Forehead: unilateral flattening or excess.
- Eyes: intercanthal and interpupillary levels.
- Malar prominences.
- Nose: level of alar bases.
- Lips: level of commissures.
- Chin point: deviation from midline.
- Dental midlines:
Investigations:
- Serial photographs: over a period of time to establish whether asymmetry is progressive or static.
- Radiographs:
- Diagnostic: use of cephalometric analysis on anteroposterior and lateral cephalograms as well as TMJ radiographs to determine the focal cause of the asymmetry (e.g., hyperplastic condyle).
- Radioisotope bone scans to determine sites of active bone growth.
- Three-dimensional computed tomographic scan reconstructions.
- Biopsy: when a disease process is suspected rather than just aberrant growth
- Treatment planning.
- Determine the side and site of the abnormal growth and where the compensatory growth has occurred.
- Eliminate all disease processes prior to undertaking any corrective surgery.
- Often the underlying skeletal abnormalities must be corrected before any soft tissue procedures. It sometimes may be necessary to undertake tissue expansion in deficient regions prior to the bony surgery.
- Aim not only to correct the site of aberrant growth but also to eliminate any compensatory growth that may have occurred.
- In growing children, functional appliance therapy is of immense value, particularly in those with mild lower facial asymmetry.
In patients with mild asymmetry, in the presence of a functional occlusion and unrestricted mandibular movements, orthognathic surgery is best confined to a camouflage genioplasty.
In the presence of a maxillary occlusal cant, make an esthetic judgment, based on incisal display, as to whether to impact the maxilla on the excess side or downgraft the maxilla on the deficient side, regardless of where the aberrant or compensatory growth lies.
Timing of corrective surgery:
- Early surgery (during the growth phase):
- It will stimulate development of a functional occlusion through the creation of a proper interocclusal relationship at an early age.
- It will stimulate soft tissue development on the affected side.
- Early esthetic and functional improvement has a positive psychologic effect on both the parents and the child.
- Delayed surgery (after growth is completed):
- It avoids possible untoward effects of early surgery on subsequent facial growth.
- It avoids the difficulty in predicting final facial form that arises if early surgery is planned.
- It provides a more predictably stable result with less likelihood of multiple procedures.
Distraction osteogenesis
Distraction osteogenesis (DO) is a technique in which new bone is created through physical stretching of a developing callus between two bony ends that have been osteotomized or fractured. As the two bony fragments are gradually separated (distracted), the resulting gap is filled with an expanding callus that eventually develops into new bone (osteogenesis). DO has been touted as an alternative to conventional osteotomies.
Historical review
The first report of bone lengthening by gradual distraction was published in 1905 in the orthopedic literature (Codivilla, 1905), but it was many decades before the concept attracted the attention of llizarov, a Russian orthopedic surgeon. Ilizarov is credited as the pioneer in the development of DO, especially in the treatment of limb deformities. It was not until the 1970s, however, that the idea of using the DO technique in the jaws emerged with animal studies (Snyder et al, 1973; Michel)) and Miotti, 1977).
Tairov U. (1982) proposed the surgicaly-orthopedic method of distraction of mid-face zone.
After another hiatus of more than a decade, McCarthy and coworkers (1992) published a report of the first clinical application of DO for the management of congenitally hypoplastic mandibles in children. The publication brought to light the possibility of treating very young children with severe and disfiguring facial deformities without the need for conventional osteotomies. As interest in DO gradually gathered momentum during the 1990s, bold predictions were made that DO would eventually replace all conventional osteotomies, even in adult patients.
Surgical procedures
- Select the site of the osteotomy.
Make an incomplete bone cut through the cortex only. Fix the distraction apparatus across the osteotomy site with bone plates and screws.
Complete the osteotomy and ensure that free and unobstructed movement of the bone fragments on both sides of the osteotomy is possible.
To allow time for the initial callus to develop, do not commence distraction by a screw-type apparatus until 5 to 7 days following the osteotomy.
Thereafter, have the patient activate the screw device twice daily to achieve a distraction (callus-lengthening) rate of 1 mm per day until the desired length is achieved. Leave the distraction apparatus fixed in place for a further 2 to 3 months until the distracted callus has fully mineralized into new bone before removing the device.
Clinical applications
The fundamental fuel that drives the interest in the distraction technique is the concept of new bone growth, which in itself is a startling medical breakthrough. DO has been applied to the following situations.
Mandibular lengthening
Mandibular lengthening was the first application for DO, and presently myriad devices, both intraoral and extraoral, are available on the market. Despite the obvious advantages of the intraoral devices, the external devices are making a slow comeback, because the complex three-dimensional vectors of distraction required to lengthen a hypoplastic mandible cannot be adequately addressed with the simpler intraoral devices.
Mandibular widening at the symphysis
Symphyseal widening can be used in combination with ramus-body distraction devices to lengthen and widen the mandibular arch at the same time. Some researchers have raised the concern that widening of the mandibular arch may torque the condyles and result in TMJ pain and dysfunction. Clinical experience has so far failed to show any significant detrimental effects of DO on the TMJs.
Alveolar augmentation
Distraction techniques are also gaining popularity for the augmentation of alveolar ridges both in width and height to facilitate the placement of dental implants. Distraction is an alternative to the conventional onlay bone grafts and sandwich or visor osteotomies used in the past.
Palatal expansion
Palatal expansion using orthodontic appliances is a well-known technique that has been utilized for many decades. The introduction of surgically assisted rapid maxillary expansion has enabled palatal expansion to be undertaken in adult (nongrowing) patients. Palatal expansion techniques were the earliest form of DO, which predated the pioneering mandibular lengthening devices of the early 1990s.
Midfacial distraction
Midfacial distraction devices such as the RED system and Modular Internal Distraction system (Stryker) are designed to advance the midface at various levels, from low Le Fort I to high Le Fort III and beyond to fronto-orbital levels. As with the mandibular devices, attempts to make the midfacial devices almost fully implantable beneath the skin have met with the problem of uniplanar directional control. To address the three-dimensional vector requirements, the RED system, which has a fully adjustable external frame, permits multidirectional vectors of advancement of the midface; in particular the maxilla. The biggest drawback is the unsightly head frame.
Mandibular resection and distraction
Mandibular resections are also amenable to the technique of DO. The technique involves the creation of a transporter segment of bone that is osteotomized a few millimeters from the edge of the resection margin and distracted across the resection defect with an expanded callus following behind it.
Advantages
DO has a number of essential advantages compared with conventional osteotomy techniques:
- It eliminates the need for bone harvesting from remote donor sites.
- It allows gradual expansion of the surrounding soft tissue envelope.
- It may provide better stability than conventional osteotomies (yet to be proven).
- A much greater degree of bone lengthening can be attained.
- Surgical morbidity is lower.
- Operating time is reduced.
Disadvantages
The biggest disadvantage of DO is the distraction device itself:
Expensive hardware is required.
The metallic hardware protruding through the mouth, face, scalp, or neck is unsightly and uncomfortable.
Exposed hardware will draw unwanted attention.
There may be an increased potential for ascending infection via exposed hardware into the osteotomy site (not yet proven).
External devices result in pin-tract scarring of the skin.
A high level of patient compliance is required in terms of daily screw activation and meticulous hygiene.
The vector of lengthening (distraction) is difficult to control because of the three-dimensional nature of the maxillofacial skeleton. Mandibular distraction often results in anterior open bites unless due diligence is taken in the proper positioning of the device.
A second surgery is required to remove the device at the completion of treatment.
Complications
The evolution of surgical techniques and instrumentation and the introduction of new technology (e.g., miniature bone plates and screws and bone substitutes) have contributed to the improved safety and predictability of orthognathic surgery. Complications associated with orthognathic surgery can be divided into several categories.
Preoperative complications
- Poor communication:
- Surgeon.
- Orthodontist.
- Patient: unrealistic expectations.
- Incorrect diagnosis:
- Insufficient clinical data.
- Lip and mandibular posturing.
- Errors in radiographic measurements.
- Unsatisfactory laboratory work:
- Incorrect bite registration.
- Poor-quality surgical wafers or splints.
- Poor patient preparation:
- Unsatisfactory presurgical orthodontics.
- Inadequate medical history and examination.
- Poor workup of medically compromised patients (including psychiatric patients).
Intraoperative complications:
- Hemorrhage:
- Poor surgical technique.
- Awkward anatomy.
- Nerve injury:
- Neuropraxia.
- Axonotmesis.
- Neurotmesis.
- Unfavorable osteotomy:
- Poor design.
- Poor surgical technique.
- Jaw malpositioning:
- Soft tissue interferences.
- Bony interferences.
- Poorly constructed surgical splints.
- Improper seating of condyles.
- Inadequate surgical reference markings.
- Fixation problems (especially with bicortical screws):
- Direct injuries to tooth roots.
- Direct injuries to the inferior alveolar nerve.
- Excessive torque on condyles.
Postoperative complications
Acute phase (less than 2 weeks):
- Wound dehiscence.
- Hemorrhage:
- Reactionary.
- Secondary.
- Infection.
Chronic phase (more than 3 months):
- Relapse:
- Relapse is the propensity for the jaws to revert back to their original, preoperative position after surgery.
- Magnitude of movement: Any single jaw movement greater than 8 to 10 mm is potentially likely to relapse.
- Direction of movement: Maxillary downgrafts and counterclockwise rotation of the mandible are inherently unstable.
- Type of fixation: Rigid fixation with plates and screws is more stable than wire fixation because of three-dimensional control of fragments.
- Latent growth (age of patient): Class III mandibular setbacks in growing adolescents are highly likely to relapse.
- Condylar resorption: Patients with Class II skeletal relationships, steep mandibular plane angles, and preexisting TMJ symptoms are most likely to suffer condylar resorption following mandibular advancement procedures.
- Neurologic dysfunction:
- Persistent paresthesia or anesthesia lasting more than 6 months.
- Dysesthesia.
- Poor esthetics:
- Lip imbalance.
- Nasal base problems: excessive alar width, upturned tip, or nasal asymme try caused by an unsupported anesthetic tube that buckles the nasal septum.
- Soft tissue of the chin-throat angle.
- Poor bone healing:
- Delayed union.
- Nonunion.
- Inadequate fixation:
- Loose.
- Annoying.
- Exposure and infection.
- Unhappy patient:
- Poor esthetic result.
- Unrealistic expectations.
- Psychiatric issues:
- Depression.
- Dysmo rphobia.
Prevention and management
Prevention of most complications can be achieved through proper preoperative preparation and planning. Good presurgical orthodontic alignment of the teeth will help simplify the surgery and therefore minimize the likelihood of complications. Identifying problems before they occur eliminates the unwelcome surprises that often lead to unnecessary delays and a protracted course of treatment. Communication among the surgeon, the orthodontist, and the patient should be nurtured and maintained at all times to effectively produce a treatment plan that satisfies all parties concerned.
Response to a problem is a matter of the training, experience, attitude, and approach of the individual clinicians concerned. Maxillomandibular (two-jaw) surgery with rigid fixation and appropriate bone grafting are often effective measures that help to reduce the likelihood of relapse. Problems tend to arise when clinicians fail to recognize the merits and limitations of each of the treatment options, such as trying to close an anterior open bite with a mandibular osteotomy alone. A broad-minded attitude and sensible approach to problem solving are indispensable traits every surgeon must acquire during the protracted course of surgical treatment
Facial reconstructive surgery. Skin grafts and flaps.
Principles and techniques for local plastics
Few procedures are more challenging than the surgical repair of patients with craniomaxillofacial deformities and defects. They are the end results of the trauma, cancer, infection, or congenital anomalies. These defects may involve both bone and overlying soft tissue. No matter how subtle a deformity is, it will more than likely be quite obvious when involving the cranio – maxillofacial region.
Regardless of the etiology, surgeons must direct their repair toward the correction of the aesthetic defect with the restoration of function.
When treating patients who have undergone tumor resection or suffered severe facial trauma, both the surgeon and the patient must understand that the patient most likely will never function or appear as they did prior to their trauma or tumor surgery. The difficult task for the craniomaxillofacial surgeon is not the surgical correction of the deformity, but the basic understanding of the deformity’s nature.
As with all patient interviews and examinations, the information obtained during the initial assessment will be the first insight into the patient’s general health and mental readiness regarding their surgical treatment. This information should be clearly recorded and readily accessible to all those involved in the patient’s treatment. At this point, the surgeon’s feelings toward the accuracy and reliability of the history and information obtained should be stated. Was the patient or informant confused, cooperative, and was there a language barrier? Psychosocial problems that may pose potential problems regarding the surgery and its final outcome should be identified early in the patient interview if possible. In the adolescent and adult patient, the surgeon should try to identify who is the driving force regarding the chief complaint (i.e., the patient, family members, or friends). This information will again reflect the psychosocial status of the patient and family and should be noted because missed signals at this point may cause problems for the treating surgeon when patients enter treatment with unrealistic or misconceived expectations.
A variety of medical conditions are commonly associated with craniomaxillofacial deformations and defects. In planning for the surgical correction of craniomaxillofacial deformities, medical risk factors that contraindicate general anesthesia and surgical reconstruction must be identified.
Clinical assessment of facial defects from the esthetic point of view is a rather complicated process.
Dating back to ancient civilizations, many attempts have been made to establish a set of standards for facial beauty. Mathematicians have also attempted to calculate and quantify facial measurements to distinguish what is beautiful and what is not, but these calculations can be complex and difficult to interpret. However, it was Leonardo da Vinci who felt that anatomic relationships were more valuable than absolute numerical values. His studies furnished important data upon which many modern concepts of facial beauty are based. He divided the face into equal thirds and noted that these divisions should be relatively equal and symmetric. Therefore, the clinical examination should begin with the general assessment of symmetry and deformity in the frontal and profile views.
In the study of facial harmony, symmetry is one of the most obvious yet most critical concepts to appreciate. The aesthetic face requires reasonable symmetry. When planning a surgical procedure (either reconstructive or cosmetic), the surgeon must have symmetry as a primary goal.
Balance among different aesthetic units of the face also plays a very important role in creating facial harmony. The facial units that should be systematically studied preoperatively include the forehead, nose, eyes, malar prominences, lips, chin, and mandibular angles.
Over the past 50 years the development and application of several different flaps has led to reliable reconstruction of facial defects. Most defects can be reconstructed immediately, leading to better restoration of form and function with early rehabilitation.
Commonly there is a wide range of options for repairing a given defect, including healing by secondary intention, primary closure, placement of a skin graft, or mobilization of local or regional tissue. Compared to skin grafts, local flaps often produce superior functional and esthetic results.
When deciding which option to use, there should be a progression from simple to complex treatments. Consideration should be given to primary closure or the use of skin grafts first, followed by local, then regional, and finally distant pedicled or microsurgical free tissue transfer. Flaps require additional incisions and tissue movement, which increase the risks of postoperative bleeding, hematoma, pain, and infection. Confirmation of tumorfree margins should be done prior to flap reconstruction if a malignant lesion has been excised.
Some defects are amenable to closure with a single flap, but others require a combination of flaps for optimal results. An advantage of using multiple flaps is that they can be harvested from separate esthetic units. This decreases the size of the secondary defect and may allow placement of scars between esthetic units, thus improving scar camouflage leading to better cosmesis. Often, separated repair of individual facial subunits with separate flaps provides a better cosmetic result than if a single flap is used to reconstruct the entire defect.
Skin grafts
A skin graft may be defined as an intact piece of the skin that has been completely separated from its donor site attachment and is transferred to a different recipient site.
At this site, it reestablishes a new blood supply. A full-thickness skin graft is an intact piece consisting of the entire epidermis, complete thickness of dermis, with no connection to subcutaneous fat. A split-thickness skin graft consists of the entire thickness of epidermis, a varying thickness of dermis, and no connection to the underlying subcutaneous fat. Composite grafts consist of intact skin, both epidermis and dermis, with an additional component such as fat or cartilage directly attached.
Full-thickness grafts offer several advantages over split-thickness grafts. Full-thickness grafts have less tendency to contract, their cosmetic appearance is generally better and improves with time; they are more durable, there is a better chance for texture and thickness match. At the same time grafting creates a defect of a donor site that must be repaired, graft failure, there is a chance of unfavorable appearance, contracture along free margins, as well as potential surgical complications at two sites. A clean, well-vascularized recipient bed is also necessary for full-thickness grafts.
Survival of transplanted skin is primarily dependent upon reestablishing blood supply to ischemic tissue. The phases of graft vascularisation are: plasma imbibition, inosculation, and capillary ingrowth. The phase of serum imbibition occurs during the first 24 to 48 h after skin graft transplantation. During this time, the graft survives by taking up nutrients from the wound exudate.
The phases of inosculation and capillary ingrowth are characterized by the host endothelial buds’ “hooking up” to existing arterioles and venules present within the graft. These vascular buds grow through the fibrin layer. Thus the graft is revascularized from ingrowth of new vessels from the margin and base of the recipient bed. Actual blood flow is on 5 to 7 day after an operation. The speed at which vascularization occurs depends primarily on the vascularity of the donor site and on graft thickness.
Full-thickness skin grafting is a useful technique for resurfacing and reconstructing various surgical defects. Selection of a full-thickness graft to resurface a defect depends on various factors. Local factors to be considered are defect size, location, lack of adequate adjacent tissue, and mobility. Tissue quality factors such as injured tissue, underlying medical disease, adjacent hair-bearing skin, and heavy smoking may all adversely affect local tissue transfer. Irradiated skin typically is also of poor quality with compromised vasculature. In certain anatomic areas, grafts may provide a better cosmetic result than flaps. Sites frequently used for full-thickness grafts include the distal nose, ear, lower eyelid, and inner canthus.
A variety of donor areas exist for free skin grafts. It is necessary to match the qualities of the donor skin and the surrounding recipient area. Texture, color, and actinic damage vary from donor site to recipient site and should be matched if at all possible. Most full-thickness grafts are harvested from the preauricular skin, postauricular skin, supraclavicular and clavicular areas, neck, and inner upper arm areas. The groin, hypothenar area, and wrist are less frequently used.
It is important to measure and size the graft correctly. This should include the depth of the defect. A template is ideal to ensure exact sizing. An imprint of the defect is made, cut out along the blood-tinged paper, and placed over the donor area for marking.
Removal of the donor graft is performed with standard surgical technique. After the graft is incised, a tip of the graft is grasped, and with sharp and blunt dissection the graft is removed. Next, hemostasis is obtained and the donor site is repaired with a layered closure. Sometimes a local skin flap or split-thickness graft is required to close the donor defect. Defatting the graft requires meticulous technique, patience, sharp scissors, and adequate lighting. The graft should be frequently moistened with saline to prevent desiccation. Once the fat is removed, the dermis may be thinned as to sculpt the graft thickness to match the surrounding defect thickness. If the graft is placed at the same time of tumor or scar removal, little donor site preparation is required. Absolute hemostasis must be obtained and any devitalized tissue should be removed. Once the recipient bed is prepared, the moistened graft is placed over the bed. The graft is aligned into position. All wrinkles or folds should be straightened. The graft is then trimmed and tailored to the defect. The graft edges must proximate the recipient bed margin exactly. If not, a suboptimal result will occur.
Precise suturing technique is required for full-thickness grafts. Initially “tacking” interrupted sutures may be placed to hold the graft in position at key anchoring points. Then, interrupted or simple running sutures may complete graft placement. The sutures may be placed directly into the graft margin as a tacking suture or a few millimeters away from the graft edge. The graft must be secured and protected from the outside environment. The dressing should prevent shearing forces from disturbing the graft and firmly hold the graft against the recipient bed to reduce the potential for hematoma and seroma formation. The graft is immediately covered with a thin layer of antibiotic ointment followed by a nonstick contact layer. Sterile cotton balls are moistened in saline or Betadine and placed over the contact layer.
Specific instructions for postoperative care should be reviewed with each patient. Removal of a dressing is done in 5 to 7 days. Grafts take time to mature. Thus, the initial cosmetic appearance may be discolored and have contour irregularity. Reviewing the graft’s color and contour and the future expectations of the patient is essential. Initially grafts may be pink, reddish blue, or dusky. Darker colors may indicate superficial epidermal and dermal loss. However, the deeper papillary and reticular dermis may be viable. Full-thickness loss of graft may be indicated by necrotic black tissue.
Placement of a graft immediately after soft-tissue surgery may not be possible if exposed bone or cartilage is present. The intact undisturbed perichondrium or periosteum must be in place to supply vascularity to the graft. If an exposed cartilage or bone exists, one may delay grafting until sufficient granulation tissue covers the exposed cartilage or bony surface. This may take 2 weeks or longer, depending upon the size of the exposed surface.
Complications
Bleeding is a postoperative complication that must be evaluated immediately. If active bleeding exists, the graft should be taken off and hemostasis accomplished. This may require suture, spot electrodesiccation, pressure, liquid thrombin. Milia and cyst formation are frequently seen and are treated with simple incision and drainage. Graft hypertrophy is managed with massage and intralesional steroids. Contour irregularity may be improved with spot dermabrasion of the graft and the immediate surrounding area. Pigmentation, scaling, and erythema may be concealed with cosmetics. Graft contraction may be improved with massage or if marked may require revision and placement of a second graft.
Flap surgery
Flaps differ from grafts in that they maintain their blood supply as they are moved. The pedicle connects the flap to the surrounding tissue; it is also called the base of the flap. Abundant dermal and subdermal plexus allow for predictable elevation of random cutaneous flaps. A cutaneous flap may also have its arterial supply based on a dominant artery in the subcutaneous layer. Survival of the flap is dependent upon blood flow across the flap. Placement and size of the base must take into account local arterial blood flow into the flap as well as venous and lymphatic drainage.
Because local flaps provide their own blood supply, they are particularly useful in patients with compromised recipient sites such as those that have been irradiated.
The recovery of sensory nerve function in facial flaps is dependent on the intimacy of contact between the flap and the recipient bed and on the viability of the type of restoration.
Classification
There are many methods described for classifying cutaneous flaps: by the arrangement of their blood supply, their configuration, location, tissue content, and method of transferring the flap.
By location, flaps may be classified as local, distant, or free flaps. Local flaps imply use of tissue adjacent to the defect (from the same or an adjacent cosmetic unit). A great advantage of local tissue transfer is that the tissue closely resembles the missing skin in color and texture. These flaps can be rotated, advanced, or transposed into a tissue defect. Regional tissue can also be recruited to repair facial defects. Distant flaps are harvested from different parts of the body. Because the skin of the flap is transposed over intervening skin of one or more cosmetic units, these flaps are executed in two or more stages. After a local blood supply is developed in the flap, the pedicle is severed and returned to its initial site. Free flaps represent a combination of characteristics between flaps and grafts. They are excised at a distant site along with a major artery and completely severed from the skin as in harvesting a graft. The free skin is then sewn into the primary defect anastomosing the artery to a major artery in the surrounding skin. The transplanted skin thus carries its own blood supply analogous to flaps.
Flaps may also be classified according to their blood supply. These include random pattern, axial pattern, and pedicle flaps. Axial pattern flaps are based on a major artery, that is oriented longitudinally along the flap axis. Their advantage is that of a more secure blood supply. This allows the sur geon to harvest larger flaps with smaller width/length ratios. Random pattern flaps are supplied by the dermal and subdermal plexus alone and are not based on any specific artery. They are most successful in richly vascularized regions, particularly the head and neck, or when small flaps are performed in other areas. Because of the lack of a defined blood supply, there are restrictions on the size of the flap and on the width/length ratios considered safe for optimum flap survival. Pedicle flaps are supplied by large named arteries that supply the skin paddle through muscular perforating vessels.
Flaps are often referred to by their geometric configuration. Examples of these flaps include bilobed, rhombic, and Z-plasty (Fig. 16.30).

Fig. 16.30. Z-plasty by Limberg
The layers of tissue contained within the flap can also be used to classify a flap. Cutaneous flap refers to those flaps that contain the skin only. When other layers are incorporated into the flap they are classified accordingly. Examples include myocutaneous and fasciocutanous flaps.
A final classification is based on the type of flap movement. Advancement flaps are mobilized along a linear axis toward the defect and are slid in a linear fashion from adjacent skin into the primary defect. Rotation flaps are slid in an arcuate manner into the surgical defect. Although most flaps are moved by a combination of rotation and advancement into the defect, the major mechanism of tissue transfer is used to classify a given flap. Transposition flaps are cut, elevated, and rotated over an incomplete bridge of skin into the defect. Interposition flaps differ from transposition flaps in that the incomplete bridge of adjacent skin is also elevated and mobilized. An example of an interposition flap is a Z-plasty. Interpolated flaps are those flaps that are mobilized either over or beneath a complete bridge of intact skin via a pedicle. These flaps often require a secondary surgery for pedicle division. The first stage moves tissue into the primary defect, with the relatively bulky pedicle spanning over normal skin. In 3 to 4 weeks, an adequate local blood supply develops in the flap tip, and the pedicle is severed and discarded or replaced to its original position. Microvascular free tissue transfer from a different part of the body relies on reanastomosis of the vascular pedicle.
There are many options for reconstructing facial defects. Often the optimal method is not readily apparent. A stepwise approach can be helpful in selecting and designing a flap. The characteristics of the defect and adjacent tissue must be analyzed. These include color, elasticity, and texture of the missing tissue. The defect size, depth, and location are evaluated as well as the availability and characteristics of adjacent or regional tissue. It is important to determine the mobility of adjacent structures and to identify those anatomic landmarks that must not be distorted. The orientation of the RSTLs and esthetic units should by analyzed closely.
Potential flap designs should be drawn on the skin surface being careful to avoid those designs that obliterate or distort anatomic landmarks. The final location of the resultant scar should be anticipated by previsualizing suture lines and choosing flaps that place the lines in normal creases.
The secondary defect that is created as the tissue is transferred into the primary defect must be able to be closed easily. When designing a flap, it is important to avoid secondary deformities that distort important facial landmarks or affect function. Avoid obliterating critical anatomic lines that are essential for normal function and appearance.
Proper surgical technique involves gentle handling of the tissue by grasping the skin margins with skin hooks or fine-toothed tissue forceps. Avoid traumatizing the vascular supply by twisting or kinking the base of the flap. Deep sutures minimize tension on the flap and eliminate dead space. Excessive tension on the flap may decrease blood flow and cause flap necrosis.
Usage of different flap types for facial reconstruction
Advancement flaps are sliding flaps. They have a linear configuration and are advanced into the defect along a single vector. They limit wound tension to a single vector with minimal perpendicular tension. These flaps can be single or double. For random pattern advancement flaps, an adequate pedicle must be maintained to ensure the blood supply to the distal flap tip. In general, a 3:1 length/width ratio is considered safe. In areas of rich vascular supply, such as the helix of the ear or nasal dorsum, 4:1 length/width ratios are safely achieved.
Advancement flaps are created by parallel incisions approximately with the width of the defect. Once designed and cut, the flap is undermined in a mid-subcutaneous fatty plane. Enough fat must be maintained to protect the blood supply and fill the defect but not so much as to create a bulky appearance. Standing cutaneous deformities (“dog ears”) are usually created and are managed with excision. Advancement flaps are most useful in areas of good tissue extensibility and elasticity and the resulting incision lines can be hidden in natural creases. These include the cheek, preauricular region, lips, and chin. They are also indicated in areas of pronounced linear skin tension lines or cosmetic borders. They are often helpful in reconstructing defects involving the forehead, helical rim, lips, and cheek The forehead, nasal dorsum, and helix of the ear represent such sites.
Intraoral uses of advancement flaps include covering oroantral fistulas and alveolar clefts. A disadvantage of buccal advancement flaps is the decrease in vestibular sulcus depth.
The rotation flap is also a sliding flap that is pulled into the position across the primary defect. They have a curvilinear configuration so the design of a rotation flap is slightly more complex than that of an advancement flap. As with all random pattern flaps, survival of a rotation flap depends in part on the adequacy of its pedicle. Another important consideration, however, is that the degree of force of the secondary motion is inversely proportional to the flap/defect size ratio. For these two reasons, rotation flaps tend to be large, particularly around free margins. In areas of lesser tissue extensibility they must also be cut large, such as on the forehead, scalp, or dorsal hands. These flaps are usually random in their vascularity but may be axial. The flap/defect size ratio should be 3:1 or 4:1 to ensure adequate blood supply across the pedicle and to limit stresses due to secondary motion.
The flap should be cut and undermined. The undermining is carried beyond the base of the flap and around the edges of the flap and the primary defect for 1 to 2 cm. The key suture is placed through the center of the leading edge of the flap and is anchored into the far edge of the primary defect, thus pulling the flap across the defect and closing.
Rotation flaps are most useful in areas with arcuate cosmetic borders or arcing skin tension lines. These include the lateral forehead/temple regions, cheeks, upper lip, and chin (Fig. 16.31). They are most easily employed in more elastic skin as they are pulling-type flaps. However, they are also useful in regions with very inelastic, nonextensible skin such as the scalp, nasal dorsum, and dorsal hands. To reconstruct a scalp defects one or more rotation flaps can be used. Because of the relative inelasticity of the scalp tissue, these flaps must be large relative to the size of the defect.

Fig. 16.31. Rotation flap
Transposition flaps are conceptually the most difficult of this group to design and execute. These flaps are rotated and advanced over adjacent skin to close a defect. However, these efficient flaps offer a number of advantages to the surgeon performing facial repair. Transposition flaps are small compared to advancement and rotation flaps, generally equaling the size of the defect. They are usually designed so that one border of the flap is also a border of the defect. These flaps are advantageous in areas where it is desired to transfer the tension away from closure of the primary defect and into the repair of the secondary defect. They are pushed rather than pulled into the defect, which allows them to drape into place. They are ideal for use around free margins such as nasal alar rims and lower eyelids. The example of transposition flap is a traditional rhombic flap. The rhombic flap is a precise geometric flap that is useful for many defects of the face. The traditional rhombic (“Limberg”) flap is designed with 60 and 120° angles and equal-length sides. The angle of the leading edge of the rhombic flap is approximately 120° but may vary.
Interpolation Flaps. Interpolation flaps contain a pedicle that must pass over or under intact intervening tissue. A disadvantage of these types of flaps is that for those passing over bridging skin, the pedicle must be detached during a second surgical procedure. Occasionally it is possible to perform a single-stage procedure by deepithelializing the pedicle and passing it under the intervening skin. Advantages of interpolation flaps include their excellent vascularity, and also their skin color and texture match.
The forehead flap (median and paramedian) is a commonly used interpolation flap used for large nasal defects. The nasolabial flap is useful for reconstructing defects involving the oral cavity and those involving the lower third of the nose. It can be used as an interpolation flap with either a single or staged technique. The lip-switch flap (Abbe) can be taken from either lip, but it is most commonly switched from the lower to the upper lip. This flap can be used to reconstruct as much as one-third of the upper lip. The labial artery supplies the flap and should be maintained with a small cuff of subcutaneous tissue and muscle surrounding the vascular pedicle. The pedicle is divided after approximately 2 to 3 weeks.
For large facial defects, local flaps may not provide sufficient tissue to adequately restore the missing tissue. In these cases consideration should be given to using a regional flap.
Regional flaps are defined as those that are located near a defect but are not in the immediate proximity. They are frequently harvested from the neck, chest, or axilla and can provide coverage of large surface areas on the face. Selection of a specific regional flap depends on the size and location of the defect and also on the properties of the flap. Advantages of regional flaps include the large amount of soft tissue and skin available. Disadvantages of these types of flaps include poor color and texture match, excessive bulkiness of the flap, and donor site morbidity.
Alternatively distant flaps can be used. The most frequently used technique is a tubed pedicle flap or Filatov’s graft. In this flap the sides of the pedicle are sutured together to create a tube, with the entire surface covered by skin. The tube pedicle was developed by Vladimir Petrovich Filatov in Odessa, between 1916 and 1917. A tube pedicle is a flap of skin sewn down its long edges, with one end left attached to the site of origin, the other is attached to the site to be grafted.
The procedure begins with the lifting of a long, large flap of skin by making a roughly “U” shaped incision. The rounded end of the flap is cut to shape to fit the area to be repaired. The long edges of the skin flap are stitched together to form a tube to prevent drying out and infection of the raw side of the skin flap. The shaped end of the tube is then attached to the site to be repaired whilst the other end of the tube remains attached to its site of origin. After a number of weeks, the tube is cut near the area to be repaired leaving enough skin on the graft site to shape and model. The remainder of the tube can once again be opened and returned to its original position. On occasion, multiple tubes might be taken to rebuild substantial parts of the face or body.
Tissue must be taken from distant parts of the body in stages. For example a tube might be taken from the stomach area and attached to the wrist. After a number of weeks the tube would be disconnected from the stomach, the arm raised and the loose end of the tube attached to the site on the face to be repaired. Once again after a number of weeks the tube is disconnected from the wrist and this loose end of the tube is attached to another part of the face. Only then can the tube be opened and modelled to the face. Any mature tubed flap, in comparison with other sophisticated flaps, is suitable for the meticulous detailed modelling that is particularly important in face reconstruction.
Many things must be considered to ensure a functionally and cosmetically successful flap surgery. Cosmetic units and borders, skin tension lines, blood and lymphatic flow, tissue elasticity, and local anatomy all play roles in the final appearance of a flap along with technical execution.
One should always consider several flaps when planning any closure, working through the advantages and disadvantages of each. Variations in local anatomy, defect size and depth, available tissue, prior surgeries, and patient factors such as smoking or diabetes may impact the appropriateness of a given flap in a given patient. The proper respect for the complexity of flap surgery and associated risks must be maintained. Technical skills must be supported by knowledge of the basic science relative to skin anatomy and physiology, wound healing, and complications. Factors particular to the individual patient must be considered for each procedure. Only then can we satisfy the requirements of qualified flap surgeons as demanded by our patients and peers.
Complications of the flap surgery
Postoperative complications can be minimized with careful preoperative planning of flap design and by early recognition of problems.
A medical history can be used to identify patients with risk factors involving small vessels. These risk factors include smoking, diabetes, hypertension, previous radiation, and pre-existing scars. Flap survival depends on early recognition of flap compromise. Ischemia is defined as an inadequacy of perfusion in providing tissue needs. Signs of arterial ischemia include a pale and cool flap that does not blanch with pressure and typically does not bleed with a pinprick. Flaps are somewhat ischemic initially because the original tissue perfusion has been compromised by flap elevation. Most tissue can survive on 10 % of its average blood flow.
Whether the flap will undergo necrosis depends on patient-related and surgery-related factors that influence the risk of necrosis in facial flaps. Smoking is associated with an increased risk of flap failure. Patients should be advised to quit smoking during the perioperative period.
Hyperbaric oxygen (HBO) has been shown to be beneficial in improving the vascularity of marginal tissues.
Prophylactic HBO therapy in cutaneous flap surgery in the irradiated tissue bed may be particularly helpful to combat the hypoxia and hypocellularity. Tissue oxygenation is an important factor in prevention of wound infection and is closely related to blood supply. Infections involving local flaps may result in flap failure or poor cosmetic outcome secondary to wound dehiscence and scarring.
Reconstruction of lips
The lips are multifunctional folds of skin, mucosa, and muscle which consist of many small cosmetic subunits and naturally occurring landmarks. The upper lip is composed of three cutaneous subunits and the upper vermilion. The two lateral cutaneous subunits of the upper lip are bounded superiorly by the nose, laterally by the nasolabial folds, and medially by the philtral crests.
There are two philtral columns along the midline of the upper lip. Between the philtral columns, a philtral groove or dimple should be present. The philtrum is the central cutaneous subunit of the upper lip. Just inferior to the philtral groove should lie the symmetric Cupid’s bow that follows the vermilion border of the upper lip in the midline. The sole cutaneous component of the lower lip is bounded laterally by the inferior extension of the nasolabial fold and inferiorly by the labiomental crease. The lateral commissure at the angles of the mouth separates the upper and lower lips. Both the right and left commissures should be symmetric in repose.
Because there are no bony or cartilaginous supporting structures, the lips are capable of a wide range of motion and a multitude of functions. A competent oral aperture contributes to proper deglutition, verbal and nonverbal communication, oral continence, and maintenance of a stable intraoral milieu. Thus, it is extremely important to consider functional integrity as well as the aesthetic outcome when planning reconstruction of defects involving the lip and perioral tissue. The lips should be examined from the facial and profile view where symmetry and balance are important. Obvious deformities such as clefts, scars, lesions, and asymmetric regions should be documented.
The favorable lines of closure lie within the relaxed skin tension lines, which are created by the cutaneous tension from the underlying facial musculature. In the perioral region, these lines are usually perpendicular to the vermilion-cutaneous junction. If possible, optimal cosmetic results are obtained by placing the incisions along the boundaries of the cosmetic units.
The reconstructive modality of choice for repair of defects involving the lips and perioral tissue will largely depend on the location, size, and depth of the wound. Partial-thickness wounds may heal by second intention, close primarily, or need local flaps. Occasionally, skin grafting can be used for reconstruction of superficial perioral wounds. Reconstruction of full-thickness (into the oral cavity) defects usually requires more extensive tissue rearrangement such as wedge repair, switch flaps, or full-thickness local flaps.
Before undertaking any reconstructive procedure, one should clearly delineate and mark the cosmetic units and favorable lines of closure prior to local anesthesia. Reconstruction of perioral defects requires a multilayered approach, carefully approximating the mucosal, submucosal, muscular, and subcutaneous tissues, followed by realignment and eversion of the vermilion border and cutaneous tissue.
Most of the partial-thickness wounds are repaired with local flaps, while second intention wound healing and skin grafting are less commonly used. Because the lips have no bony attachment, the free margin of the lip may be unfavorably displaced during normal scar contracture, resulting in an incompetent oral aperture.
Skin grafts in the perioral region have a greater tendency to heal with a convex contour than elsewhere, and thus they are rarely used for lip repair. However, in certain defects, if the size and location of the wound are unfavorable for flap reconstruction it requires skin grafting to minimize functional and cosmetic distortion of the lip. Local skin flaps provide the most useful and diverse approach to achieving optimal cosmetic results in lips reconstruction.
Large defects on the cutaneous portion of the lips are reconstructed with a more complex variation of the advancement flap. Complex advancement flaps require extensive undermining to release the redundant tissue of the lateral lip and cheek. A releasing incision is commonly made at the lateral aspect of the defect, along the vermilion-cutaneous junction. Because of the lateral tissue availability, there is usually only minimal displacement of the philtrum.
Rotation flaps are rarely used to repair the defects of the perioral tissue because it is difficult to place the incisions within the normal relaxed skin tension lines.
Transposition flaps are extremely useful in mobilizing local tissue on many areas of the face, especially the nose. Depending upon the size and location of the wound, the transposition flap can be inferiorly or superiorly based to harvest excess tissue from the nasolabial fold.
Complex wounds which involve several cosmetic subunits may require a combination of surgical techniques for adequate reconstruction.
Full-thickness wounds of the lips and perioral tissue extend through the mucosa into the oral cavity. Usually, full-thickness lip defects of the upper lip which are less than one-third of the vermilion length (1.5 to 2 cm) can be closed primarily in a wedgelike fashion. Various modifications of the wedge closure may be helpful to achieve optimal functional and cosmetic results. Full-thickness defects greater than one-third of the vermilion length usually require more extensive tissue rearrangement. The Abbe flap is a fullthickness, lip-switch flap which is pedicled on the labial artery. These flaps are created by incising a wedge of tissue from the lip opposite the defect and rotating the full-thickness flap on its vascular pedicle into the defect. Once collateral circulation has been established (approximately 2 to 3 weeks), the pedicle is transected and the vermilion is carefully realigned.
For defects greater than one-half of the vermilion length, recruitment of large amounts of local tissue may require unilateral or bilateral cheiloplasty followed by medial advancement of the cheek tissue.
Immediately following wound repair, an antibiotic ointment is applied to the incision and the wound is covered with a simple pressure dressing. It is extremely important to stress that the patient should minimize use of his or her lips, including chewing, talking, laughing, smiling, or frowning. Liquids and small bites of soft foods are highly recommended postoperatively. The cutaneous sutures are usually removed at 5 to 7 days postoperalively. Prophylactic antibiotics are routinely used after reconstruction.
Reconstruction of the nasal defects
The nose is a respiratory and olfactory organ made up of skin and muscle overlying a skeleton of bone and cartilage which is lined with mucosa. Its midline position is best examined in the frontal view, and its anterior projection from the profile view. The nose is examined in relation to the forehead, orbital rims, eyes, maxilla, lips, and chin. Examination of the nose should include inspection from the lateral, frontal, and submental vertex views, as well as a complete intranasal examination. The proximal third of the nose is supported by the paired nasal bones. The skin of the upper nose is usually elastic and easily undermined. The underlying bony rigidity resists distortion and contributes to the successful outcome of many skin flaps on the upper nose. The middle third is supported by the upper lateral nasal cartilages. The distal third is supported by the lower lateral cartilages medially and the sesamoid cartilages and dermis laterally.
The nasal septum provides support for both aesthetics and function by separating the bony and cartilaginous vault of the nose. The nasal septum also aids airflow and supports the tip and columella. The mobile portion of the nose includes the membranous septum, columella, and lobule, which contains the tip and alae. Each alar cartilage is shaped like a wishbone, with the apex supporting one side of the nasal tip. The nasal cartilages are highly mobile and do not resist distortion well.
Although nasal reconstruction is an ancient art, the complexities of nasal anatomy and physiology continue to make the repair of nasal defects one of the most challenging aspects of reconstructive surgery.
There are no simple guidelines to nasal reconstruction, although a number of approaches to management, reconstructive algorithms, and classifications of nasal defects have been proposed. However, one reasonable approach to the repair of soft-tissue defects is to consider more conservative options first. Superficial wounds and wounds in certain anatomic areas may heal naturally with excellent cosmetic results, and direct primary closure often works well on the upper nose. Full-thickness skin graft repair often works well for nasal defects with an adequate subcutaneous bed, although the skin color and texture match may be poor. In general, local skin flaps offer a superior color and texture match for nasal skin and are the repairs of choice for deep nasal defects. Penetrating defects may require reconstruction of the nasal lining and provision of structural support.
Full-thickness skin grafts usually offer a better color and texture match than the best split-thickness graft and have less tendency to contract. They may be used to repair superficial nasal defects, either immediately or following a period of secondary intention during which the wound will contract and granulation tissue will begin to fill deep defects, possibly enhancing graft viability.
Composite grafts, which consist of skin and other structures and include combinations of skin and fat, skin and perichondrium, and skin and cartilage, may be used to repair deep defects of the lower nose, columella, and alar free margin. The auricular helix, conchal bowl, and lobe are the most common donor sites, and the donor defect can be closed in a variety of ways.
Free cartilage grafts can be used to provide structural support for skin flaps and are most commonly harvested from the nasal septum, conchal bowl, auricular rim, and occasionally from costal cartilage. Cartilage grafts can be placed within nasolabial or forehead flaps, or a composite graft of skin, perichondrium, and cartilage may be used. Free cartilage grafts require highly vascular tissue beds to ensure their survival.
A large number of skin flaps have been described for the repair of nasal defects. The majority are harvested in the upper nose, adjacent cheek, nasolabial fold, and the forehead. Surgical undermining is relatively simple on the upper nose and becomes increasingly more difficult toward the nasal tip. Undermining is usually performed below the muscles of the upper nose and above the perichondrium or periosteum in order to prevent vascular injury (Fig. 16.32; 16.33).

Fig. 16.32. Nasal reconstruction by rotation flap (a, b, c, d)
Partial or total nasal prostheses may be of value in both cosmetic and functional rehabilitation. Severe trauma and extensive nasal tumors may be treated by total rhinectomy and the permanent use of a prosthetic nose. Alternatively, a prosthesis can be used if delayed reconstruction is planned. An accurate color match is essential and requires the services of an expert prosthetist. Patients must be able to clean and apply the prosthesis, which may be retained in place by a combination of adhesives and appliances such as those used for spectacles or dentures.
Major nasal defects can involve the loss of any combination of skin, mucosa, and structural support; each of the lost nasal structures needs to be replaced, Any such repair is likely to be followed by flap contraction due to granulation of the undersurface of the flap. Defects of nasal mucosa or structural support must be repaired prior to replacing the missing skin. Reconstruction of the nasal lining may involve split- or full-thickness skin grafts. Free mucosal grafts harvested from the buccal mucosa can be also used. A nasolabial or reverse nasolabial flap can be used to replace lost nasal lining with cheek skin. Pivoted mucosal flaps can be raised from intranasal donor sites (vestibule, vault, and septum). These flaps are thin and yet provide highly vascular beds for free bone or cartilage grafts.
Reconstruction of missing nasal bone or cartilage is required to support skin flaps, maintain a normal nasal shape, and prevent nasal collapse. Support can be provided in a number of ways. A skin-cartilage composite graft together with a cutaneous flap can be used. Cartilage grafts may be placed within folded nasolabial flaps in the reconstruction of the nasal ala. Alternatively, cartilage or bone grafts can be buried beneath the tips of planned nasolabial or forehead flaps, and sometime later they are transferred to the nasal defect as an integral part of the flap. Sculpted bone or cartilage grafts can be assembled on a highly vascular, pivoted septal mucosal flap and covered with a thin forehead flap Cartilage grafts can be inserted into skin flaps as a secondary procedure after the flaps have been allowed to establish a local blood supply, although the results may be inferior to the primary placement of the cartilage. Structural support of the upper nose and dorsum can be provided by skeletal rib or iliac crest cantilever bone grafts anchored to the nasal process of the frontal bone and covered with a forehead flap.
Esthetic surgery of the face
Modern society raises conditions to our appearance. Word “beauty” is becoming synonymous of success, sexuality and healthy. A beauty person have more chances in professional, social and biological realization. That is why every year necessity in plastic surgery procedures increases between individuals.
Esthetic face surgery is aimed to achieve harmony of the face appearance, elimination of pathological aging changes of the soft and hard tissues.
Ecological environment, harmful habits, insolation, bad dietary, genetic predisposal and stresses are factors that cause premature aging.
The first feature of aging process in the skin and subdermal layer is the decreasing of the concentration of hyaluronic acid, ptosis of tissues and decreased tone of the skin.
From 25 years of age the reduction of the quantity of hyaluronic acid in the skin and subdermal layer begins.
Aging changes in face appearance: wrinkles, fat herniation eyelids, rounding the eyes, skeletonizing orbits, deep nasolabial folds, Crown’s feet, thinning lips, hanging nose tip, ptosis of skin and fat, squaring of the face, platysma banding, dropping mouth corners.
Facial rejuvenation procedures:
- injection techniques (botulinum toxin injections, fillers, biorevitalization);
- blepharoplasty;
- browlift;
- extended SMAS facelift and neck lift.
Injections of botulinotoxin are used for eliminating mimic wrinkles of forehead, glabella region, lateral orbital region (Crown’s feet), nose, upper lip, corners of the mouth. Clostridium botulinum was first identified in 1897, in Belgium, by Professor Emile van Ermengem who was investigating fatal cases of food poisoning following the consumption of macerated ham.
During the Word War II research continued into this potent neurotoxin as a possible agent (“agent X”) for biological warfare. Dr Alan Scott performed first clinical tests of usage of botulinum toxin A on humans for treatment of strabismus in 1978. Then, botulinum toxin A was used for treatment of blepharospasm, hemifacial spasm, cervical distonia and its rejuvenating effect was also noticed.
Botulinum toxin induces paralysis by blocking the release of acetylcholine at the skeletal neuromuscular junction, thereby inhibiting the transmission of nerve impulses across the synaptic junction to the motor end plate.
Standart zones of botulinum toxin injections for wrinkles treatment: glabellas’ region, horizontal wrinkles of the forehead, Crow’s feet, mouth corners, platysma banding, “turkey” neck bundles.

Fig. 16.34. Points of botulinum toxin injections:
1 – forehead horizontal wrinkles;
2, 3 – glabella region;
4 – periorbital region (Crow’s feet);
5 – oblique wrinkles of the nose;
6 – for dropping mouth corners
Injection techniques are also used for filling wrinkles and flattening the surface of the skin. This method is called contour plastics, it also used for augmentation of lips, malar eminences, and correction of tissue loss. For these purposes are used resorbable materials, such as collagen, hyaluronic acid, agarose, fat, and permanent materials – silicone, acrylamide gel, tephlon and others. Preference is given to resorbable materials. Typical zones of usage are glabellas vertical wrinkles, nasolabial folds, horizontal wrinkles of the forehead, dropping mouth corners, periorbital region (Crow’s feet) and others.
Standard surgical procedures for face rejuvenation are blepharoplasty, browlift, facelifting (Fig. 16.35).

Fig. 16.35. Surgical procedures for face rejuvenation:
1 – upper blepharoplasty – scar hides into upper palpebral crease;
making it almost invisible;
2 – zones of herniated fat removal;
3 – lower blepharoplasty – scar lies under lashes, it becomes invisible after few months; 4 – lines of tissue tension during facelifting procedure;
5 – cosmetic incision line used for facelifting procedure
Method of blepharoplasty is based on excision of excess of skin and removal of herniated fat of the lower and upper eyelids (Fig. 16. 36). It is the most frequently performed cosmetic surgical procedure.

Fig. 16.36. Method of the upper (a, b) and lower (c, d, e) blepharoplasty y Kruchinskiy
Endoscopic browlift allows raising brows and forehead using only small incisions hidden on the hearbearing zone of the head.
After endoscopic forehead periosteum transsection and detaching of the depressor muscles 10–12 suspension sutures are placed for fixation of the forehead on its new position.
Facelifting procedures (Fig. 16.37) – extended SMAS facelift and neck lift. Incision of the skin performed in temporal hierbearing region, descends in the preauricular area & then hides in the postauricular area. Subcutaneus undermining performed to the vertical line drawn through the lateral corner of the eye. Malar fat pad and cheek fat are pushed upward and backward by several sutures, fixed to temporal fascia and fascia parotideamassetterica. The superficial muscle aponeurose system of the face (SMAS) has to be pushed upwards and backwards, excess of fascia parotideamassetterica is excised and refixed by sutures. Then excess of the skin is removed and cosmetic sutures are applied on skin edges.

Fig. 16.37. Scheme of the facelift by the method of Rauer – Michelson
Microsurgery of the maxilla-facial area
Microsurgery – the highest level of surgical technique. This technique involves the use of special equipment and facilities and opens up entirely new opportunities in every field of surgery. This line of surgery involves the use of intraoperative magnification (surgical microscope), as well as microinstruments for surgical interventions on the very small structures of organism.
The main areas of microsurgery, the following:
- Emergency operations – replantation of lost limbs.
- Damage to peripheral nerves of different origin.
- Tendon suture.
- Surgery on the face, including allotransplantation large tissue fragments with the restoration of the innervation and blood supply (“face transplant”). This kind of operation was firs presented by Professor Bernard Devauchelle in 2005 (Fig. 16.38–16.41).
- Transplant tissue complexes with the restoration of blood supply.

Fig. 16.38. Patient with traumatic disfigurement of the face (dog bite) defect of nose, right chic, lips, chin

Fig. 16.39. Scheme of tissue block including oral and nasal mucosa, nose cartilages, mimic muscles, skin of the lips, nose, cheek and chin, nutritive arteries, veins, motor and sensitive nerves

Fig.16.40. Allotransplant was taken accordingly to preoperative planning

Fig. 16.41. Patient’s face appearance with microsurgical allotransplantation of the face after 4 years
Microsurgery techniques allow the transfer of tissues for reconstruction from one area of the body to the other. A wider range of donor sites is available, very large flaps can be transferred, and a multiplicity of tissues can be included in the flap for an optimal functional reconstruction. Microsurgical tissue block transplantation is more effective procedure than free tissue grafting in cases when recipient zone is compromised – irradiated in oncologic patients, cicatricated after inflammatory processes or burn injury.
The development of microsurgical free tissue transfer resulted in a dramatic evolution in head and neck reconstruction, allowing for a significant increase in the available choices of anatomic and functional rehabilitation. The first surgical microscope was built by Dr. Carl Nylen, a Swedish otolaryngologist who used it for the first time in 1921. In the late 1950s and early 1960s Jacobson and Suarez performed successful anastomosis of carotid arteries in dogs and rabbits with a 100 % patency rate. When Jacobson presented the outcome of his research at a national meeting, a leading surgeon at a prestigious institution stated in front of the audience, “This is very nice work, but it is simply ridiculous to bring a microscope into the operating room.” During the 1960s microsurgery was promoted by neurosurgeons and plastic surgeons with encouraging results. In 1973, there was established the first department of microsurgery in Moscow, Research Institution for Clinic and Experimental Surgery under Ministry of Health. Similar clinics have been organized in Leningrad, Kiev and Tbilisi. In 1975 Taylor and colleagues described the free fibula flap, while Hidalgo applied the technique for mandibular reconstruction in 1989. In 1981 Yang developed the radial forearm flap, while Soutar and colleagues popularized the technique for intraoral reconstruction with and without the addition of a portion of the radius in the mid-1980s. In 1978 Taylor described the transfer of the iliac crest as an osteomyocutaneous flap based on the blood supply from the circumflex artery and vein. Free flaps became popular in the head and neck region due to the ability to transfer vascularized bone and soft tissue in one stage at the time of the resection, with predictable high success rates.
The microsurgery instruments require the following specifications. Their weight must not exceed 15 to 20 g. They must be at least 10 cm long so that they lie loosely in the hand. The closing pressure of some instruments such as forceps or scissors should lie between 50 and 60 g. Tremor increases with higher closing pressure. The vascular clamps must exert an evenly distributed pressure over the whole length of the jaw of the clamp. The jaws must lie parallel with each other. Microscissors should have an opening of less than 4 mm. They can be either straight or curved, but it is imperative that they cut tissue in a clean fashion in order to reduce the risk of a thrombosis in a vascular anastomosis or the formation of a neuroma in a crushed nerve. A magnification of 10 is usually enough for anastomosis. During surgical interventions surgeons needed support for hands and special work places (chair), as part of the operation lasting many hours. Therefore, there exists the need for more comfort for the body during surgery.
Prior to undertaking a microsurgical procedure skills should be learned in the laboratory on experimental animals. The laboratory should include an operating microscope, microinstruments, and animals for practice. Several manuals exist for the graded exercises necessary for acquiring microsurgical skills. Before presuming to do this surgery in the operating room, surgeon patency rate in the laboratory should exceed 99 per cent in 1-mm vessels, such as rat femoral vessels.
During transplantation composite flap with the resumption of blood supply may be different options for applying microvascular anastomoses. In head and neck surgery both end-to-end and end-to-side anastomoses are used for the artery and vein. Suitable recipient vessels, such as superior thyroid or facial vessels, are dissected. The venous anastomosis is done before the arterial anastomosis, and the clamps are released simultaneously after completion of both. The donor and recipient arteries are prepared by carefully dissecting the adventitial layers. For end-to-end anastomosis, the vessels are placed in a clamp approximator, gently dilated, and irrigated with heparin solution (Fig. 16.42).

Fig. 16.42. A technique of microsurgery suturing (a, b, c, d, e)
The suture (usually 9–0) is passed at a distance from the margin of the vessel similar to that of the thickness of the wall. It is recommended to apply a counterforce while passing the needle through the vessel by holding the forceps open inside the lumen instead of grasping the vessel wall which may damage the edge of the vascular structure. After the suture has passed through both ends of the vessel, a small “tail” of 2 to 3 mm is left in order that the knot can be performed while seeing the suture end within the field of the surgical microscope.
After the first suture is placed the second suture is usually placed 180° from the first. The third suture is placed in between the first and the second, and two more interrupted sutures are placed on the same side. After finishing one side the vascular clamps are turned to expose the other side of the anastomosis. The sutures should always be at the same distance as the edges of the vessel as well as the same distance between each one of the sutures.
When the vascular anastomosis cannot be performed “end-to-end” due to very significant differences in the diameter of the lumen, an “end-to-side” anastomosis is a viable alternative. An oval excision of the wall of the large-diameter artery is performed, and the sutures are executed in a similar fashion as explained in the end-to-end anastomosis. After the anterior sutures are placed, the clamp is turned over, and the posterior sutures are placed. The clamps are released and a patency test is performed. For end-to-end anastomosis, an opening equal to the diameter of the smaller vessel is made in the larger vessel. The arteriotomy should be made by resecting a small lenticular piece of the arterial wall; the venotomy may be made as a simple slit. The initial sutures are placed 180° apart at the “heel and toe.” The two walls are then completed. A mattress suture facilitates eversion of the vein. The patient is anticoagulated with a single bolus of heparin prior to clamping and maintained on low molecular weight dextran thereafter for the first postoperative week.
The benefits of a free flap should be weighed against the risks of a prolonged operative procedure and the greater risk of flap failure from anastomotic thrombosis.
The probability of thrombosis depends on the quality of the vascular suture, hemodynamic disorders in the area of the anastomosis due to the turbulent blood flow, vascular spasm, the maximum linear rate of blood flow, the ratio of blood coagulation and anticoagulation system. In this possibility of anastomoses evaluated clinically, visualy, instrumentally and using angiography. Anesthetic maintenance of microsurgical operations has a number of features, because sometimes they can last up to 46.5 hours. In this case, the patient should be immobilized, and the anesthesia occur with a stable blood pressure. Output from anesthesia should proceed without vascular spasm, which is important to ensure consistency created anastomosises, as well as for high-quality restoration of circulation in the transferred tissues.
If you need to ensure reinervation of tissues one could used stapling nerve or transplantation of fragments of nerve fibers. At the same time one should try to identify the bundles of functions: sensory and motor. Suture of the nerve may impose without dividing into groups of beams, split into groups of beams and divided into separate beams. Neurorrhaphy is the act of nerve suturing for both direct and gap repairs (Fig. 16.43). The trigeminal nerve is repaired using epineurial sutures. Generally, an 8–0 monofilament nonresorbable nylon suture is chosen since a resorbable material would invoke inflammation and disturb the area of anticipated neural healing. At least two sutures are used per anastomosis site to prevent rotation, but not more than three or four sutures should be used per anastomosis.

Fig. 16.43. Direct epineurial neurorrhaphy
The first suture is placed on the medial side of the anastomosis since it is more difficult to access. The epineurium is pierced with the needle of 0.5 to 1.0 mm from the edge of the nerve. The second suture is placed 180° from the first suture, and then an assessment is made regarding the need for more sutures. When neurorrhaphy is not possible without tension and a nerve gap exists, an interpositional graft must be considered for indirect neurorrhaphy. The options for autogenous nerve grafting include but are not limited to the sural nerve, the greater auricular nerve, and possibly the medial antebrachial cutaneous nerve.
The sural nerve is the preferred nerve for grafting since it most appropriately matches the nerve diameter and the fascicular number and pattern of the trigeminal nerve. Sural grafts up to 20 cm in length are possible, and patients tolerate the donor site deficit well. The greater auricular nerve is a poor choice for trigeminal repair. Patients are generally not amenable to sacrificing one facial region for another. Additionally, the small diameter of the nerve makes it useful only when used as a cable graft. The sole advantage of a greater auricular graft over a sural graft is in situations when it can be harvested via the same incision for another procedure, such as the repair of an extraoral mandibular fracture or management of pathology. The basic premise with graft repair is that the graft supplies the Schwann cells and growth factors necessary to support and encourage axonal sprouting through the graft toward the target site.
As for the structure of flaps, using for transferring (transplants), they are divided into skin-fat, skin-fascial, skin-muscle, muscle, skin and bone, etc. In this composite flap is used to restore lost functions or replace tissue defects. But the main purpose of this type of surgery is often the restore of body tissue defect with the resumption of its inherent function.
Undoubtedly the main advantage of transplantation using microsurgical technique is to restore blood flow in free transferred tissues. This process has several stages: A period of acute disorders (ischemia during transplantation, a decrease in sources of blood, the axial reorientation of the vessels, hypotension) the formation of vascular connections and the final adjustment. To succeed in this type of transplantation is necessary to ensure adequate arterial blood flow along with adequate venous outflow, a reliable contact between the graft and recipient bed, immobilization of the segment, to prevent compression of the vascular pedicle graft (vein, artery).
It is suggested a large number of different flaps for transplantation, which are used for different purposes and have different anatomical features. Thoracodorsal flap proposed by G. Maxwell (1976), incorporates the subscapular artery, the envelope of the scapular (D = 1.5–3 mm, length 8–14 cm), 2 accompanying veins, the thoraco-dorsal nerve. In this case, there are different versions allowing the flap to include in the graft: skin, muscle and bone fragments. Its advantages are the following: accessibility, ease of harvesting, large sizes – up to 43 × 16 cm, long pedicle, large caliber vessels and a slight lack of features, the ability to use a fragment of rib. The disadvantage is cosmetic defect.
Parascapulery (lower shoulder) skin-fascial flap (size – up to 15 × 30 cm) incorporates skin Parascapulery artery, the envelope of the scapular (length 4–14 cm) and a concomitant vein. Its advantages are the following: a long pedicle, large diameter feeder vessels, small thickness, which is convenient for oral and maxillofacial surgery. The external skin-fascial thoracal flap includes thoracodorsal artery (D = 2.3 mm, length 10 cm), the accompanying vein and cutaneous branch of the second intercostal nerve. This graft is characterized by up to 19 × 14 cm, small thickness, the possibility of reinnervation, the long vascular pedicle, a large defect in the vessels. Costal flap proposed R. Danice (1975) incorporates a rear intercostal neurovascular bundle and fragment edges. Deltoid flap was first proposed in 1984 I. Franklin. The flap includes a pair posterior branch of the artery, a vein of the same name and the lateral cutaneous nerve of the arm. It is characterized by a fairly large volume, large diameter vessels and the opportunity of reinervation.
The radial forearm flap is perhaps the most commonly used soft tissue microvascular flap for intraoral and oropharyngeal defects. It has gained wide acceptance because of its reliability, adaptability, ease of harvest, and the thin pliable nature of the flap. The arterial blood supply of the radial forearm fasciocutaneous flap is based on perforators of the radial artery. The venous drainage of the radial forearm flap occurs through the interconnecting superficial (cephalic vein) and deep (venae comitantes) systems. The free radial forearm fasciocutaneous flap is extremely useful in head and neck reconstruction. The flap’s reliability, adaptability, ease of harvest, and the similar character of the thin pliable skin to the lining tissues of the oral cavity make its use commonplace in modern maxillofacial reconstruction.
The fibula is ideal for large bony defects since it offers up to 25 cm of vascularized cortical bone (Fig. 16.44). The blood supply to the fibula is delivered through perforators originating in the peroneal artery which is usually between 2 and 4 mm in diameter. The venae comitantes provide the venous drainage; these are paired vessels that run along the artery. The free fibula flap can be raised with or without a skin paddle but the skin paddle had a poor prognosis. A significant limitation of the free fibula flap is the common presence of peripheral vascular disease in the lower extremities.

Fig. 16.44. Elevation of free fibula flap after the osteotomy (adapted from Serafin D)
The blood supply to the osteomyocutaneous iliac crest flap is based on the deep circumflex iliac artery and vein. This artery takes origin from the external iliac artery or femoral artery in the region of the inguinal canal. It courses a distance of about 5 to 7 cm between its origin and the anterior superior iliac spine, following thereon the inner aspect of the iliac crest. The iliac crest provides a significant segment of the bone that may reach 4 cm in height and 11 cm in length. The dimensions of the flap may allow for a reconstruction of a hemimandibulectomy or anterior mandibular defect. There are some significant advantages to the iliac crest free flap: the amount of bone available for potential reconstruction with osseointegrated implants; and the availability of a thin and broad muscle that can be left to heal by secondary epithelization intraorally. In most cases the inner aspect of the iliac crest is sufficient to reconstruct a mandibular defect, having the advantages of a less deforming defect and avoiding the lateral dissection of the gluteus medius muscles. The disadvantage of the flap is the relatively short vascular pedicle and the potential for herniation of the abdominal contents.
The rectus abdominis free flap has been used mostly for base of skull reconstruction and tongue reconstruction. It is based on two vascular pedicles: the deep superior epigastric vessels; and the deep inferior epigastric vessels, which are branches of the external iliac artery. The deep inferior epigastric vessels have a larger diameter and a longer vascular pedicle which makes them the preferred choice for anastomosis to the recipient vessels with very high reliability and success.
Other flaps have been used for oropharyngeal reconstruction, including free omentum for oral lining, gracilis muscle free flaps with the anterior obturator nerve for facial reanimation, and lateral thigh or lateral arm free flaps for pharyngeal reconstruction. Even free temporoparietal fascial flaps have been used based on the superficial temporal vessels for intraoral lining or combined with the overlying skin or underlying bone. In the treatment of ankylosis of temporomandibular joint an autograft of foot bones is used for arthroplasty.
The flaps described in the current chapter are the most commonly used in head and neck reconstruction. The ability to transfer vascularized tissues allows for a significant varietyof options.